Patients with congenital heart disease (CHD) are at increased risk of cardiac arrhythmias. The utility of ambulatory (Holter) monitoring in predicting these arrhythmias remains unclear. We sought to evaluate the clinical utility and cost effectiveness of Holter monitoring in patients with CHD. A retrospective study of patients with CHD who had undergone Holter monitoring was performed. The Holter data from patients with tetralogy of Fallot (TOF), d-transposition of the great arteries (d-TGA) after an atrial switch operation, and patients with a single ventricle after Fontan palliation were reviewed. The Holter indication included evaluation of clinical symptoms or as a part of routine screening. The Holter results were deemed clinically significant if they resulted in a change in patient treatment. Sudden cardiac events included death or aborted sudden death and appropriate defibrillator therapies. A total of 589 Holter studies were performed in 189 patients (100 with TOF, 38 with d-TGA, and 51 with Fontan). The results of Holter monitoring performed for clinical symptoms had a low positive predictive value (0.08) for clinically significant changes in management. On routine monitoring, the sensitivity was low (0.40) but the negative predictive value was high (0.96) for future clinically significant arrhythmias. The frequency of clinically significant findings and associated cost-effectiveness improved with older patient age and Fontan and d-TGA CHD type. Nonsustained ventricular tachycardia was associated with sudden cardiac events in patients with TOF but not in those with d-TGA or Fontan palliation. In conclusion, Holter monitoring is generally inefficient for symptomatic evaluation; however, within specific age and CHD type subgroups, such as patients with repaired TOF >25 years old, it could be useful in clinical management and risk assessment as a part of routine care.
It has been estimated that 85% of children diagnosed with congenital heart disease (CHD) will survive to reach adulthood, including 80% of patients with complex forms of CHD. Current guidelines such as the American Heart Association and European Society of Cardiology guidelines remain vague with respect to evidence regarding the utility of Holter monitoring in patients with CHD. In the present study, we sought to determine the utility of clinical 24-hour ambulatory Holter monitoring in adolescent and adult patients with complex CHD, including tetralogy of Fallot (TOF) after surgical repair, d-transposition of the great arteries (d-TGA) after the Mustard or Senning procedure, and patients with single ventricular physiology after Fontan palliation. The aims of the present study were to (1) describe the arrhythmia findings from individual Holter studies by age and CHD type and determine the positive and negative predictive value of Holter monitoring in patients with and without clinical symptoms, and (2) describe the Holter findings in patients with CHD during their lifetime and determine the sensitivity, specificity, and negative predictive value of Holter monitoring in the detection of clinically significant arrhythmias in individual patients. Additionally, we analyzed the resource usage involved with clinical Holter monitoring in patients with CHD.
Methods
The present study was a single-institution, retrospective analysis of ambulatory Holter monitoring in patients with CHD from January 2001 to January 2011 and was conducted in accordance with the Cincinnati Children’s Hospital Medical Center institutional review board (protocol no. 2010-2865). The patients were included if they were ≥18 years at Holter monitoring, had had ≥1 previous Holter study, and had 1 of the following forms of CHD: TOF after surgical repair, d-TGA with previous atrial switch operation, including Mustard or Senning palliation, and single ventricle physiology after Fontan palliation.
The patient demographic, cardiac, and electrophysiologic data from the general cardiology and electrophysiologic-specific databases were reviewed. The demographic data collected included patient age, gender, previous electrophysiologic-related procedures, history of syncope, sudden cardiac death, aborted sudden cardiac death event, and cardiac transplantation. The cardiac rhythm device data collected included device type (pacemaker or implantable cardioverter-defibrillator [ICD], and the clinical indications for device implantation. For patients with an ICD device, the device charts were reviewed to determine whether the patient had received a device shock and whether the given therapy was appropriate or inappropriate. An inappropriate therapy event was defined as ventricular antitachycardia pacing or shock delivered for rhythms that were incorrectly characterized by the device. The arrhythmia history was reviewed, including documentation of a history of atrial fibrillation or flutter, supraventricular rhythms other than atrial fibrillation or flutter, ventricular arrhythmias, and a history of antiarrhythmic drug therapy.
After patient identification, all ambulatory Holter monitor studies were reviewed for each patient. For each Holter study, data were collected for an indication for ambulatory monitoring, study findings, and the effect of the study on clinical management. The Holter monitor indications were categorized as follows: (1) routine screening in an asymptomatic patient with no previous arrhythmia history, (2) routine screening in an asymptomatic patient with a history of arrhythmia, (3) evaluation of a symptomatic patient with no history of arrhythmia, (4) evaluation of a symptomatic patient with history of previous arrhythmia, and (5) screening in an asymptomatic patient with benign clinical findings such as premature ventricular contractions seen on routine electrocardiograms. For the purposes of statistical comparisons, these categories were collapsed into 2 groups: the presence or absence of clinical symptoms as an indication for Holter monitoring.
