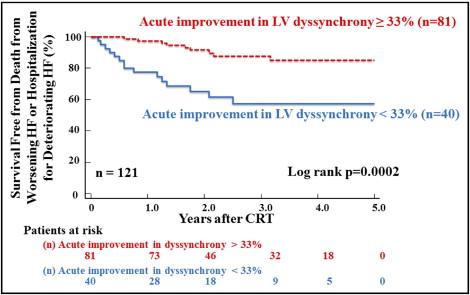
Although left ventricular (LV) mechanical dyssynchrony can predict the response to cardiac resynchronization therapy (CRT), the presence of baseline LV dyssynchrony might not be the only determinant of the response to CRT. The objectives of the present study were to test the hypothesis that a combined assessment of baseline LV dyssynchrony and its acute improvement can produce a more accurate prediction of the long-term outcomes after CRT. We studied 121 patients with heart failure undergoing CRT. LV dyssynchrony was determined by measuring the anteroseptal-to-posterior wall time delay using the speckle-tracking radial strain (≥130 ms was predefined as significant) and was assessed at baseline and 7 ± 3 days after CRT. Long-term unfavorable outcome events were tracked for 5 years. Acute improvement in LV dyssynchrony of ≥33% was predictive of the long-term outcome with an area under the curve of 0.67 (p = 0.0024). Using this cutoff value, the Kaplan-Meier curve showed that patients with acute improvement in LV dyssynchrony experienced fewer cardiovascular events than those without (log-rank p = 0.0002). The event-free survival of patients whose baseline LV dyssynchrony was ≥130 ms and whose acute improvement in LV dyssynchrony was ≥33% was greater than that of the patients with baseline LV dyssynchrony of ≥130 ms but with acute improvement in LV dyssynchrony of <33% (88% vs 65%, p = 0.012). In conclusion, the combined assessment of baseline LV dyssynchrony and its acute improvement after CRT produced a more accurate prediction of long-term outcomes after CRT.
Although cardiac resynchronization therapy (CRT) is an established treatment of patients with advanced heart failure (HF) with depressed left ventricular (LV) ejection fraction (EF) and wide QRS duration, it is well known that roughly ⅓ of patients do not respond to CRT when they are selected according to these current standard criteria. The presence of a substantial number of nonresponders after CRT has a wide variety of causes, but a large body of data supports LV mechanical dyssynchrony as a prognostic marker for patient response to CRT. Baseline LV mechanical dyssynchrony can predict the response to CRT; however, the presence of baseline LV dyssynchrony might not be the only determinant of the response to CRT, because some patients with significant LV dyssynchrony still do not respond to CRT. In addition, the association of baseline LV dyssynchrony and the improvement in LV dyssynchrony immediately after CRT with the long-term response to CRT remains unknown. Accordingly, the objectives of the present study were to test the hypothesis that a combined assessment of baseline LV dyssynchrony and its acute improvement would produce a more accurate prediction of the long-term outcomes after CRT.
Methods
A series of 128 consecutive patients with HF undergoing CRT were prospectively enrolled in the present study from 2 centers, Kobe University Graduate School of Medicine (Kobe, Japan) and Himeji Cardiovascular Center (Himeji, Japan). Seven patients (5%) were excluded from all subsequent analyses because of poor echocardiographic image quality; thus, eventually 121 patients with HF were enrolled in the present study ( Table 1 ). Their mean age was 68 ± 11 years, the EF was 26 ± 6% (all ≤35%), and the QRS duration was 164 ± 23 ms (all ≥120 ms), 36 patients (30%) were women, and 30 (25%) had ischemic cardiomyopathy, defined as a history of myocardial infarction. All patients were classified as New York Heart Association functional class III or IV and were receiving optimal pharmacologic therapy, if tolerated. Of the 121 patients, 82 (68%) had been diagnosed with sinus rhythm and 5 (4%) with atrial fibrillation, and 34 (28%) had previously undergone implantation of permanent right ventricular pacing. the local ethics committees of both institutions approved this study, and all patients provided written informed consent.
