Approximately 20% of patients with heart failure have left bundle branch block (LBBB) on surface electrocardiogram (ECG). In this group of patients, detection of right ventricular (RV) dilatation on standard ECG can be of clinical relevance because RV enlargement is an important prognostic marker. Consequently, the aim of this study was to evaluate diagnostic accuracy for several electrocardiographic criteria in determining significant RV dilatation in these patients. Standard 12-lead ECGs were obtained in 173 patients with heart failure and known LBBB. From the ECG, 3 criteria for RV dilatation were defined: presence of terminal positivity in lead aVR (late R wave in lead aVR), low voltage (<0.6 mV) in all extremity leads, and an R/S ratio <1 in lead V 5 . In addition, all patients underwent comprehensive echocardiographic evaluation including assessment of RV dimensions. Measurements were performed blinded to electrocardiographic results. Significant RV dilatation was defined as an RV base-to-apex length ≥86 mm or an RV diastolic area ≥33 cm 2 . Eighty-six patients (50%) had a late R wave in lead aVR, 36 patients (21%) had low voltage in extremity leads, and 67 patients (39%) had an R/S ratio <1 in lead V 5 . An RV base-to-apex length ≥86 mm was present in 67 patients (39%), and 62 patients (36%) had an RV diastolic area ≥33 cm 2 . Any combination of 2 to 3 positive criteria could predict an RV base-to-apex length ≥86 mm with a positive predictive value of 89% and a negative predictive value of 88%. Similarly, an RV diastolic area ≥33 cm 2 was predicted with a positive predictive value of 80% and a negative predictive value of 88%. In conclusion, combining 2 to 3 distinct electrocardiographic criteria allows for accurate detection of RV dilatation in patients with heart failure and LBBB.
Approximately 20% of patients with heart failure have left bundle branch block (LBBB) on surface electrocardiogram (ECG). In patients with LBBB, ventricular activation occurs abnormally, affecting the application of conventional electrocardiographic rules for diagnosing abnormalities in blood supply, scar location, and ventricular hypertrophy because these are based on normal conduction over the bundle branch system. Attempts have been made to recognize those abnormalities in the presence of LBBB. More specifically, the possibility of detecting right ventricular (RV) dilatation using a standard ECG can be of clinical relevance because RV enlargement is a prognostic marker in these patients. Consequently, the aim of this study was to evaluate the diagnostic accuracy for several electrocardiographic criteria in determining RV dilatation in patients with heart failure and LBBB.
Methods
In total 173 patients with heart failure were selected according to the following criteria: New York Heart Association functional classes III and IV and an LBBB configuration on surface ECG. Cause of heart failure was considered ischemic in the presence of significant coronary artery disease (≥50% stenosis in ≥1 major coronary artery) and/or a history of myocardial infarction or previous revascularization. In all patients a 12-lead ECG was obtained and extensive echocardiographic evaluation including assessment of RV size and function was performed. All echocardiographic measurements were performed blinded to electrocardiographic results. From the 12-lead ECG, 3 criteria for RV dilatation were defined. Diagnostic accuracy of these electrocardiographic criteria for detecting RV dilatation was evaluated.
A standard supine artifact free 12-lead ECG (filter range 0.15 to 100 Hz, AC filter 60 Hz, 25 mm/s, 10 mm/mV) showing a supraventricular rhythm (sinus or atrial fibrillation) with an LBBB pattern was available for analysis. The interval between ECG and echocardiogram was <10 days in all patients.
