Although point of care ultrasound examinations can be performed with the standard, full-featured ultrasound systems used by ultrasound professionals (Fig. 27.1), these relatively expensive and complicated instruments are not typically available to health care providers in the clinical setting. Fortunately, there are now a variety of smaller, less expensive, and easier to use ultrasound instruments that are well suited for point of care applications (Fig. 27.2), and some of these systems have features that approach those of the larger systems.


FIGURE 27.1. Examples of full-featured ultrasound systems. A,GE Logiq 9, photo courtesy of GE Healthcare. B,Philips iU22, photo courtesy of Philips Healthcare.
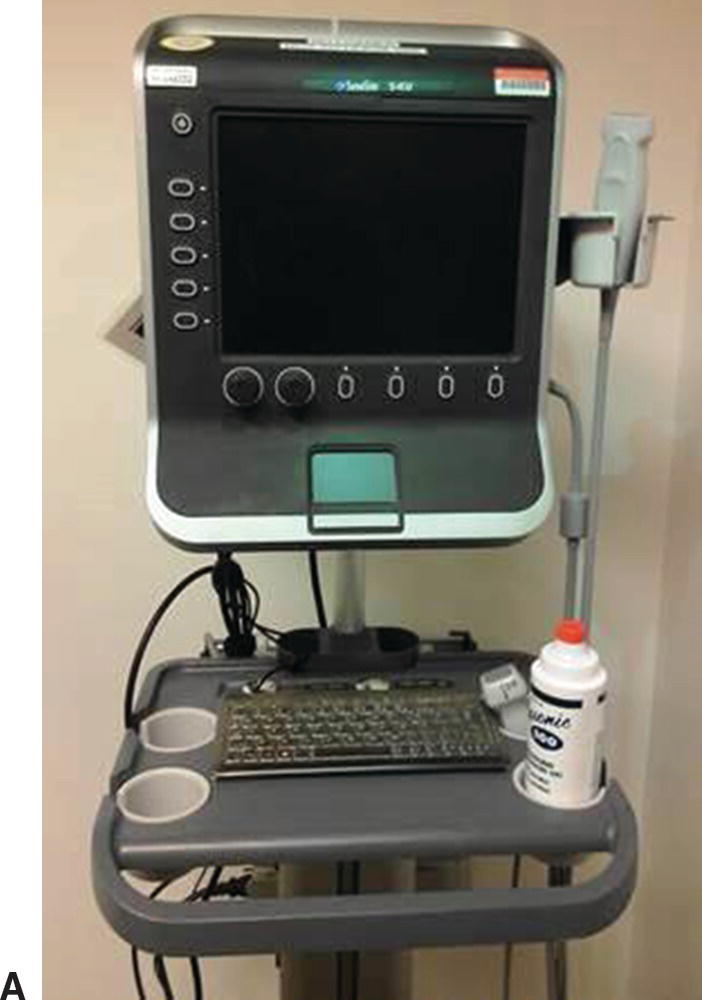

FIGURE 27.2. Examples of compact point of care ultrasound systems. A,SonoSite S-Series, photo courtesy of Amy Morris, MD. B,SonoSite NanoMaxx, photo courtesy of SonoSite, Inc.
Most vascular applications of point of care ultrasound are abbreviated or simplified versions of the complete diagnostic tests discussed elsewhere in this book. To be most effective, each application should be used to answer a specific clinical question, and the interpretation criteria should be clearly defined—preferably as a dichotomous choice (yes/no, present/absent, positive/negative). This chapter reviews some aspects that are unique or especially relevant to the use of ultrasound by a health care provider to facilitate clinical decision making or a therapeutic intervention in a patient with vascular disease.
EVALUATION OF SUSPECTED LOWER EXTREMITY ISCHEMIA
The concept of using ultrasound at the point of care is not really new in vascular surgery. In 1967, Strandness et al2 published a paper titled Ultrasonic Flow Detection—A Useful Technic in the Evaluation of Peripheral Vascular Disease in which they described their initial experience with a commercially available Doppler device. Their approach was simply to listen to the audible flow signals and learn to recognize the sounds associated with various arterial and venous abnormalities. When used in this fashion, the Doppler assessment was an extension of the physical examination. In their own words, “Since the clinician uses the instrument as he would a stethoscope, the major requirements for success are experience and normal auditory acuity.” Although this seems primitive by modern standards, these authors were able to accurately assess acute and chronic arterial occlusions, detect flow alterations produced by arteriovenous fistulas, evaluate extremity veins for thrombosis, and monitor the results of arterial reconstructions. In the summary of this paper, they state, “When used in a similar manner to a stethoscope, the examiner may learn to recognize normal arterial velocity signals and those that result from narrowing or occlusion of the arteries. With stenoses the frequency of the signal over the narrowed segment is higher than that observed in the pre-stenotic segment. With arterial occlusion, both acute and chronic, the velocity signal is absent from the involved area.” Although written almost 50 years ago, this description can still be applied at the point of care today.