Each Holter study was analyzed for atrial arrhythmias, ventricular arrhythmias, central conduction system abnormalities such as sinus node dysfunction or atrioventricular nodal disease, and patient-reported symptoms during monitoring. Atrial and ventricular arrhythmias were categorized as follows: no ectopy, rare or occasional single ectopic beats (1 to <720 beats/24 hours), frequent single ectopic beats (≥720 beats/24 hours), nonsustained tachycardia (4 consecutive beats to 30 seconds of arrhythmia), and sustained arrhythmias (>30 seconds of arrhythmia). All patient-reported symptoms during ambulatory monitoring were noted and compared to the rhythm at clinical symptoms. A clinically significant study was defined as a study that led to a change in clinical management, including ≥1 of the following clinical outcomes: electrophysiologic study, pacemaker or ICD implantation or replacement, initiation or change in antiarrhythmic drug therapy, or findings that directly led to additional testing. A significant clinical arrhythmia was defined as clinical atrial fibrillation, atrial flutter, nonatrial supraventricular tachycardia (atrioventricular tachycardia and atrioventricular nodal tachycardia), sudden cardiac death, and a history of appropriate ICD device therapy. For evaluation of the individual Holter studies, additional analyses were performed stratified by patient age at monitoring. Subanalyses included studies stratified by patient age: <18, 18 to 25, and >25 years.
The Holter findings were analyzed from 2 perspectives. First, the individual Holter studies were analyzed as separate events to determine the positive predictive value and negative predictive value of Holter monitoring in patients with and without clinical symptoms. Second, the cumulative data from the ≥1 Holter studies from each individual patient were analyzed to determine the sensitivity, specificity, and negative predictive value of Holter monitoring in the detection of clinically significant arrhythmias by individual case history. Comparisons of proportions were made using the exact test or other chi-square test, as appropriate.
Cost analysis for ambulatory monitoring was performed using the 2011 average hospital reimbursement rates for Holter monitoring at Cincinnati Children’s Hospital ($407.71). This included all payer reimbursement types, including third-party payers, self-pay, and Medicare or Medicaid. An analysis on the cost per study that affected clinical management was performed for the total population and for the individual CHD type and age cohorts.
Results
A total of 245 patients with either TOF after repair, d-TGA after a Mustard or Senning procedure, or Fontan were identified ( Table 1 ). Of the total cohort of identified patients with CHD, 189 of the patients (77%) had ≥1 Holter monitor studies and were included in the present study. No significant difference was seen in the percentage of patients with ≥1 Holter studies among the CHD types (p = 0.32). Atrial arrhythmias (p <0.01), pacemakers (p <0.01), and the use of antiarrhythmic medications (p <0.01) were more frequent in the d-TGA after Mustard/Senning and Fontan cohorts than in the TOF cohort.
| Total (n = 245) | TOF (n = 134) | d-TGA (n = 44) | Fontan (n = 67) | p Value | |
|---|---|---|---|---|---|
| Patient demographics | |||||
| Number with Holter study | 189 (77%) | 100 (75%) | 38 (86%) | 51 (76%) | 0.32 |
| Age ∗ (yrs) | 27 ± 7.8 | 26.9 ± 8.3 | 28 ± 5.9 | 26 ± 7.9 | 0.38 |
| Female gender | 113 (45%) | 67 (49%) | 16 (35%) | 30 (44%) | 0.26 |
| Electrophysiologic and clinical characteristics | |||||
| Atrial fibrillation or flutter | 44 (18%) | 4 (3%) | 14 (32%) | 26 (39%) | <0.01 |
| Supraventricular tachycardia † | 7 (3%) | 5 (4%) | 1 (2%) | 1 (1%) | 0.87 |
| Pacemaker | 26 (11%) | 5 (4%) | 9 (20%) | 12 (18%) | <0.01 |
| Defibrillator | 22 (9%) | 15 (11%) | 1 (2%) | 6 (9%) | 0.16 |
| Ventricular tachyarrhythmias | 20 (8%) | 14 (10%) | 3 (7%) | 3 (4%) | 0.3 |
| Cardiac transplantation | 2 (1%) | 0 (0%) | 1 (2%) | 1 (1%) | 0.21 |
| Antiarrhythmic medication | 38 (16%) | 3 (2%) | 14 (32%) | 21 (31%) | <0.01 |
| Cardiac arrest | 5 (2%) | 3 (2%) | 0 (0%) | 2 (3%) | 0.71 |
| History of syncope | 17 (7%) | 11 (8%) | 4 (9%) | 2 (3%) | 0.3 |
∗ Patient age at Holter study.
