Cardiac resynchronization therapy (CRT) reduces mortality and morbidity in selected patients with heart failure (HF), but up to 1/3 of patients are nonresponders. Sum absolute QRST integral (SAI QRST) recently showed association with mechanical response on CRT. However, it is unknown whether SAI QRST is associated with all-cause mortality and HF hospitalizations in patients undergoing CRT. The study population included 496 patients undergoing CRT (mean age 69 ± 10 years, 84% men, 65% left bundle branch block [LBBB], left ventricular ejection fraction 23 ± 6%, 63% ischemic cardiomyopathy). Preimplant digital 12-lead electrocardiogram was transformed into orthogonal XYZ electrocardiogram. SAI QRST was measured as an arithmetic sum of areas under the QRST curve on XYZ leads and was dichotomized based on the median value (302 mV ms). All-cause mortality served as the primary end point. A composite of 2-year all-cause mortality, heart transplant, and HF hospitalization was a secondary end point. Cox regression models were adjusted for known predictors of CRT response. Patients with preimplant low mean SAI QRST had an increased risk of both the primary (hazard ratio [HR] 1.8, 95% CI 1.01 to 3.2) and secondary (HR 1.6, 95% CI 1.1 to 2.2) end points after multivariate adjustment. SAI QRST was associated with secondary outcome in subgroups of patients with LBBB (HR 2.1, 95% CI 1.5 to 3.0) and with non-LBBB (HR 1.7, 95% CI 1.0 to 2.6). In patients undergoing CRT, preimplant SAI QRST <302 mV ms was associated with an increased risk of all-cause mortality and HF hospitalization. After validation in another prospective cohort, SAI QRST may help to refine selection of CRT recipients.
Cardiac resynchronization therapy (CRT) is an established treatment for patients with systolic heart failure (HF) and electrical dyssynchrony. Despite established benefits, approximately 1/3 of patients demonstrate a lack of response after CRT, framing the continued need to refine selection for this beneficial but nonetheless costly therapy.
In keeping with the expected benefit of reversing electrical dyssynchrony and delayed activation of the lateral left ventricular (LV) wall, there has been increasing interest in identifying electrical markers of dyssynchrony as predictors of outcome in patients undergoing CRT. For example, contemporary data have suggested that the benefits of CRT accrue primarily to patients with significantly (>150 ms) prolonged QRS duration and those with a left bundle branch block (LBBB) morphology. In addition to these standard measures of electrical conduction (QRS duration and morphology), sum absolute QRST integral (SAI QRST) was recently shown to be associated with LV reverse remodeling in patients undergoing CRT. Analysis of SmartDelay Determined AV Optimization: A Comparison to Other AV Delay (SMART-AV) clinical trial data showed that high pre-CRT SAI QRST has been associated with a higher likelihood of mechanical response (measured as a reduction in LV end-systolic volume 6 months after CRT), whereas low baseline SAI QRST values has predicted mechanical nonresponse. However, it remained unknown whether pre-CRT SAI QRST can predict clinical outcomes (mortality and HF hospitalizations). We, therefore, conducted retrospective cohort study and hypothesized that a low SAI QRST would be associated with an increased risk of adverse clinical outcomes. In addition, given the established use of standard electrocardiographic markers in predicting response to CRT, we also examined the prognostic value of SAI QRST in prespecified subgroups defined by QRS duration and BBB morphology.
Methods
We conducted a retrospective cohort study and included consecutive patients receiving CRT implants (cardiac resynchronization therapy defibrillator [CRT-D] or cardiac resynchronization therapy pacemaker [CRT-P]) from 1999 to 2012 at a large volume tertiary care center in Sweden. Inclusion criteria were HF with dilated or ischemic cardiomyopathy, optimal pharmacologic HF treatment and QRS duration ≥120 ms, meeting standard guideline criteria for CRT implantation. All baseline data were gathered from an individual assessment of medical records by the same investigators (JJ and CR). Ischemic cardiomyopathy was diagnosed if there was a history of myocardial infarction or coronary revascularization or if the patient had verified coronary artery disease and the clinical evaluation had indicated ischemic cardiomyopathy. Patients with “nonstandard” CRT indication or with failed CRT implant were excluded, as were patients without available digital baseline (preimplant) electrocardiogram (ECG). The study complies with the Declaration of Helsinki and was approved by the local ethics committee.
