Degraded by shear stress, loss of high-molecular-weight multimers of von Willebrand factor (VWF) correlates strongly with pressure gradient in aortic stenosis (AS) and obstructive hypertrophic cardiomyopathy (HC). We assessed VWF tests before and after interventions in HC and contrasted the severity of abnormalities in HC to patients with AS, mitral regurgitation, and left ventricular assist devices. Ninety patients with median (interquartile range) age 66 (53 to 72) years, 51% men, with HC had assessments of 3 VWF parameters and B-type natriuretic peptide before and after 26 discreet medical/pacing interventions, 22 alcohol septal ablations, and 28 ventricular septal myectomies. VWF multimers were abnormal in 87% of patients with obstructive HC versus 48% of patients with latent obstruction (p = 0.0001). VWF measurements correlated with peak instantaneous left ventricular outflow tract gradient, Spearman ρ 0.51 to 0.61, p <0.0001. For B-type natriuretic peptide, correlation with left ventricular outflow tract gradient was weaker, ρ = 0.37, p = 0.0005, but stronger with septal thickness or mitral E/e’. In pre-/post-medical treatment of HC, VWF multimers were abnormal in 73%/68% of patients, p = 0.74; pre-/post-septal ablation 74%/26%, p = 0.0035; and pre-/post-septal myectomy 75%/0%, p <0.0001. In obstructive HC, the degree VWF multimer loss was greater than in severe AS or severe mitral regurgitation and overlapped that seen in left ventricular assist devices. In conclusion, VWF activity indexes were predictably abnormal in patients with HC with resting obstruction to a degree where bleeding could be anticipated, accurately reflected gradient changes after intervention, and demonstrated complete normalization after septal myectomy.
Among the future research needs highlighted by the 2011 hypertrophic cardiomyopathy (HC) guidelines was the evaluation of therapies to directly modify HC pathophysiology. Termed a “biological sensor of blood flow,” von Willebrand factor (VWF) elongates under high shear stress from 146 to 774 nm resulting in proteolytic loss of the highest molecular weight multimers. This phenomenon is present in most patients with HC with resting obstruction, and reports of bleeding and gastrointestinal angiodysplasia in a manner similar to that described in aortic stenosis (AS) or left ventricular assist device (LVAD) therapy suggest that in some patients, the degree of VWF disruption is not only a marker of gradient severity but an important pathophysiological manifestation of the disease entity. The quantitative relation between pressure gradient and VWF disruption suggests the possibility that VWF tests could reflect the natural history of progression in HC, accurately reflect responses to medical treatment or septal reduction therapy, and possibly predict prognosis. In this study, we examined the relation of peak pressure gradient to VWF function before and after discrete treatment interventions in HC and compared these with results seen with the standard HC biomarker B-type natriuretic peptide (BNP). In addition, we compared the severity of VWF disruption with other cardiac disorders in which VWF abnormalities are known to be associated with bleeding from acquired von Willebrand syndrome.
Methods
From August 2010 to July 2015, we recruited consenting patients with HC who were referred for clinically indicated echocardiography. The protocol allowed inclusion of data in patients with HC obtained for the clinical indication of bleeding during the same period. Clinical data including symptoms, concomitant medical problems, prescribed medications, physical findings, electrocardiogram, and chest radiology studies were recorded. Patients were excluded if they had inadequate echocardiographic images for diagnosis of HC, decreased research blood sampling, were receiving thienopyridenes, or had a hemoglobin <8 g/dl at the time of research blood draw. The protocol was approved by the Mayo Foundation Institutional Review Board. This study was registered at www.clinicaltrials.gov as # NCT01334801 . The outcome of patients with bleeding associated with HC has been reported separately.
The diagnosis of HC was based on findings of septal thickness >13 mm (women) or >15 mm (men). Left ventricular outflow tract maximal instantaneous velocities were recorded, and peak instantaneous gradient was calculated by the Bernoulli equation. Patients in whom the peak gradient at rest was >30 mm Hg were considered to have obstructive HC, whereas those with resting gradient ≤30 mm Hg at rest but >30 mm Hg with provocation (Valsalva maneuver, exercise, amyl nitrite, isoproterenol) were considered to have latent obstruction.