† Not atrial fibrillation or flutter but including atrioventricular re-entrant tachycardia, atrioventricular nodal tachycardia, and focal atrial tachycardia.
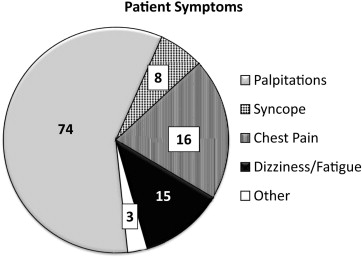
A total of 589 ambulatory monitor studies reviewed ( Table 2 ). Most studies were ordered for screening in asymptomatic patients (80%) and not diagnosis in symptomatic patients. For the 20% of Holter studies ordered for symptom evaluation, the most common symptom was palpitations followed by chest pain ( Figure 1 ). Of the Holter studies ordered because of symptoms, 44 patients (38%) reported some type of symptom during their study. Of these 44 patients, only 1 (<1%) had a significant arrhythmia (atrial flutter) during monitoring that was associated with their symptoms. The remaining 43 patients who had reported any symptom during monitoring had symptoms associated with sinus rhythm or single premature atrial or ventricular complexes. When stratified by individual clinical symptom type, the percentage of patients with clinical symptoms during monitoring was 37% with palpitations, 50% with chest pain, and 0% with syncope.
| Variable | Patient Age at Study (y) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All Studies | TOF | Senning/Mustard | Fontan | ||||||||||
| Total | <18 | 18–25 | >25 | Total | <18 | 18–25 | >25 | Total | <18 | 18–25 | >25 | ||
| Patient (n) | 190 | 101 | 64 | 58 | 21 | 38 | 25 | 27 | 15 | 51 | 31 | 24 | 16 |
| Holter (n) | 589 | 290 | 150 | 101 | 39 | 151 | 62 | 65 | 24 | 148 | 84 | 37 | 27 |
| Holter indication | |||||||||||||
| Symptomatic | 117 (20%) | 56 (19%) | 32 (21%) | 14 (14%) | 10 (26%) | 24 (16%) | 6 (10%) | 10 (15%) | 8 (33%) | 37 (25%) | 18 (21%) | 8 (22%) | 11 (41%) |
| Asymptomatic | 472 (80%) | 234 (81%) | 118 (79%) | 87 (86%) | 29 (74%) | 127 (84%) | 56 (90%) | 55 (85%) | 16 (67%) | 111 (75%) | 66 (79%) | 29 (78%) | 16 (59%) |
| Findings that changed management | 22 (4%) | 5 (2%) | 0 (0%) | 2 (2%) | 3 (8%) | 8 (5%) | 2 (3%) | 3 (5%) | 3 (13%) | 9 (6%) | 2 (2%) | 3 (8%) | 4 (15%) |
| Atrial arrhythmias | |||||||||||||
| Frequent premature atrial complexes | 44 (7%) | 16 (6%) | 10 (7%) | 2 (2%) | 2 (5%) | 17 (11%) | 9 (15%) | 6 (9%) | 2 (8%) | 11 (7%) | 2 (2%) | 1 (3%) | 8 (30%) |
| Couplets triplets | 119 (20%) | 40 (14%) | 17 (11%) | 9 (9%) | 14 (36%) | 47 (31%) | 16 (26%) | 22 (34%) | 9 (38%) | 32 (22%) | 14 (17%) | 5 (14%) | 13 (48%) |
| Nonsustained tachycardia | 40 (7%) | 10 (3%) | 3 (2%) | 4 (4%) | 3 (8%) | 21 (14%) | 5 (8%) | 11 (17%) | 5 (21%) | 9 (6%) | 2 (2%) | 2 (5%) | 5 (19%) |
| Sustained tachycardia | 6 (1%) | 3 (1%) | 1 (1%) | 0 (0%) | 2 (5%) | 2 (1%) | 2 (3%) | 0 (0%) | 0 (0%) | 1 (1%) | 0 (0%) | 0 (0%) | 1 (4%) |
| Ventricular arrhythmias | |||||||||||||
| Frequent premature ventricular contractions | 54 (9%) | 34 (12%) | 11 (7%) | 12 (12%) | 11 (28%) | 9 (6%) | 3 (5%) | 4 (6%) | 2 (8%) | 11 (7%) | 2 (2%) | 4 (11%) | 5 (19%) |