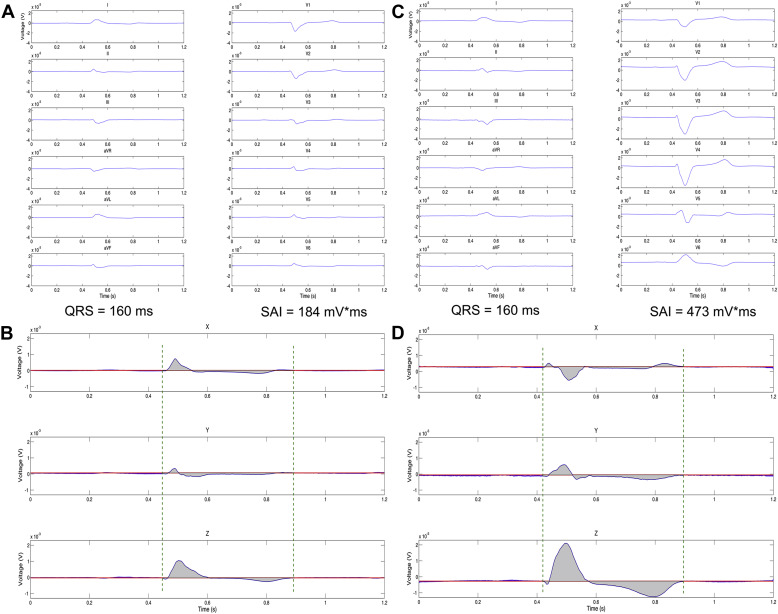
A 12-lead ECG was collected before CRT device implantation in all subjects and stored digitally in the hospital ECG database. Digital electrocardiographic data were exported from the local MUSE database (GE health care, Chicago, IL, USA) in xml. file format. All electrocardiographic files were deidentified and sent to an independent core laboratory for analysis. ECG analysis was performed by investigators (EG, MK, and LGT) blinded to the study outcomes and the patients’ clinical characteristics. Customized Matlab (MathWorks, Inc, Natick, Massachusetts) software was used, and the digitized 12-lead electrocardiographic signal was transformed into 3-dimensional orthogonal XYZ ECG using an inverse Dower transformation matrix ( Figure 1 ). The median beat was used for analysis. The absolute value of the area under the entire QRST waveform was calculated for each orthogonal lead (X, Y, and Z). Absolute QRST integral values on X, Y, and Z leads were then added together to obtain averaged SAI QRST.
The primary outcome was an all-cause mortality. A composite end point of all-cause death, heart transplant, or HF hospitalization, whichever came first, served as a secondary end point. End points were extracted from a review of the medical record with cross validation using the Swedish Pacemaker Registry and the Swedish Death and Hospital Discharge Registries.
Continuous variables are reported as mean ± SD unless otherwise specified. The SAI QRST variable was dichotomized using the median value. The Pearson chi-square test or Fisher’s exact test were used to compare categorical variables, as appropriate. Unadjusted Kaplan–Meier survival analysis was used. The log-rank statistic was computed to test the equality of survival distributions in participants with SAI QRST above and below the median value. Multivariate Cox regression analysis was performed to determine the association of SAI QRST with outcomes, after adjustment for clinically relevant confounders, which associated with outcome in univariate analysis at p value <0.2. Association of SAI QRST with outcomes was tested in the subgroups of participants with LBBB versus non-LBBB; and patients with QRS duration ≥150 ms versus and <150 ms. A p value of <0.05 was considered statistically significant. SPSS 22.0 (IBM SPSS Statistics for Windows, version 22.0; IBM Corp, Armonk, New York) was used for data analysis.