Doppler Evaluation of Peripheral Arterial Pulses
A simple CW Doppler device can be used to assess peripheral arterial pulses during the physical examination (Fig. 27.3). As discussed in Chapter 7, CW Doppler signals do not allow for depth resolution and are not ideal for spectral waveform analysis; however, they can provide information on flow direction and produce signals that are suitable for audible interpretation. Experienced examiners can readily differentiate between the normal multiphasic peripheral arterial flow signal and the dampened, monophasic flow signal that is heard distal to a severe stenosis or occlusion. As described by Strandness and colleagues in 1967, a focal, high-pitched arterial signal represents the high-velocity jet within a stenosis.2 These qualitative findings can be used to establish the presence or absence of peripheral arterial disease and determine its approximate location and severity.

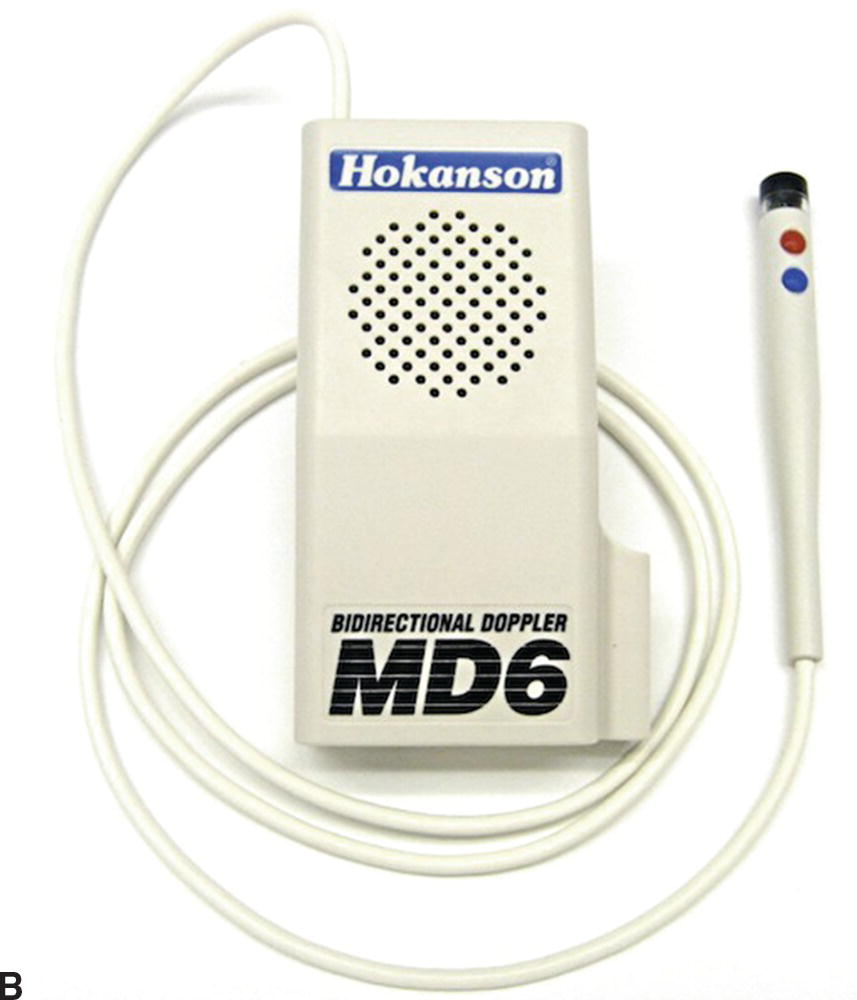
FIGURE 27.3. Continuous-wave (CW) Doppler instruments suitable for assessment of peripheral arterial pulses and measurement of ankle pressures. A,Portable Doppler. B,Pocket Doppler.
Photos courtesy of D. E. Hokanson, Inc.