| Variable | |
|---|---|
| Age (years) | 68 ± 11 |
| Women | 36 (30%) |
| Coronary disease | 30 (25%) |
| QRS duration (ms) | 164 ± 23 |
| Rhythm | |
| Sinus rhythm | 82 (68%) |
| Atrial fibrillation | 5 (4%) |
| Right ventricular pacing | 34 (28%) |
| QRS morphology | |
| Left bundle branch block | 41 (34%) |
| Right bundle branch block | 4 (3%) |
| Right ventricular pacing | 34 (28%) |
| Intraventricular conduction delay | 42 (35%) |
| New York Heart Association functional class | |
| III | 105 (87%) |
| IV | 16 (13%) |
| Medication | |
| Diuretics | 107 (88%) |
| Loop diuretics | 101 (82%) |
| Spironolactone | 76 (61%) |
| Angiotensin-converting enzyme inhibitors/angiotensin II receptor blockers | 94 (77%) |
| β Blockers | 98 (80%) |
| Left ventricular ejection fraction (%) | 26 ± 6 |
| Left ventricular end-diastolic volume (ml) | 190 ± 72 |
| Left ventricular end-systolic volume (ml) | 171 ± 77 |
| Left ventricular dyssynchrony (ml) | 315 ± 125 |
All echocardiographic studies were performed using commercially available echocardiography systems (Vivid 7; GE-Vingmed, Horten, Norway, or Aplio SSA-770A; Toshiba Medical System, Tochigi, Japan) before and 7 ± 3 days after CRT. Digital routine grayscale 2-dimensional cine loops were obtained, including mid-LV short axis views at the level of the papillary muscle and standard 3-dimensional apical views. The mean frame rate was 60 ± 4 frames/s in the short-axis view for grayscale imaging, which was used for speckle-tracking analysis. All data were prospectively and blindly analyzed by the coordinating echocardiographic core laboratory at Kobe University Hospital. For patients with atrial fibrillation, measurements of standard echocardiographic and speckle-tracking parameters were obtained as the average of ≥4 cardiac cycles. Digital data were transferred to dedicated software (EchoPAC, version 8.0.0; GE Vingmed, Horten, Norway, or EchoAgent; Toshiba Medical System, Tochigi, Japan) for subsequent off-line analysis. The LV volumes and EF were assessed using biplane Simpson’s rule.
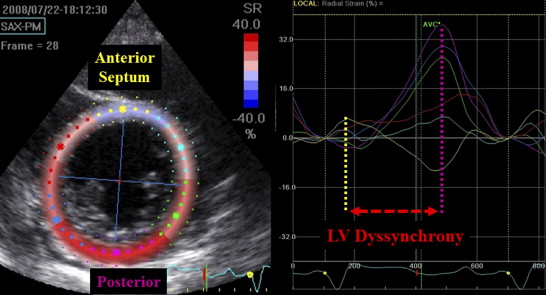
Baseline LV dyssynchrony was assessed using speckle-tracking radial strain from the mid-LV short-axis images, as previously described in detail. Radial dyssynchrony by speckle-tracking strain was defined as the time difference between the anteroseptal and posterior wall segmental peak strains ( Figure 1 ). A baseline speckle-tracking radial dyssynchrony ≥130 ms was predefined as significant. In addition, an acute change in LV dyssynchrony was detected as a decrease in speckle-tracking radial dyssynchrony 7 ± 3 days after CRT compared with the baseline value.
Biventricular pacing systems were implanted with right ventricular apical leads and an LV lead through the coronary sinus in 118 of the patients. The LV leads were placed in the lateral veins of 56 patients, the posterolateral veins of 45 patients, and the anterolateral veins of 17 patients. The epicardial surgical approach was required for the remaining 3 patients. Device implantation was successful in all cases without any major complications. Biventricular pacing systems with an implantable cardiovascular-defibrillator were implanted in 35 patients (29%). The atrioventricular interval was adjusted for optimal diastolic filling using Doppler echocardiographic assessment of mitral inflow, as was the interventricular interval using Doppler echocardiographic assessment of LV outflow 7 ± 3 days after implantation.
Long-term unfavorable outcome events were prespecified as the primary end points of death from worsening HF and hospitalization for deteriorating HF. Long-term follow-up after CRT was tracked for 5 years.