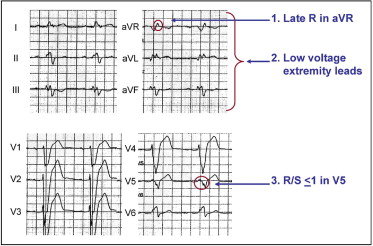
The ECG was analyzed manually and the following electrocardiographic parameters were obtained: frontal plane axis, ventricular rate, QRS width, frontal plane axis of the full and second half of the QRS complex, voltage of extremity and precordial leads, T-wave axis in frontal plane, QRS-T angle in frontal plane, presence of terminal positivity in lead aVR, presence of an R/S ratio <1 in lead V 5 , and presence of low QRS voltage (<0.6 mV) in all 6 extremity leads with a normal or increased voltage in precordial leads. For reasons outlined in the Discussion, 3 electrocardiographic criteria were selected as indicators for RV dilatation: presence of terminal positivity in lead aVR, low QRS voltage (<0.6 mV) in all extremity leads, and an R/S ratio <1 in lead V 5 ( Figure 1 ).
All patients underwent echocardiography in the left lateral decubitus position. Imaging was performed using a commercially available echocardiographic system (VIVID 7, General Electric Vingmed Ultrasound, Milwaukee, Wisconsin). Images were obtained using a 3.5-MHz transducer at a depth of 16 cm in the parasternal and apical (2- and 4-chamber) views. Standard 2-dimensional and color Doppler data triggered to the QRS complex were saved in cine-loop format and analyzed off-line with commercial software (EchoPac 108.1.5, General Electric Vingmed Ultrasound). Left ventricular (LV) end-diastolic and LV end-systolic volumes were determined from conventional apical 2- and 4-chamber views and LV ejection fraction was calculated using the biplane Simpson technique. Severity of tricuspid regurgitation and mitral regurgitation was assessed according to current guidelines.
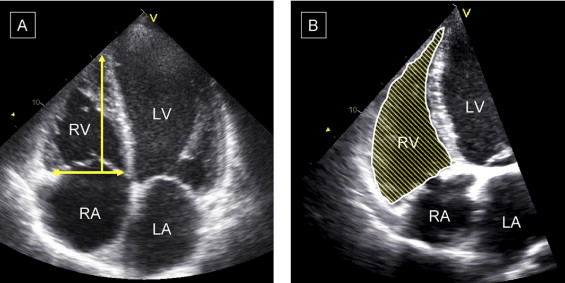
For quantification of RV size, the apical 4-chamber view was used. Special care was taken to obtain a true nonforeshortened apical 4-chamber view oriented to obtain maximum RV dimension. The RV base-to-apex length and RV diastolic area ( Figure 2 ) were assessed as described previously. Significant RV dilatation was defined as an RV base-to-apex length ≥86 mm or an RV diastolic area ≥33 cm 2 (moderate to severe RV dilatation). These specific measurements were selected because these were expected to best identify RV dilatation defined by the chosen electrocardiographic criteria.
For assessment of RV function, the tricuspid annular plane systolic excursion was measured. Pulmonary artery systolic pressure was derived from the RV to right atrial pressure gradient or tricuspid regurgitation jet gradient and calculated with the modified Bernoulli equation.
Continuous data are presented as mean ± SD and dichotomous data are presented as numbers and percentages. Comparison of data between patient groups was performed using independent-samples t test for continuous data. Fisher’s exact tests or chi-square tests were used as appropriate to compare dichotomous data. Comparisons between >2 patient groups were performed using 1-way analysis of variance with Bonferroni post hoc testing. All analyses were performed with SPSS 16.0 for Windows (SPSS, Inc., Chicago, Illinois). All statistical tests were 2-sided. A p value <0.05 was considered statistically significant.
Results
Baseline characteristics of the patient population are presented in Table 1 . Most patients were men (64%) and cause of heart failure was ischemic cardiomyopathy in 83 patients (48%). No differences were observed between patients with ischemic heart failure and those with nonischemic heart failure, except that ischemic patients were older (68 ± 9 vs 63 ± 10 years, p <0.001) and more frequently men (76% vs 53%, p = 0.002). Mean heart rate during electrocardiographic registration was 71 ± 13 beats/min and mean QRS duration was 178 ± 16 ms. Other electrocardiographic parameters are listed in Table 1 . When assessing the predefined electrocardiographic criteria, the following observations were made: (1) 86 patients (50%) patients had a late R wave in lead aVR, (2) 36 patients (21%) had low voltage in extremity leads, and (3) 67 patients (39%) had an R/S ratio <1 in lead V 5 . There were 51 patients (29%) without any positive criterion for RV dilatation, 61 patients (35%) had 1 positive criterion, 55 patients (32%) had 2 positive criteria, and 6 patients (3%) had all 3 positive criteria.