Results
Of 705 eligible CRT-implanted patients, 496 had a digital ECG stored before the procedure, and these patients were included in the study. About 2/3 of study population received CRT-P, and only 1/3, CRT-D devices. The median SAI QRST value was 302 mV ms. The baseline characteristics of the study population stratified by median SAI QRST are presented in Table 1 . Patients with SAI QRST below the median were more likely to have ischemic cardiomyopathy, an atypical intraventricular conduction block on ECG, diabetes, and a narrower QRS duration preimplant.
| Variable | All Patients n = 496 | SAI QRST (mV*ms) | P-Value | |
|---|---|---|---|---|
| <302 (n = 249) | ≥302 (n = 247) | |||
| Age at implant (years) | 69±10 | 69±10 | 70±10 | 0.14 |
| Women | 16% | 14% | 17% | 0.39 |
| Ischemic cardiomyopathy | 63% | 72% | 53% | <0.001 |
| Left Ventricular Ejection Fraction (%) | 23±6 | 24±6 | 23±7 | 0.16 |
| QRS duration (ms) | 169±28 | 158±24 | 180±27 | <0.001 |
| Electrocardiographic morphology | ||||
| Left bundle branch block | 65% | 61% | 69% | 0.06 |
| Right bundle branch block | 2% | 1% | 2% | 0.34 |
| Intraventricular conduction delay | 13% | 20% | 5% | <0.001 |
| Paced QRS | 20% | 17% | 24% | 0.07 |
| NYHA class (mean±SD) | 2.9±0.5 | 2.9±0.5 | 2.9±0.5 | 0.28 |
| S-Creatinine (mg/dL) | 1.32±0.51 | 1.35±0.55 | 1.29±0.47 | 0.27 |
| Hypertension | 38% | 36% | 41% | 0.31 |
| Diabetes mellitus | 35% | 42% | 28% | 0.001 |
| History of atrial fibrillation | 49% | 51% | 48% | 0.47 |
| Previous stroke / TIA | 11% | 10% | 11% | 0.48 |
| Loop diuretic treatment | 91% | 91% | 91% | 1 |
| Beta-blocker | 84% | 81% | 86% | 0.27 |
| ACEi/ARB | 93% | 94% | 92% | 0.72 |
| Upgrade from previous PM/ICD | 20% | 17% | 24% | 0.09 |
| Cardiac resynchronization therapy defibrillator | 35% | 39% | 31% | 0.09 |
During the 2-year follow-up period, there were 113 deaths (68 in the low SAI QRST group and 40 in the high SAI QRST group), 5 heart transplants (4 and 1, respectively), and 226 patients experienced the combined end point of death, heart transplant, or HF hospitalization (140 and 86, respectively).
In unadjusted Kaplan–Meier analysis, SAI QRST was associated with the primary and secondary outcomes ( Figure 2 ). In univariate Cox regression analysis ( Table 2 ), SAI QRST below 302 mV ms was associated with about twice higher mortality. After adjustment for age, gender, type of cardiomyopathy, New York Heart Association (NYHA) class, QRS duration and morphology, presence of atrial fibrillation, co-morbidities (creatinine and diabetes), HF medical management (diuretics, angiotensin-converting enzyme inhibitors [ACEis]/angiotensin II receptor blockers [ARBs]), and type of CRT (with or without defibrillator), the association attenuated only slightly.