Qualitative loss of high-molecular-weight VWF multimers was assessed from Western blot gel electrophoresis, and VWF activity and antigen were measured from citrated frozen plasma samples as previously described. Quantitative assessment was done by dividing the ratio of bands >15 mers by bands 2 to 15, VWF multimer ratio, and also reported as a normalized multimer ratio, dividing the VWF multimer ratio of the patient by the control plasma from the same gel, as described by van Belle et al. Whole blood platelet function analyzer testing was performed with the PFA-100 (Siemens USA, Deerfield, Illinois), an established screening test for von Willebrand disease, which measures whole blood clotting time when forced through an aperture containing collagen. Collagen plus adenosine diphosphate (PFA-100, Co:ADP) and collagen plus epinephrine (PFA-100, Co:EPI) were used. Because the PFA-100, Co:EPI value is sensitive to aspirin therapy, the PFA-100, Co:EPI results were eliminated from analysis. Normal values from our laboratory for PFA-100, Co:ADP are 57 to 121 seconds. We have previously discussed the differences and relative merits of these 3 VWF activity indexes in the high shear setting of AS.
The Biosite BNP immunoenzymatic assay was performed on a Beckman Coulter DX1800. Normal values for this assay are age and gender adjusted; thus, the upper limit of normal (ULN) for our study varied in each patient, and we analyzed both BNP and normalized BNP (BNP/ULN) as has been previously reported in patients with AS.
Baseline characteristics of patients are presented as median (interquartile range [IQR]). Differences in baseline continuous variables in patients with resting obstruction versus labile obstruction were assessed using the Wilcoxon rank-sum test and nominal variables using Fisher’s exact test. Correlation of continuous variables was examined using the Spearman rank correlation coefficients. In comparing VWF indexes among patients with HC with reference groups, AS, mitral regurgitation (MR), and LVAD therapy, the data are presented as mean ± standard deviation. Ten normal control patients were also studied. The number of controls was based on the highly significant differences noted in VWF indexes between patients with severe AS and normally functioning aortic valve replacement, with group sizes of 30 and 21, respectively.
Results
Baseline data of the patients are presented in Table 1 for the overall group and for patients with resting obstruction or latent obstruction. There were highly significant differences in VWF functional assays and BNP between patients with HC with resting obstruction and latent obstruction, and significant differences between normal controls and patients with latent obstruction ( Table 2 ). Correlations with peak gradient and peak velocity were stronger for the VWF indexes than for BNP ( Table 3 ). In contrast, BNP or BNP/ULN correlated with septal thickness and E/e’.