| Clinical Parameters | |
| Age (years) | 65 ± 10 |
| Men/women | 111/62 |
| New York Heart Association functional class | |
| III | 162 (94%) |
| IV | 11 (6%) |
| Cause of heart failure | |
| Ischemic | 83 (48%) |
| Nonischemic | 90 (52%) |
| Medications | |
| Angiotensin-converting enzyme inhibitors | 151 (87%) |
| Diuretics | 158 (91%) |
| β Blockers | 123 (71%) |
| Spironolactone | 83 (48%) |
| Digoxin | 25 (14%) |
| Electrocardiographic parameters | |
| Heart rate (beats/min) | 71 ± 13 |
| QRS duration (ms) | 178 ± 16 |
| QRS axis (°) | −22 ± 39 |
| QRS axis second half (°) | −50 ± 43 |
| QRS-T angle (°) | 136 ± 43 |
| Echocardiographic parameters | |
| Left ventricular end-diastolic volume (ml) | 234 ± 88 |
| Left ventricular end-systolic volume (ml) | 180 ± 77 |
| Left ventricular ejection fraction (%) | 24 ± 8 |
| Mitral regurgitation (grade) | 1.7 ± 1.0 |
| Right ventricular base-to-apex length (mm) | 82 ± 8 |
| Right ventricular diastolic area (cm 2 ) | 28 ± 7 |
| Tricuspid annular plane systolic excursion (mm) | 18 ± 3 |
| Pulmonary artery systolic pressure (mm Hg) | 34 ± 9 |
| Tricuspid regurgitation (grade) | 1.5 ± 1.0 |
Mean values for all echocardiographic findings are listed in Table 1 . Significant RV dilatation defined as an RV base-to-apex length ≥86 mm was present in 67 patients (39%), and an RV diastolic area ≥33 cm 2 was noted in 62 patients (36%). Of note, a concordance between the 2 definitions was found in 160 patients (92%). Mean values of RV size and function measurements in patients with 0 or 1 criterion 2 or 3 positive electrocardiographic criteria are listed in Table 2 . There were significant differences between groups in all tested RV size and RV function measurements. In particular, after post hoc testing, patients with 2 or 3 positive electrocardiographic criteria had a longer RV base-to-apex length, larger RV diastolic area, higher tricuspid regurgitation grade, and higher pulmonary artery systolic pressure (p <0.05 for all tests) compared to patients with 0 positive electrocardiographic criterion ( Table 2 ).
| 0 Positive | 1 Positive | 2 Positive | 3 Positive | p Value | |
|---|---|---|---|---|---|
| (n = 51) | (n = 61) | (n = 55) | (n = 6) | ||
| Right ventricular base-to-apex length (mm) | 78 ± 6 | 78 ± 6 | 90 ± 5 ⁎ | 92 ± 6 ⁎ | <0.001 |
| Right ventricular diastolic area (cm 2 ) | 25 ± 6 | 25 ± 7 | 34 ± 5 ⁎ | 36 ± 3 ⁎ | <0.001 |
| Tricuspid annular plane systolic excursion (mm) | 18 ± 3 | 19 ± 2 | 18 ± 4 | 16 ± 4 | 0.034 |
| Pulmonary artery systolic pressure (mm Hg) | 30 ± 8 | 30 ± 9 | 38 ± 7 ⁎ | 46 ± 2 ⁎ | <0.001 |
| Tricuspid regurgitation (grade) | 1.1 ± 0.8 | 1.4 ± 0.9 | 2.0 ± 0.9 ⁎ | 2.2 ± 1.3 ⁎ | 0.002 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