Ankle-Brachial Indices (without Doppler waveforms)
The measurement of systolic ankle pressures and calculation of the ankle-brachial indices is a simple quantitative method for assessing the status of the lower extremity arterial circulation (see Chapter 13). Although tibial artery flow waveforms are routinely recorded with the ankle pressures in a formal vascular laboratory examination, this step is not necessary at the point of care. Measurement of ankle and brachial systolic pressures and audible interpretation of the CW Doppler signals from the distal tibial arteries will provide a valuable physiologic assessment of the overall severity of lower extremity arterial occlusive disease. Figure 27.4 shows Dr. Strandness performing an ankle pressure measurement in the 1970s.

FIGURE 27.4. Dr. Strandness measuring an ankle pressure in the 1970s.
COMPRESSION ULTRASOUND FOR DEEP VEIN THROMBOSIS
Screening for Proximal Lower Extremity Deep Vein Thrombosis
As discussed in Chapter 19, a complete lower extremity venous duplex examination performed in the vascular laboratory includes evaluation of multiple anatomic sites from the inferior vena cava to the tibial veins with B-mode imaging, pulsed Doppler spectral waveforms, and color Doppler. Although this comprehensive approach has become the standard test for diagnosis of acute deep vein thrombosis (DVT), a relatively quick 2-point compression ultrasound examination of the common femoral and popliteal veins has been advocated as a point of care screening test for acute proximal lower extremity DVT.9 In a randomized multicenter trial comparing whole-leg ultrasonography with the 2-point compression examination in 2465 outpatients, these two diagnostic strategies were found to be equivalent for the management of symptomatic patients with suspected DVT.10 The 2-point compression ultrasound examination has also been shown to compare favorably with CT venography for the diagnosis of femoropopliteal DVT with a sensitivity of 86% and specificity of 100%.11
The 2-point compression ultrasound examination relies completely on B-mode imaging; pulsed Doppler and color Doppler are not required. The common femoral and popliteal veins are imaged in a transverse view, and compressions are performed by downward pressure with the ultrasound probe, as illustrated in Chapter 19. After positioning the patient supine with the leg externally rotated, the common femoral vein is imaged from the inguinal ligament to the confluence of the deep femoral and femoral veins (Fig. 27.5). Next, the popliteal vein is imaged using a posterior approach from the adductor canal proximally to the confluence of the tibial veins distally (Fig. 27.6). The vein at both of these sites is compressed throughout its length in a transverse image. It is standard practice to point the indicator mark on the probe toward the right side of the patient for all transverse images, as shown in Figure 27.7, so the left side of the image will correspond to the patient’s right side—similar to the conventional orientation of a transverse image from a CT scan. With the posterior approach to the popliteal vein, the vein is typically closer to the transducer (skin line) than the artery (Fig. 27.8).

FIGURE 27.5. Patient positioning for the 2-point compression venous ultrasound examination. The leg is externally rotated, and the common femoral vein is imaged from the inguinal ligament to the confluence of the deep femoral and femoral veins in transverse view.

FIGURE 27.6. The 2-point compression venous ultrasound examination. The popliteal vein is imaged from a posterior approach in transverse view from the adductor canal proximally to the confluence of the tibial veins distally.
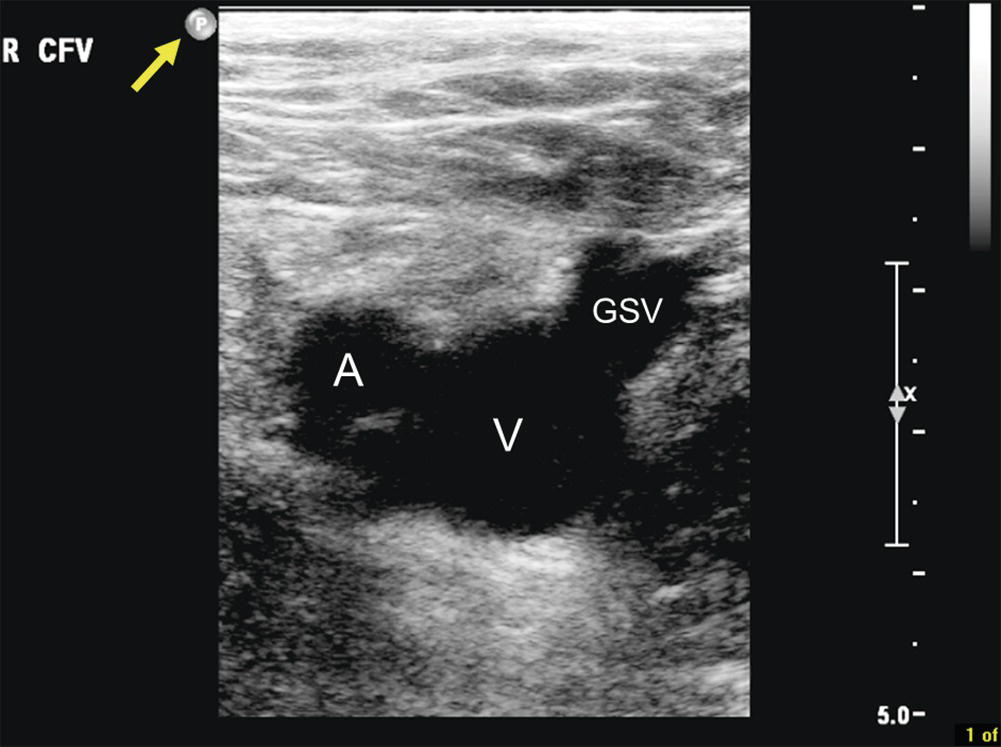
FIGURE 27.7. Transverse B-mode image of the right common femoral vein (V) in standard orientation. The indicator mark on the ultrasound probe (yellow arrow) is pointed toward the patient’s right side, so the common femoral artery (A) is lateral and the great saphenous vein (GSV) is medial.