| Variable | Total (n=90) | Obstructive (n=62) | Latent (n=28) | Control (n=10) |
|---|---|---|---|---|
| Age (years) | 66(53−72) | 66(57–72) | 60(46-72) | 48(35−53) |
| Male | 51% | 44% | 71% | 40% |
| Hypertension | 59% | 61% | 53% | 15% |
| Atrial fibrillation | 24% | 21% | 32% | 0 |
| Heart failure | 8% | 10% | 4% | 0 |
| Defibrillator | 8% | 5% | 11% | 0 |
| On aspirin | 41% | 34% | 54% | 20% |
| Septal thickness, (mm) | 16 (14-20) | 17 (15-20) | 15 (12-20) | |
| Peak gradient, rest (mm Hg) | 44 (22-69) | 54 (39-76) | 18 (12-24) | |
| Peak gradient, Valsalva (mm Hg) | 76 (54-97) | 88 (64-112) | 54 (34-75) | |
| Hemoglobin (mg/dl) | 13.1(11.6−14.6) | 12.0(11.2−14.1) | 14.0(13.0-15.0) | 13.8(13.0−15.1) |
| Creatinine (mg/dl) | 0.9(0.8−1.2) | 1.0(0.8−1.1) | 1.0(0.9-1.2) | 0.8(0.8−0.9) |
| NYHA class III/IV | 42% | 45% | 36% | |
| Heart rate (bpm) | 66(59−74) | 67(60−74) | 63(58-71) | 76(65−79) |
| Variable | Total (n=90) | Obstructive HC (n=62) | P, Obstructive Versus Latent HC | Latent HC (n=28) | P, Latent HC Versus Control | Control (n=10) |
|---|---|---|---|---|---|---|
| Abnormal VWF multimers | 64/87, 74% | 53/61, 87% | 0.0001 | 13/28, 48% | 0.008 | 0/10 |
| Abnormal PFA | 64/88, 73% | 50/61, 82% | 0.0044 | 14/28, 50% | 0.056 | 1/10, 10% |
| Abnormal VWF activity/ antigen | 41/82, 50% | 36/58, 62% | 0.0018 | 6/26, 23% | 0.157 | 0/10 |
| BNP abnormal | 71/83, 86% | 51/55, 93% | 0.0001 | 13/27, 48% | 0.007 | 0/10 |
| Peak Gradient | p | Peak Velocity | p | ||
|---|---|---|---|---|---|
| PFA | 0.51 | <0.0001 | PFA | 0.51 | <0.0001 |
| VWF Ag | 0.26 | 0.02 | VWF Ag | 0.26 | 0.02 |
| VWF Act | 0.14 | 0.21 | VWF Act | 0.13 | 0.24 |
| Act/Ag | -0.57 | <0.0001 | Act/Ag | -0.57 | <0.0001 |
| NMR 15 | -0.57 | <0.0001 | NMR 15 | -0.57 | <0.0001 |
| NMR 10 | -0.61 | <0.0001 | NMR 10 | -0.62 | <0.0001 |
| BNP | 0.37 | 0.0005 | BNP | 0.38 | 0.0005 |
| BNP/ULN | 0.26 | 0.02 | BNP/ULN | 0.24 | 0.03 |
| Septal Thickness | p | LV Mass Index | p | ||
|---|---|---|---|---|---|
| PFA | 0.19 | 0.07 | PFA | 0.16 | 0.16 |
| VWF Ag | -0.26 | 0.02 | VWF Ag | -0.1 | 0.39 |
| VWF Act | -0.29 | 0.01 | VWF Act | -0.13 | 0.26 |
| Act/Ag | -0.1 | 0.38 | Act/Ag | -0.21 | 0.06 |
| NMR 15 | -0.15 | 0.16 | NMR 15 | -0.24 | 0.03 |
| NMR 10 | 0.15 | 0.16 | NMR 10 | -0.29 | 0.009 |
| BNP | 0.26 | 0.02 | BNP | 0.29 | 0.01 |
| BNP/ULN | 0.44 | <0.0001 | BNP/ULN | 0.37 | 0.001 |
| E/e’ | p | LA Volume Index | p | ||
|---|---|---|---|---|---|
| PFA | 0.29 | 0.008 | PFA | 0.23 | <0.04 |
| VWF Ag | 0.36 | 0.001 | VWF Ag | 0.01 | 0.93 |
| VWF Act | 0.2 | 0.08 | VWF Act | 0.02 | 0.87 |