All group data are presented as the mean ± SD and were compared using the 2-tailed Student t test for unpaired data for 2 groups. Proportional differences were evaluated with Fisher’s exact test or the chi-square test, as appropriate. Receiver operating characteristic curves were computed to determine the optimal cutoff values for the prediction of cardiovascular events and for the calculation of the area under the curve for each of the indexes to determine their prognostic significance. Event-free survival curves were determined by the Kaplan-Meier method, and cumulative event rates were compared using the log-rank test. The intraclass correlation coefficient was used to determine inter- and intraobserver reproducibility from 20 randomly selected subjects. Statistical significance was set at p <0.05. All the analyses were performed with commercially available software (MedCalc software, version 10.4.0.0, MedCalc Software, Mariakerke, Belgium).
Results
The baseline clinical and echocardiographic characteristics of the 121 patients with HF are summarized in Table 1 . The following primary end points of a prespecified cardiovascular event occurred in 24 patients (20%): 9 deaths from worsening HF and 15 hospitalizations for deteriorating HF. In addition, of 35 patients with implanted biventricular pacing systems with an implantable cardiovascular-defibrillator, 3 (9%) received an appropriate shock during follow-up. Of the initially excluded 7 patients, 1 met the primary end point, including hospitalization for deteriorating HF. Patients with and without cardiovascular events showed similar values for mean age, QRS duration, LV volume, EF, New York Heart Association functional class, and prevalence of women ( Table 2 ). The differences observed were that the LV dyssynchrony of patients with cardiovascular events was significantly larger (330 ± 117 vs 257 ± 142 ms, p = 0.001; Table 2 ), and prevalence of coronary disease of patients with cardiovascular events was significantly greater, than for patients without cardiovascular events (41% vs 21%, p = 0.03; Table 2 ). The intraclass correlation coefficients for interobserver reproducibility of speckle-tracking radial dyssynchrony was 0.971 (95% confidence interval 0.928 to 0.989), and that for intraobserver reproducibility was 0.850 (95% confidence interval 0.652 to 0.939).
| Variable | Patients Without Events (n = 97) | Patients With Events (n = 24) | p Value |
|---|---|---|---|
| Age (years) | 68 ± 10 | 66 ± 11 | NS |
| Women | 27 (28%) | 8 (33%) | NS |
| Coronary disease | 20 (21%) | 10 (41%) | 0.03 |
| QRS duration (ms) | 164 ± 23 | 163 ± 28 | NS |
| Rhythm | |||
| Sinus rhythm | 69 (71%) | 13 (54%) | NS |
| Atrial fibrillation | 3 (3%) | 2 (8%) | NS |
| Right ventricular pacing | 25 (26%) | 9 (38%) | NS |
| QRS morphology | |||
| Left bundle branch block | 36 (37%) | 5 (20%) | NS |
| Right bundle branch block | 3 (3%) | 1 (4%) | NS |
| Right ventricular pacing | 25 (26%) | 9 (38%) | NS |
| Intraventricular conduction delay | 33 (34%) | 9 (38%) | NS |
| New York Heart Association functional class | NS | ||
| III | 87 (90%) | 18 (75%) | |
| IV | 10 (10%) | 6 (25%) | |
| Medication | |||
| Diuretics | 84 (86%) | 23 (95%) | NS |
| Loop diuretics | 78 (80%) | 23 (95%) | NS |
| Spironolactone | 57 (59%) | 19 (79%) | NS |
| Angiotensin-converting enzyme inhibitors/angiotensin II receptor blockers | 83 (86%) | 15 (63%) | <0.01 |
| β Blockers | 84 (86%) | 20 (83%) | NS |
| Left ventricular ejection fraction (%) | 27 ± 6 | 26 ± 6 | NS |
| Left ventricular end-diastolic volume (ml) | 187 ± 68 | 203 ± 87 | NS |
| Left ventricular end-systolic volume (ml) | 169 ± 77 | 181 ± 83 | NS |
| Left ventricular dyssynchrony (ml) | 330 ± 117 | 257 ± 142 | 0.01 |
Receiver operating characteristic curves were constructed to determine the optimal cutoff value of acute changes in LV dyssynchrony for the prediction of cardiovascular events during long-term follow-up after CRT. The receiver operating characteristic curve analysis identified the optimal cutoff of acute changes in LV dyssynchrony as ≥33%, with sensitivity of 63%, specificity of 74%, and area under the curve of 0.672 (p = 0.0024). When using this cutoff, the Kaplan-Meier curve showed that patients with acute changes in LV dyssynchrony of ≥33% experienced fewer cardiovascular events than those with changes of < 33% (log-rank p = 0.0002; Figure 2 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