| Couplets triplets | 130 (22%) | 71 (2%) | 25 (17%) | 26 (26%) | 20 (51%) | 41 (27%) | 17 (27%) | 14 (22%) | 10 (42%) | 18 (12%) | 8 (10%) | 6 (16%) | 3 (11%) |
| Nonsustained tachycardia | 18 (3%) | 10 (3%) | 2 (1%) | 3 (3%) | 5 (10%) | 6 (4%) | 1 (2%) | 2 (3%) | 3 (13%) | 2 (1%) | 0 (0%) | 1 (3%) | 1 (4%) |
| Sustained tachycardia | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Second-degree atrioventricular block | 14 (2%) | 10 (3%) | 9 (6%) | 1 (1%) | 0 (0%) | 2 (1%) | 2 (3%) | 0 (0%) | 0 (0%) | 2 (1%) | 1 (1%) | 1 (3%) | 0 (0%) |
| Sinus node disease | 83 (14%) | 2 (1%) | 2 (1%) | 0 (0%) | 0 (0%) | 53 (42%) | 22 (35%) | 27 (42%) | 4 (17%) | 28 (19%) | 19 (23%) | 6 (16%) | 3 (11%) |
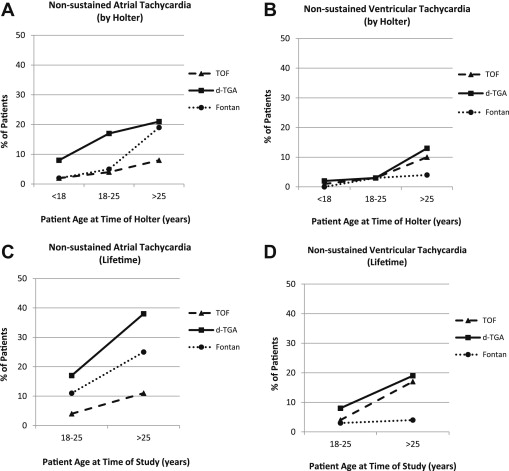
Atrial ectopy was relatively frequent for all CHD types, with the most prevalent finding frequent premature atrial complexes and atrial couplets or triplets, and the frequency of atrial ectopy increased with age ( Figure 2 ). Ventricular ectopy was also relatively common and also increased with age. No patient in the present study demonstrated sustained ventricular arrhythmias during ambulatory monitoring.
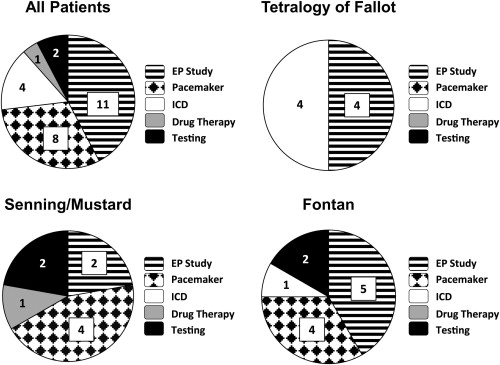
Clinically significant studies, those that directly affected a change in management, were relatively rare, although the occurrences increased with increasing patient age at the time of study. This varied somewhat with the type of underlying CHD, with only 5 of 290 studies (2%) in the TOF after repair cohort, 8 of 151 in the d-TGA after Mustard/Senning cohort (5%), and 9 of 148 in the Fontan cohort (6%) leading to a clinical change in management. Of the 22 Holter studies that changed clinical management, 10 occurred after previously normal Holter findings. The most common Holter-directed changes in management were an invasive electrophysiologic study and pacemaker implantation, although this varied according to the underlying CHD type ( Figure 3 ). None of the 150 studies performed in patients <18 years old in the TOF cohort led to a clinically significant change in management.
Overall, of the 589 Holter studies performed, 22 led to a change in management, for a cost per clinically significant study of $12,732. This cost was affected by CHD type, with a cost per significant study in the TOF after repair cohort of $27,579, >3 times that in the d-TGA after Mustard/Senning cohort ($8,976) and Fontan cohort ($7,821). Patient age also affected the cost per clinically significant study, with a cost of $4,281 for patients >25 years old compared to a cost of $35,187 for those <18 years. The greatest cost was seen in the younger age groups of the TOF after repair cohort, which had no studies that changed management for patients <18 years and only 2 of 251 for those aged <25 years, for a cost per significant Holter study of $59,679.