| Act/Ag | -0.48 | <0.0001 | Act/Ag | -0.11 | 0.35 |
| NMR 15 | -0.37 | 0.0007 | NMR 15 | -0.29 | 0.008 |
| NMR 10 | -0.37 | 0.0007 | NMR 10 | -0.41 | 0.0001 |
| BNP | 0.52 | <0.0001 | BNP | 0.34 | 0.002 |
| BNP/ULN | 0.34 | 0.002 | BNP/ULN | 0.35 | 0.002 |
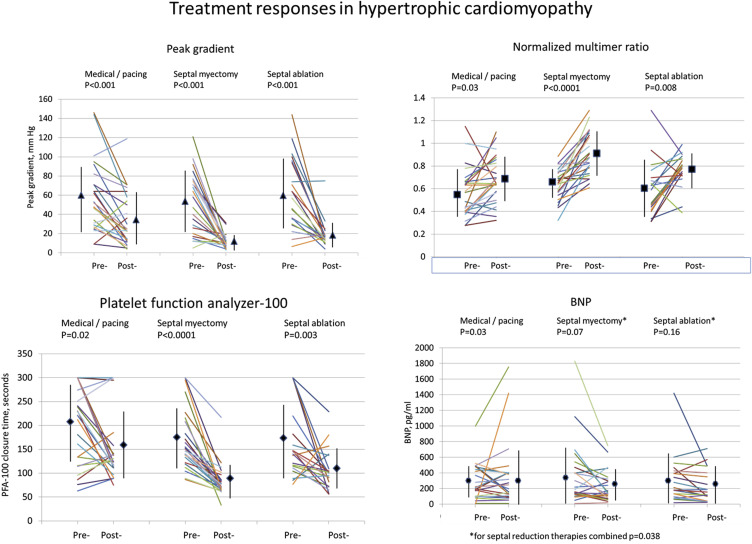
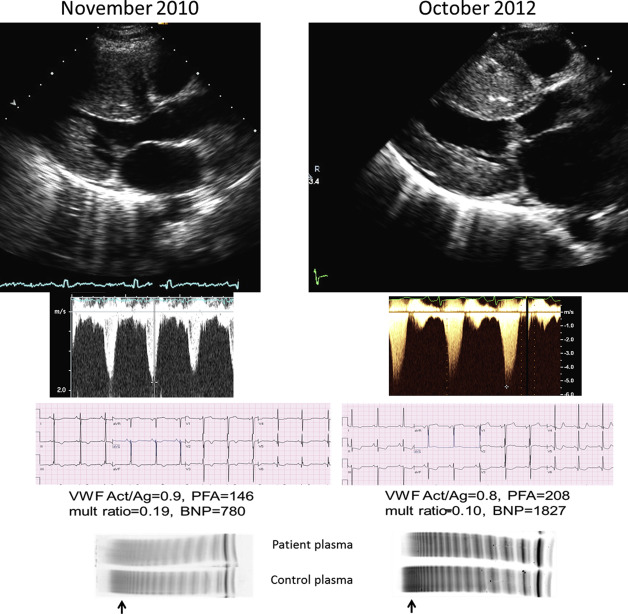
An example of rapid disease progression occurred in a patient with mutations in 2 myosin-binding protein C genes ( Figure 1 ), and the change in VWF variables reflected the hemodynamic progression. His values normalized after septal myectomy. Overall, 24 patients underwent 26 discreet medical or pacing interventions aimed at reducing LVOT gradient, including initiation or uptitration of β blocker in 13, initiation of disopyramide in 5, verapamil in 1, and pacemaker/defibrillator atrioventricular delay adjustment in 6 patients. Twenty-two patients underwent alcohol septal ablation and 28 surgical septal myectomy. The characteristics of the patients with medical or septal reduction therapies were similar except that patients undergoing myectomy were significantly younger. Follow-up blood samples were not available or mishandled in processing in 1 patient in the medical/pacing group, 3 in the septal ablation group, and 4 in the myectomy group. For medical intervention, alcohol septal ablation, and septal myectomy, the interval between the first and follow-up blood samples was, median (IQR), 82 (27 to 191) days, 209 (86 to 319) days, and 182 (99 to 323) days, respectively.
Medical/pacing interventions, although associated with highly significant reductions in echocardiographic gradient ( Figure 2 ), were not associated with normalization of VWF multimers ( Table 4 ), although the quantitative assessment of normalized multimer ratio and PFA-100 revealed small but significant improvement in VWF function. Moreover, medical/pacing interventions were associated with a small but significant increase in BNP. Alcohol septal ablation significantly but not completely normalized VWF multimers, whereas septal myectomy normalized VWF multimers in all patients ( Table 4 , Figure 2 ), and all quantitative VWF indexes were improved by both types of septal reduction therapy. It is notable that myectomy was associated with improved VWF function in all patients studied, whereas the results of septal ablation were not as consistent. Not shown in Figure 2 is the change in VWF activity/antigen which showed trends or slightly significant improvement in the ratio in all 3 treatment groups. There were also borderline significant reductions in BNP by both myectomy and septal ablation, and in combination, septal reduction therapy was associated with a modest reduction of BNP ( Figure 2 ).