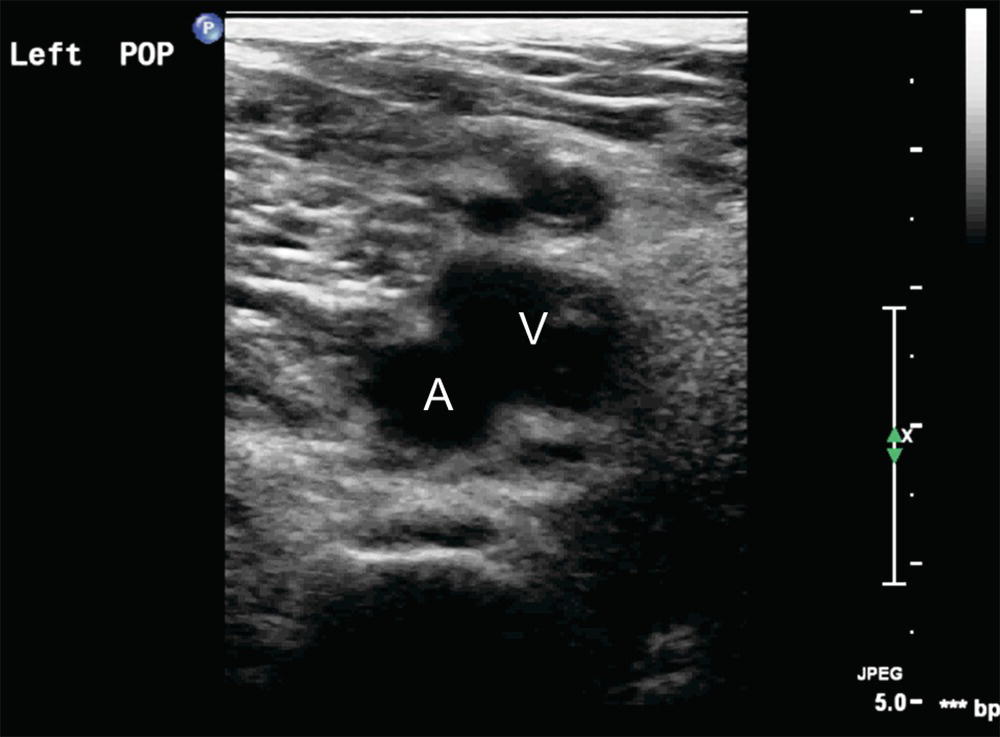
FIGURE 27.8. Transverse B-mode image of a left popliteal vein (V) taken from the posterior approach. The popliteal vein is closer to the skin line or transducer (top of the image) than the popliteal artery (A).
In some patients, thrombus will be immediately visualized in the vein lumen (Fig. 27.9), and in those cases, probe compression may not be necessary and should be performed with caution. When thrombus is visualized, longitudinal views can be used to assess the extent of the thrombus (Fig. 27.10). A normal vein is fully compressible with probe pressure, and the vessel walls are seen to coapt completely (Fig. 27.11). Failure of the vein walls to coapt is abnormal and suggests that thrombus is present in the lumen. This is especially true for acute thrombus, which tends to be hypoechoic. In some cases, ultrasound visualization is poor, and the examination is considered as equivocal or nondiagnostic.
