B-type natriuretic peptide (BNP) level may be a useful prognostic marker for the management of asymptomatic patients with aortic stenosis (AS). The aim of this study was to identify the echocardiographic determinants of BNP changes during follow-up in AS. We studied 61 asymptomatic patients with greater than moderate AS and preserved left ventricular (LV) ejection fraction who underwent rest and exercise Doppler echocardiography with concomitant BNP level measurement at baseline. BNP measurement was repeated after inclusion every 6 months. Patients were divided into 2 groups according to the median of BNP changes during follow-up. According to parameters at rest, patients in the high BNP changes group had significantly higher E/e′ ratio. Statistically significant correlations were found between BNP changes and E/e′ ratio and indexed left atrial area. According to exercise parameters, patients in the high BNP changes group had significantly lower exercise-induced increase in LV ejection fraction. Statistically significant correlations were found between BNP changes and exercise-induced changes in LV ejection fraction. After adjustment for age, mean aortic pressure gradient, and BNP level at baseline, multivariate analysis identified indexed left atrial area, E/e′ at rest, and exercise-induced increase in ejection fraction as independent determinants of BNP changes during follow-up. In conclusion, this study shows that, in asymptomatic patients with preserved LV function and moderate AS, serial BNP measurements may widely vary. Subclinical LV diastolic and systolic dysfunctions are frequently present in patients with higher serial BNP changes.
Aortic stenosis (AS) is the most common valvular heart disease. Risk stratification of asymptomatic patients with AS and preserved left ventricular ejection fraction (LVEF) remains challenging. In clinical practice, the risk-benefit ratio of early surgery should be carefully evaluated, and aortic valve replacement might be discussed in asymptomatic patients considered at high risk. Exercise echocardiography has been shown to provide incremental prognostic information beyond echocardiography at rest or exercise testing alone, even in patients with moderate AS. B-type natriuretic peptide (BNP) is probably the biomarker most frequently measured in AS; it is predominantly secreted by ventricular cardiac myocytes in response to increased wall stress. Recent European Society of Cardiology guidelines have suggested elective BNP level measurement for individual risk stratification in asymptomatic AS. Of note, interest has recently grown in terms of serial BNP measurements for better prediction of outcome in patients with valvular heart disease, with a more accurate predictive power than elective measurements. However, in AS, little is known about longitudinal changes in BNP levels during serial assessments. The aims of the present study were (1) to prospectively describe the individual changes in BNP levels during longitudinal follow-up of asymptomatic patients with AS and preserved LVEF and (2) to identify whether these changes were related to the presence of baseline left ventricular (LV) systolic and/or diastolic dysfunction.
Methods
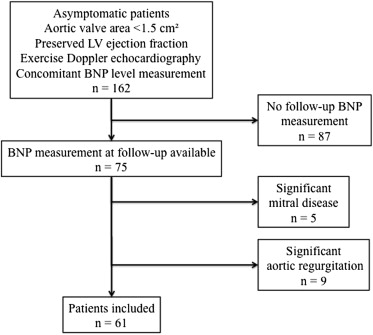
We prospectively screened 162 consecutive asymptomatic patients with at least moderate AS (aortic valve area <1.5 cm²) and preserved LVEF (i.e., >50%) who were referred to our Heart Valve Clinic to perform both resting and exercise Doppler echocardiography with concomitant BNP level measurement ( Figure 1 ). Sixty-one patients met the inclusion criteria and had a BNP measurement repeated after at least 6 months of follow-up and then after each 6 or 12 months, according to the individual management. A careful history evaluation and exercise testing confirmed asymptomatic status. The following clinical characteristics were collected: age, body surface area, gender, dyslipidemia (cholesterol-lowering medications or low-density lipoprotein cholesterol >115 mg/dl), systemic arterial hypertension (antihypertensive medications or blood pressure >140/90 mm Hg), diabetes mellitus (oral hypoglycemic medications, insulin, or glycemia >126 mg/dl), current smoking, coronary artery disease (history of myocardial infarction or documented coronary artery stenosis), atrial fibrillation, and chronic renal insufficiency. The relevant institutional review boards approved the protocol, and all patients gave written informed consent.
Before the exercise test, comprehensive transthoracic Doppler echocardiographic examination at rest was performed with a General Electric Vingmed Vivid 9 ultrasound system (Horten, Norway). The acquisitions were stored on a dedicated workstation for subsequent off-line analysis (EchoPAC; General Electric Healthcare, Little Chalfont, United Kingdom). LV stroke volume was calculated by multiplying the LV outflow tract area by the LV outflow tract velocity-time integral measured by pulse-wave Doppler. LV end-diastolic and end-systolic volumes, as well as ejection fraction, were measured by the biapical Simpson disk method. Intraobserver and interobserver variabilities, in our echocardiography laboratory, for exercise-induced changes in LVEF using Simpson’s biplane method were previously assessed and reported. The peak E-wave and A-wave velocities of the mitral inflow were measured using pulse-wave Doppler. Tissue Doppler imaging with pulse-wave Doppler at the level of septal and lateral mitral annulus was used to measure e′. The average of septal and lateral mitral annulus e′ peak velocity was used to calculate the E/e′ ratio. AS severity was evaluated using continuous-wave Doppler to measure the aortic transvalvular maximal velocities, and subsequent peak and mean gradients were calculated using the simplified Bernoulli equation. Aortic valve area was calculated using the continuity equation. Left atrial area was obtained by planimetry of an end-systolic frame from the apical 4-chamber view. All measures were indexed to body surface area.
A symptom-limited graded bicycle exercise test was performed with an initial workload of 25W and an increase of 25W every 2 minutes in a semisupine position using a tilt table. A 12-lead electrocardiography was monitored continuously, and blood pressure was measured at rest and every 2 minutes during exercise. The test result was considered abnormal if the patient presented one of the following criteria: limiting dyspnea at low workload (i.e., during the 2 first steps of exercise), angina, syncope or near-syncope, increase in blood pressure of <20 mm Hg, ≥2 mm ST-segment depression, or complex ventricular arrhythmias. By design, none of the patients studied presented a positive stress test. At peak exercise, the following echocardiographic parameters were measured: AS severity (peak velocity, mean pressure, and indexed valve area), LV systolic (indexed stoke volume and ejection fraction) and diastolic function (E/e′ ratio) parameters.
Venous blood samples for BNP level measurement were drawn at rest before echocardiography. Chilled ethylenediaminetetraacetic acid–treated tubes were centrifuged immediately at 4,000 rpm (4°C) for 15 minutes. Separated plasma samples were processed by immunofluorescence assay (Biosite, Beckman Coulter, San Diego, California). The inter- and intra-assay variations were 5% and 4%, respectively. The assay detection limit was 1 pg/ml. BNP changes were calculated as the difference between the last BNP measurement obtained during the follow-up and the baseline BNP measurement at inclusion:
BNP changes ( pg / ml ) = Last BNP at follow-up − Baseline BNP at inclusion
Annualized BNP changes ( pg/ml/year ) = ( Last BNP at follow-up − Baseline BNP at inclusion ) Time of follow-up
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