Most patients (74%) had undergone multiple studies that were similar across the CHD cohorts ( Table 3 ). The percentage of patients with ≥1 studies deemed clinically significant was small (5%). Within this small cohort, findings resulting in a change in management were greater in the patients aged ≥25 years for the TOF after repair and d-TGA after Mustard/Senning cohorts and in those patients aged <25 years in the Fontan population.
| Variable | Patient age at study (y) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All Patients | TOF | Senning/Mustard | Fontan | |||||||||
| Total | 18–25 | >25 | Total | 18–25 | >25 | Total | 18–25 | >25 | Total | 18–25 | >25 | |
| Holters per patient (n) | ||||||||||||
| Any | 189 | 92 | 97 | 100 | 53 | 47 | 38 | 12 | 26 | 51 | 27 | 24 |
| One | 49 | 18 | 31 | 26 | 9 | 17 | 8 | 2 | 6 | 15 | 7 | 8 |
| Multiple | 140 | 74 | 66 | 74 | 44 | 30 | 30 | 10 | 20 | 36 | 20 | 16 |
| Holter indication | ||||||||||||
| Symptomatic | 39 (21%) | 19 (21%) | 20 (21%) | 17 (17%) | 9 (17%) | 8 (17) | 8 (21%) | 1 (8%) | 7 (27%) | 14 (27%) | 9 (33%) | 5 (21%) |
| Asymptomatic | 150 (79%) | 73 (79%) | 77 (79%) | 83 (83%) | 44 (83%) | 39 (83) | 30 (79%) | 11 (92%) | 19 (73%) | 37 (73%) | 18 (67%) | 19 (79%) |
| Findings that changed management | 10 (5%) | 4 (4%) | 6 (6%) | 2 (2%) | 0 (0%) | 2 (4%) | 4 (11%) | 1 (8%) | 3 (12%) | 4 (8%) | 3 (11%) | 1 (4%) |
| Clinical arrhythmia | 51 (27%) | 13 (14%) | 38 (39%) | 17 (17%) | 3 (6%) | 14 (30%) | 14 (37%) | 5 (42%) | 9 (35%) | 20 (39%) | 5 (19%) | 15 (63%) |
| Atrial arrhythmias | ||||||||||||
| Frequent premature atrial complexes | 27 (14%) | 11 (12%) | 16 (16%) | 9 (9%) | 5 (9%) | 4 (9%) | 10 (26%) | 4 (33%) | 6 (23%) | 8 (16%) | 2 (7%) | 6 (25%) |
| Couplets triplets | 68 (36%) | 26 (28%) | 42 (43%) | 28 (28%) | 13 (25%) | 15 (32%) | 21 (55%) | 5 (42%) | 16 (62%) | 19 (37%) | 8 (30%) | 11 (46%) |
| Nonsustained tachycardia | 28 (15%) | 7 (8%) | 21 (22%) | 7 (7%) | 2 (4%) | 5 (11%) | 12 (32%) | 2 (17%) | 10 (38%) | 9 (18%) | 3 (11%) | 6 (25%) |
| Sustained tachycardia | 4 (2%) | 1 (1%) | 3 (3%) | 2 (2%) | 0 (0%) | 2 (4%) | 1 (3%) | 1 (8%) | 0 (0%) | 1 (2%) | 0 (0%) | 1 (4%) |
| Ventricular arrhythmias | ||||||||||||
| Frequent premature ventricular contractions | 39 (21%) | 19 (21%) | 20 (21%) | 25 (25%) | 14 (26%) | 11 (23%) | 7 (18%) | 1 (8%) | 6 (23) | 7 (14%) | 4 (15%) | 3 (13%) |
| Couplets triplets | 76 (40%) | 32 (35%) | 44 (45%) | 44 (44%) | 20 (38%) | 24 (51%) | 18 (47%) | 5 (42%) | 13 (50) | 14 (27%) | 7 (26%) | 7 (29%) |
| Nonsustained tachycardia | 18 (10%) | 4 (4%) | 14 (14%) | 10 (10%) | 2 (4%) | 8 (17%) | 6 (16%) | 1 (8%) | 5 (19) | 2 (4%) | 1 (3%) | 1 (4%) |
| Sustained tachycardia | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0) | 0 (0%) | 0 (0%) | 0 (0%) |
| Second-degree atrioventricular block | 12 (6%) | 9 (10%) | 3 (3%) | 8 (8%) | 7 (13%) | 1 (2%) | 2 (5%) | 1 (8%) | 1 (4) | 2 (4%) | 1 (4%) | 1 (4%) |
| Sinus node disease | 34 (18%) | 17 (18%) | 17 (18%) | 2 (2%) | 2 (4%) | 0 (0%) | 18 (47%) | 7 (58%) | 11 (42) | 14 (27%) | 8 (29%) | 6 (25%) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