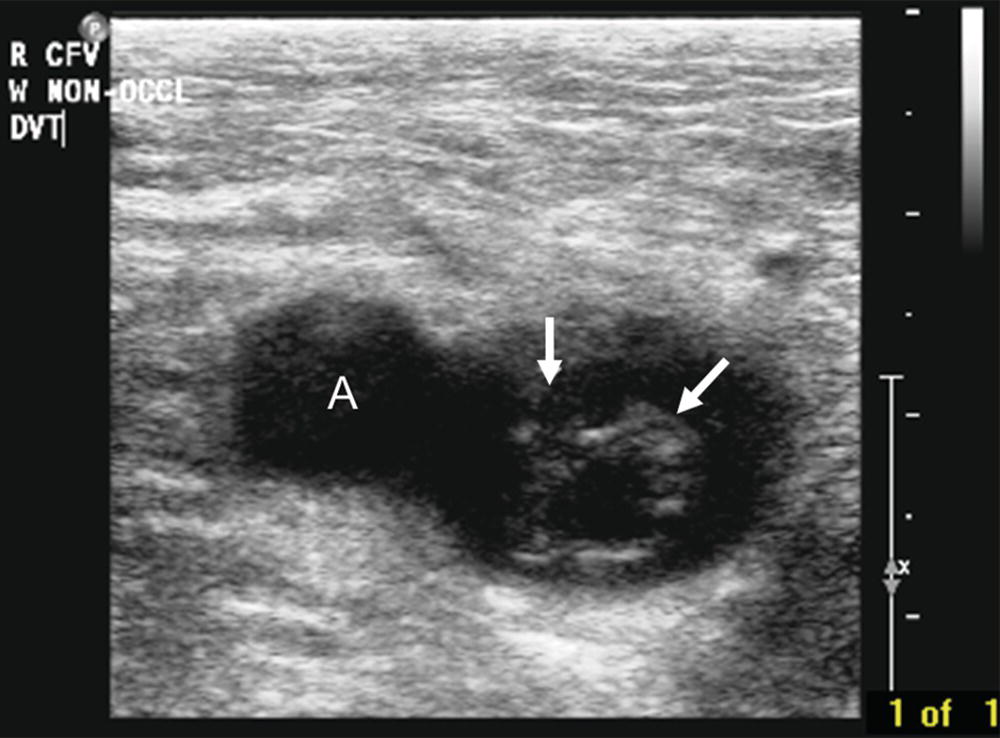
FIGURE 27.9. Transverse B-mode image of the right common femoral vein with thrombus visualized in the lumen (white arrows). The common femoral artery (A) is lateral to the vein.
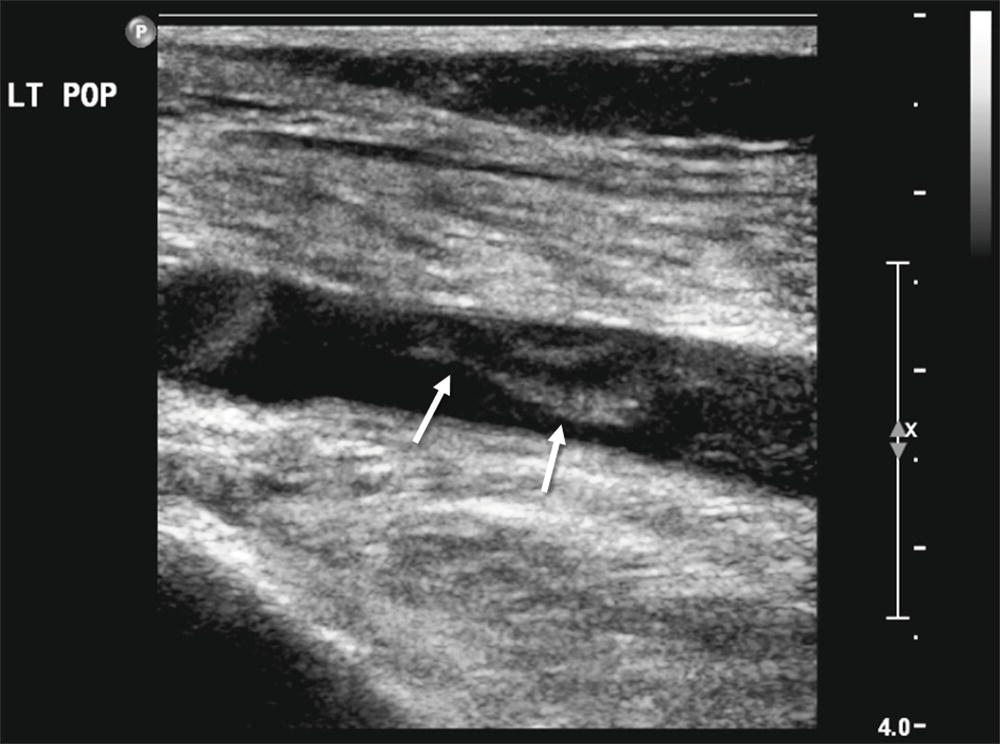
FIGURE 27.10. Longitudinal B-mode image of a left popliteal vein with thrombus visualized in the lumen (white arrows).
