A 53-year-old woman is described who underwent mitral and aortic valve replacement and tricuspid valve annuloplasty for pure regurgitation at all 3 valve sites for unrecognized carcinoid heart disease without the carcinoid syndrome 22 days before death. Metastatic carcinoid was not recognized until necropsy, which disclosed a probable ovarian primary but with large hepatic metastases and left-sided cardiac involvement either greater than or equal to the right-sided involvement. Pulmonary hypertension, very unusual in carcinoid heart disease, persisted postoperatively and probably played a role in the patient’s early death. Hepatic metastasis with ovarian primary is most unusual in this circumstance.
It was in 1930, 80 years ago, when the first patient with a metastasizing carcinoid neoplasm associated with fibrous lesions on the right side of the heart was described. In 1931, the first patient with metastasizing carcinoid syndrome (head and upper chest flushes and diarrhea) associated with fibrous lesions not only on the tricuspid and pulmonic valves but also on the anterior mitral leaflet and left ventricular mural endocardium was described. Subsequently, of course, numerous reports have appeared describing clinical and morphologic features of the carcinoid syndrome and carcinoid heart disease. Most patients have the primary carcinoid in the small intestine, widespread metastases, and specific carcinoid plaques limited to the right side of the heart. The present report was prompted by study of a patient with severe mitral and aortic regurgitation leading to double valve replacement but without symptoms of the carcinoid syndrome but with metastasizing carcinoid.
Case Description
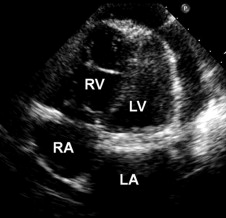
A 53-year-old mother of 6, who was born May 5, 1955, and died February 18, 2009, had been well until November 2008, when she noted exertional dyspnea, subcutaneous peripheral edema, and recurring palpitations, which proved to be runs of atrial fibrillation. The symptoms gradually worsened, with episodes of rapid heart rate, each lasting several minutes. On January 26, 2009, cardiac catheterization disclosed the following pressures in mm Hg: pulmonary arterial wedge mean 22, a wave 30, v wave 28; pulmonary trunk 56/10; right ventricle 56/18; right atrial mean 9, a wave 15, v wave 10; left ventricle 130/26; and aorta 127/58. Left ventriculography disclosed a normal-sized left ventricular cavity, with an ejection fraction of 60% and 4+/4+ mitral regurgitation. Aortography disclosed 4+/4+ aortic regurgitation. The coronary arteries were angiographically normal. Echocardiography showed thickened mitral and aortic valve cusps and a normal-sized left ventricle ( Figure 1 ).
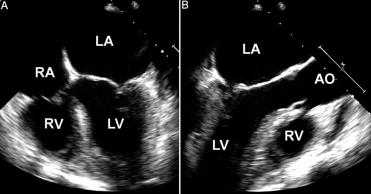
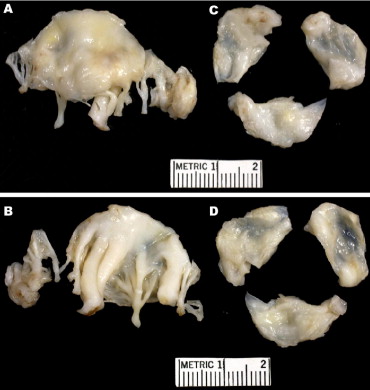
On January 27, 2009, the mitral and aortic valves were replaced with mechanical prostheses (#20 ATS Medical [Minneapolis, Minnesota] in the aortic position and #29 St. Jude Medical [St. Paul, Minnesota] in the mitral position). A Maze procedure was also performed as well as tricuspid valve annuloplasty. The operatively excised valves are shown in Figures 2 and 3 . The 6-day postoperative hospital course was characterized by a weight gain of 6.6 kg (from 76.7 to 83.3 kg), sinus rhythm, and gradual ambulation.
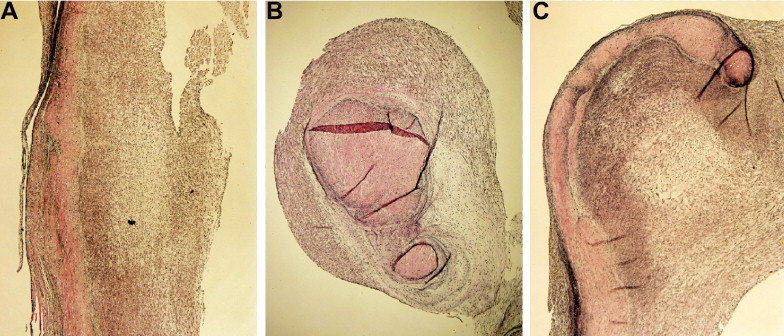
On February 13, 2009, the patient was rehospitalized because of increasing weakness and dyspnea, evidence of gastrointestinal bleeding (on warfarin with an international normalized ratio of 4.7), and large pleural and pericardial effusions. The blood hemoglobin level was 11.1 g/dl, and the hematocrit was 35%. The serum bilirubin level was 1.4 mg/dl; alkaline phosphatase, 295 U/L; aspartate aminotransferase, 210 U/L; and alanine aminotransferase, 147 U/L. The blood urea nitrogen level was 17 mg/dl and glucose 96 mg/dl. The brain natriuretic peptide level was 430 pg/ml (normal range <100). Echocardiography now showed a normal-sized, normally functioning left ventricle, a very dilated and dysfunctional right ventricle, and large pericardial and right pleural effusions ( Figure 4 ). Approximately 1,800 ml of serous fluid was drained from the right pleural space. Shortly thereafter, the patient had a cardiac arrest and died.