| Variable | Univariable Cox Regression | Multivariable Cox Regression | ||||
|---|---|---|---|---|---|---|
| HR | 95 CI | P-Value | HR | 95 CI | P-Value | |
| Age at implant (years) | 1.04 | 1.02-1.07 | <0.001 | 1.03 | 0.99-1.06 | 0.09 |
| Ischemic cardiomyopathy | 12.2 | 1.4-3.4 | 0.001 | 1.4 | 0.71-2.7 | 0.33 |
| Women | 0.61 | 0.34-1.1 | 0.11 | |||
| LVEF (%) | 0.99 | 0.97-1.0 | 0.63 | |||
| QRS duration (ms) | 0.99 | 0.99-1.0 | 0.17 | |||
| Left bundle branch block | 0.75 | 0.51-1.1 | 0.13 | |||
| NYHA class | 2.6 | 1.7-3.9 | <0.001 | 2.4 | 1.4-4.1 | 0.01 |
| S-Creatinine (mg/dL) | 2.0 | 1.5-2.6 | <0.001 | 1.3 | 0.92-1.8 | 0.15 |
| Diabetes mellitus | 11.4 | 0.95-2.0 | 0.09 | |||
| Atrial fibrillation | 1.6 | 1.1-2.4 | 0.01 | 0.88 | 0.51-1.5 | 0.65 |
| Previous stroke / TIA | 2.3 | 0.76-2.2 | 0.35 | |||
| Loop diuretic treatment | 2.2 | 0.90-5.4 | 0.09 | |||
| Beta-blocker | 0.75 | 0.47-1.2 | 0.23 | |||
| ACEi/ARB | 0.31 | 0.18-0.52 | <0.001 | 0.37 | 0.18-0.75 | 0.006 |
| Cardiac resynchronization therapy defibrillator | 0.58 | 0.38-0.90 | 0.01 | 0.82 | 0.45-1.5 | 0.52 |
| SAI QRST <302mV*ms | 1.9 | 1.3-2.8 | 0.001 | 1.8 | 1.0-3.2 | 0.048 |
Similarly, an SAI QRST below 302 mV ms was associated with 70% higher risk of the composite HF outcome ( Table 3 ). The association between SAI QRST and secondary outcome persisted after multivariate adjustment ( Table 3 ) including age, type of cardiomyopathy, QRS duration and conduction abnormality (LBBB vs non-LBBB), HF severity (left ventricular ejection fraction and NYHA class), co-morbidities (diabetes, atrial fibrillation, and creatinine level), HF medical management (use of ACEi, ARB, and diuretics), and type of CRT (CRT-P vs CRT-D).
| Variable | Univariable Cox Regression | Multivariable Cox Regression | ||||
|---|---|---|---|---|---|---|
| HR | 95 CI | P-Value | HR | 95 CI | P-Value | |
| Age at implant (years) | 1.01 | 1.0-1.02 | 0.16 | 1.02 | 0.99-1.0 | 0.11 |
| Ischemic cardiomyopathy | 1.6 | 1.2-2.1 | 0.002 | 1.1 | 0.78-1.6 | 0.56 |
| Women | 1 | 0.74-1.5 | 0.78 | |||
| Left ventricular ejection fraction (%) | 0.98 | 0.96-1.0 | 0.09 | 0.97 | 0.95-1.0 | 0.03 |
| QRS duration (ms) | 0.99 | 0.99-1.0 | 0.01 | 0.998 | 0.99-1.0 | 0.54 |
| Left bundle branch block | 0.79 | 0.61-1.0 | 0.08 | 0.928 | 0.62-1.4 | 0.715 |
| NYHA class | 2.4 | 1.7-3.3 | <0.001 | 1.6 | 1.2-2.2 | 0.003 |
| S-Creatinine (mg/dL) | 1.5 | 1.2-1.9 | 0.001 | 1.3 | 1.00-1.7 | 0.047 |
| Diabetes mellitus | 1.3 | 1.0-1.7 | 0.03 | 1.3 | 0.97-1.8 | 0.08 |
| Atrial fibrillation | 1.3 | 1.0-1.7 | 0.02 | 1.1 | 0.82-1.5 | 0.46 |
| Previous stroke / TIA | 1.1 | 0.77-1.7 | 0.51 | |||
| Loop diuretic treatment | 2.3 | 1.2-4.1 | 0.009 | 2.2 | 1.2-4.3 | 0.02 |
| Beta-blocker | 0.73 | 0.53-1.0 | 0.064 | |||
| ACEi/ARB | 0.65 | 0.41-1.0 | 0.07 | 0.75 | 0.41-1.4 | 0.36 |
| Cardiac resynchronization therapy defibrillator | 0.88 | 0.67-1.21 | 0.36 | 1.02 | 0.99-1.0 | 0.11 |
| SAI QRST <302mV*ms | 1.7 0 | 1.4-2.1 | <0.001 | 1.6 0 | 1.1-2.2 0 | 0.01 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