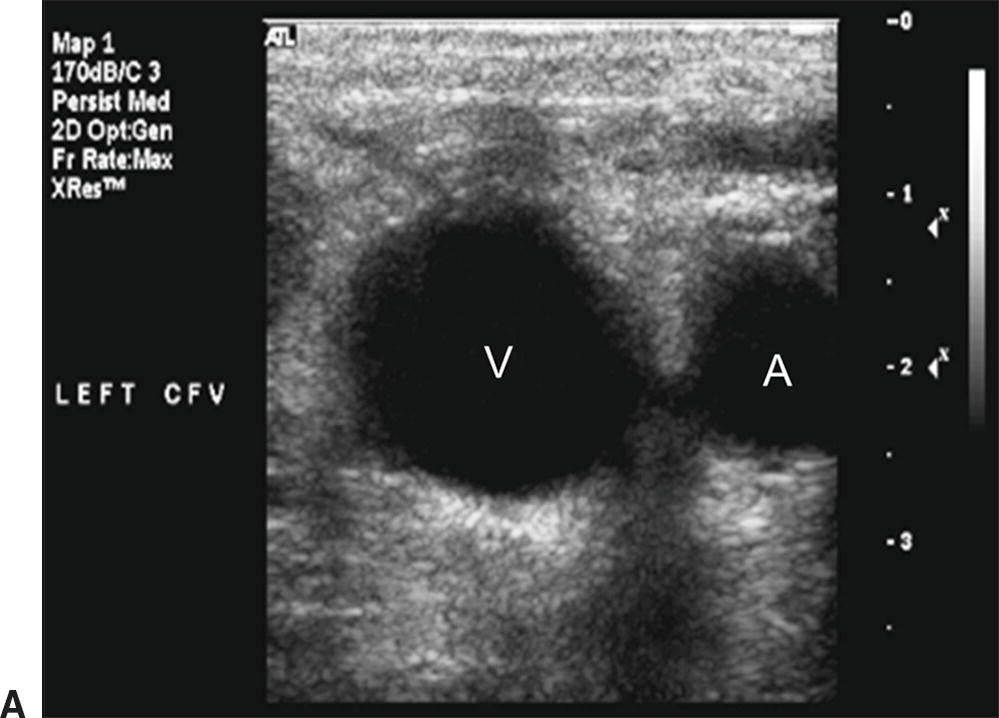
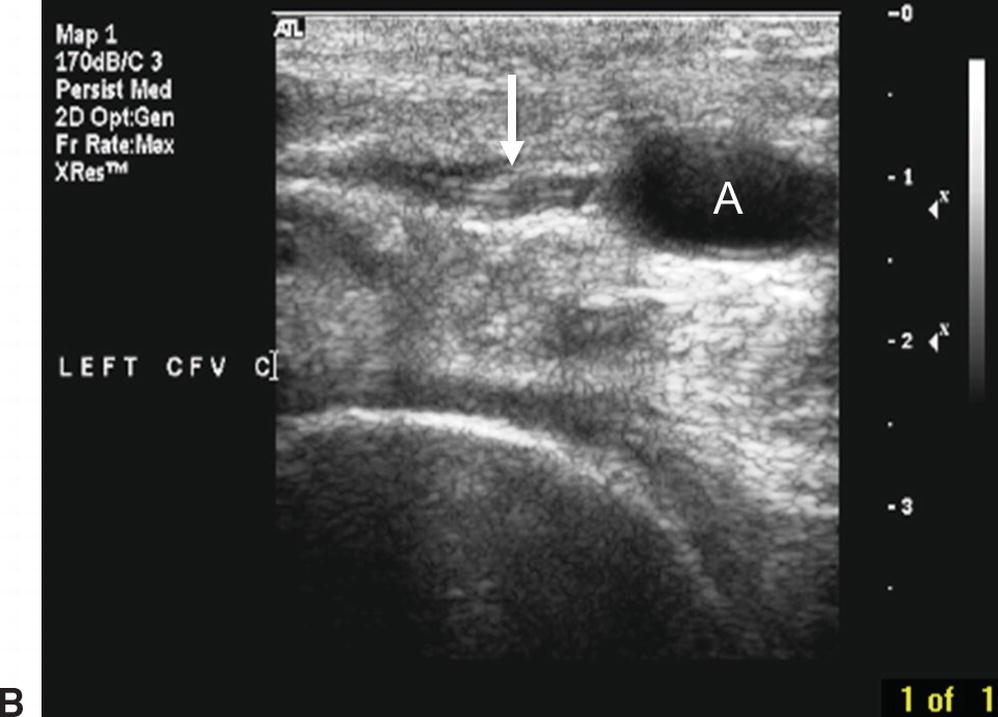
FIGURE 27.11. Normal compression of a common femoral vein. A,This transverse B-mode image shows the noncompressed left common femoral vein (V) located medial to the common femoral artery (A). B,The left common femoral vein is completely compressed (white arrow), while the common femoral artery lumen remains visible (A).
Most of the reported experience with the 2-point compression examination for detection lower extremity DVT has been in the emergency room setting. A systematic review was carried out to compare the results of the 2-point compression examination as performed by emergency physicians and a complete formal diagnostic ultrasound examination of the lower extremity.12 Six eligible studies that included a total of 936 patients were analyzed, and the overall sensitivity and specificity of the 2-point compression examination were 95% and 96%, respectively. This review also identified a number of methodologic issues that could limit the generalizability of these favorable results. The main limitations of the 2-point compression examination are that it will not detect DVT limited to the inferior vena cava and iliac veins or distal DVT in the axial or muscular calf veins. However, the results of published studies suggest that DVT isolated to these very proximal and distal segments is unusual in the outpatient setting, and the majority of patients with proximal lower extremity DVT will have abnormalities at the common femoral or popliteal vein levels that can be identified by ultrasound.13
When properly performed and interpreted, it is appropriate to begin or withhold anticoagulant treatment based on a positive or negative 2-point compression ultrasound examination for lower extremity DVT. Depending on the clinical probability and the results of d-dimer testing, a negative 2-point compression ultrasound examination may be sufficient to exclude a diagnosis of lower extremity DVT.14 However, when the clinical probability is high, a complete diagnostic lower extremity venous duplex should be considered to identify isolated inferior vena cava, iliac, or calf DVT, even when the 2-point compression examination is negative. When the 2-point compression examination is positive, treatment for lower extremity DVT can be initiated; however, it is always prudent to obtain a complete diagnostic lower extremity venous duplex to confirm the findings and document the extent of the thrombotic process.
Assessment after Saphenous Vein Ablation
Although the prevalence of thrombus extension from the superficial veins into the deep veins following saphenous vein ablation procedures is relatively low, it is common practice to perform an ultrasound examination within the first week after the procedure in order to identify those patients who might require anticoagulant treatment (see Chapter 29). Since these follow-up examinations only require limited imaging of the superficial veins and saphenofemoral or saphenopopliteal junctions, this assessment can be performed as a point of care examination in an office or clinic setting. The scanning skills required for this examination are similar to those described for 2-point compression venous ultrasound.
Ablation of the superficial veins can be confirmed by obtaining a transverse B-mode image and performing probe compressions. In successfully ablated veins, echogenic material is visualized within the noncompressible superficial vein lumen. The proximal extent of superficial vein thrombus and any extension into the adjacent deep vein should be assessed by transverse and longitudinal B-mode imaging and probe compression (Fig. 27.12). If the superficial vein thrombus extends into the deep vein by more than 50% of the deep vein diameter, then standard treatment for DVT is generally recommended. Lesser degrees of thrombus extension into the deep vein can be followed with serial ultrasound examinations or treated with anticoagulants, at the discretion of the physician.
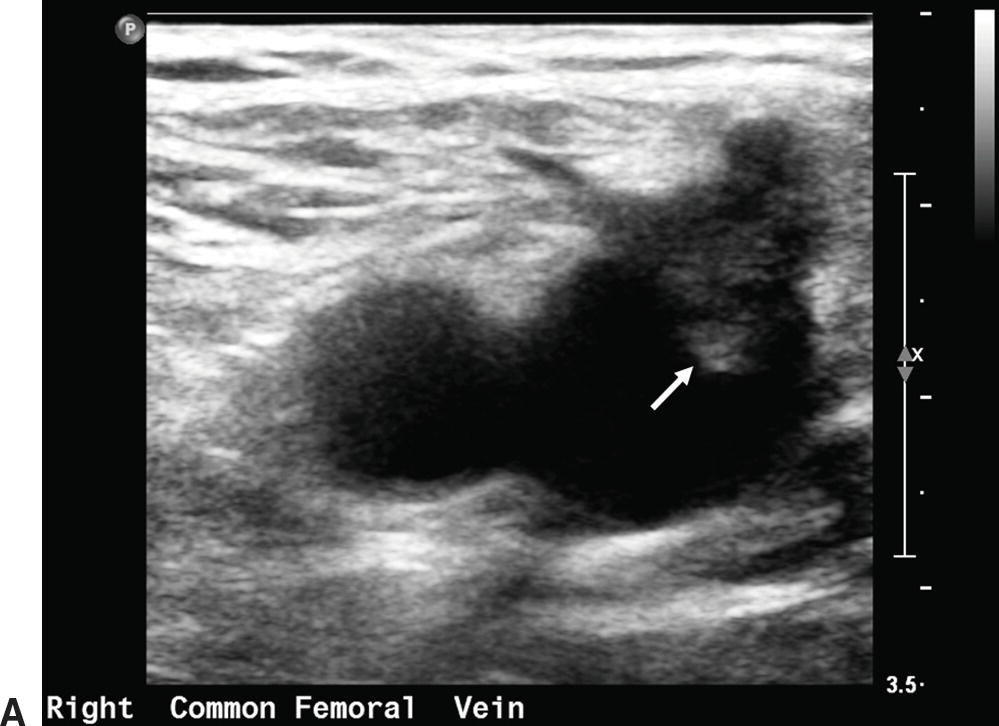
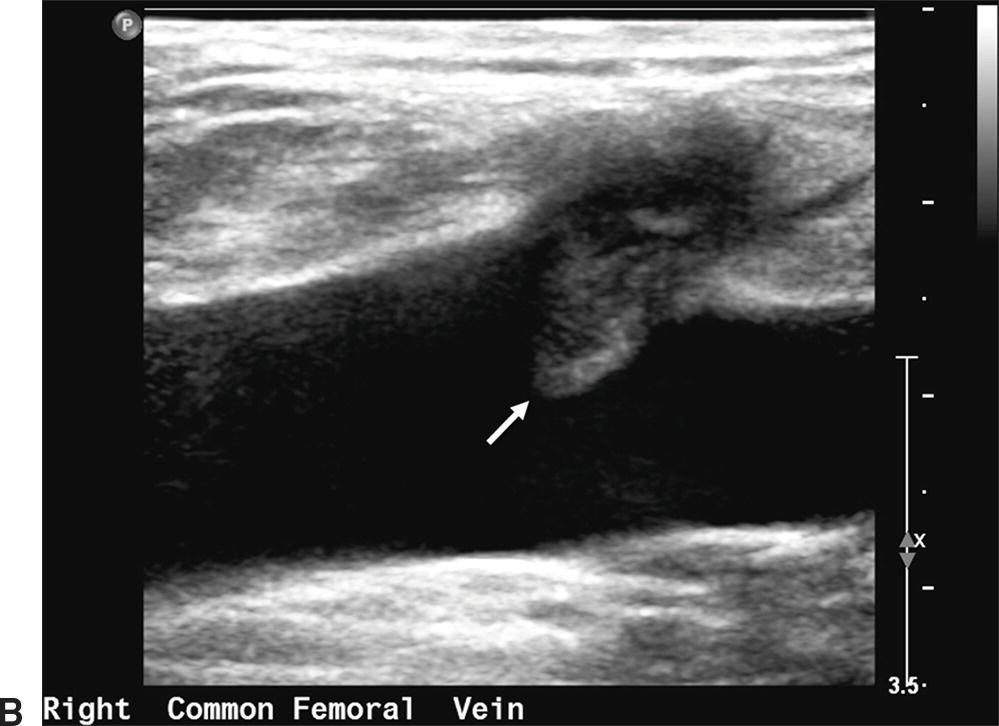
FIGURE 27.12. Thrombus at the saphenofemoral junction following a great saphenous vein ablation procedure. A,Transverse B-mode image of the right common femoral vein with thrombus visualized extending into the lumen from the great saphenous vein (white arrow). B,Longitudinal B-mode image of the same right common femoral vein with thrombus extending into the lumen (white arrow).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


