The aim of the study was to assess the impact of atrial fibrillation (AF) on outcome in patients who underwent mitral valve repair (MVRp) for mitral valve prolapse (MVP). Four hundred and forty-three consecutive patients underwent MVRp for organic mitral regurgitation due to MVP. Echocardiography was performed preoperatively and after surgery. Postoperative left ventricular dysfunction (LVD) was defined as left ventricular ejection fraction (LVEF) <50%. Before surgery, 187 patients (42%) had preoperative AF. After surgery, LVEF significantly decreased from 67 ± 9% to 56 ± 10% (p <0.0001). Compared with patients in sinus rhythm (SR), those in AF were significantly older (p <0.0001), had more severe symptoms (p = 0.004), had lower LVEF (p = 0.002), and higher EuroSCORE (p = 0.05). Compared with patients in SR, patients with AF had significantly lower 10-year survival (64 ± 4% vs 83 ± 3%, p = 0.001). On multivariate analysis, preoperative AF was identified as an independent predictor of overall mortality (hazard ratio 1.67; 95% confidence interval 1.15 to 2.42; p = 0.007). At 10 years, patients with paroxysmal AF had lower survival and higher heart failure rate than patients in SR (78 ± 3% vs 66 ± 6%) but had a better outcome compared with those with permanent AF (66 ± 6% vs 53 ± 6%, p = 0.022). Patients with AF had a significantly higher rate of postoperative LVD (23.3% vs 13.4%, p = 0.007). In conclusion, preoperative AF is a predictor of long-term mortality and postoperative LVD after MVRp for MVP. To improve postoperative outcome, surgery in these patients should be performed before onset of AF.
Atrial fibrillation (AF) is a common arrhythmia in conservatively managed organic chronic mitral regurgitation (MR). Previous studies have reported that the prevalence of AF in patients who underwent mitral valve surgery varies from 20% to 55%. It is widely accepted that, when feasible, mitral valve repair (MVRp) is the procedure of choice in patients with severe organic MR. The current American College of Cardiology/American Heart Association (ACC/AHA) and European Society of Cardiology (ESC) guidelines recommend surgery in the presence of symptoms or left ventricular dysfunction (LVD)/dilatation (class I recommendation). Mitral surgery may also be considered when patients have developed AF. Thus, the occurrence of AF is an ACC/AHA and ESC class IIa recommendation with a low level of evidence (B and C respectively). Actually, conflicting data have been reported regarding the impact of preoperative AF on outcome after mitral valve surgery. In a Mayo Clinic study including patients with degenerative mitral valve prolapse (MVP) in sinus rhythm (SR) at baseline, an increase in cardiac mortality after onset of AF was observed under conservative management. Conversely, some data have shown that preoperative AF had no significant impact on early or late mortality after MVRp. Moreover, the impact of preoperative AF (i.e., permanent or paroxysmal) on the risk of cardiac postoperative LVD has been suggested. The present study sought to analyze in patients who underwent MVRp for MVP (1) the prognostic value of preoperative permanent and paroxysmal AF on long-term mortality and (2) the association between preoperative AF and occurrence of LVD.
Methods
From January 1, 1991, to December 31, 2012, 443 consecutive patients who underwent MVRp for organic MR because of leaflet prolapse at our institution were included in this study. All patients had complete preoperative and postoperative echocardiographic evaluation. Preoperative echocardiography was defined as echocardiography performed 3 months before surgery, and postoperative echocardiography was defined as echocardiography performed 9 to 12 months after surgery.
Exclusion criteria were (1) MR caused by ischemic heart disease or dilated cardiomyopathy, rheumatic heart disease, active infective endocarditis, and congenital heart disease; (2) previous cardiac surgery; (3) concomitant aortic valve or aortic root surgery; (4) patients with history of myocardial infarction or recent acute coronary syndrome; and (5) patients with concomitant maze procedure or any surgical treatment of AF.
Baseline clinical characteristics, co-morbidity, symptoms, and operative data were collected from patients’ medical records. The standard logistic EuroSCORE was calculated retrospectively for each patient using the calculator available online at www.euroscore.org . All patients underwent preoperative electrocardiogram, and chronic and paroxysmal AF were defined as recommended by current ACC/AHA guidelines. Institutional review board authorization was obtained before initiation of the study. The study was conducted in accordance with institutional policies, national legal requirements, and the revised Declaration of Helsinki. Diagnoses of leaflet prolapse and flail leaflets were identified according to the recommended criteria. LV dimensions were assessed from parasternal long-axis views by 2-dimensional–guided M-mode using the leading edge methodology at end-diastole and end-systole. Left ventricular ejection fraction (LVEF) was estimated by the Simpson biplane method or visually. Preoperative LVD was defined as an LVEF <60%. Two-dimensional echocardiography-guided diameter was measured with M-mode at end-systole in the parasternal long-axis view, according to the method proposed by the American Society of Echocardiography. Pulmonary artery systolic pressure was estimated using the simplified Bernoulli equation (4 × tricuspid valve regurgitation velocity) plus the estimated right atrial pressure.
Study end points were perioperative mortality, overall mortality (i.e., including perioperative and mortality after hospital discharge), postoperative LVD (defined as LVEF <50%), and a composite of all-cause death and heart failure. Perioperative mortality was defined as death occurring within 30 days after surgery or longer if the patient was hospitalized for a longer duration. Mean duration of follow-up was 8.7 ± 5.3 years (median: 8.6 years; twenty-fifth to seventy-fifth percentiles: 4.4 to 12.5 years). During follow-up, patients were monitored by their personal general practitioners or cardiologists. Events were ascertained by review of medical records and clinical interviews or by telephone calls to physicians, patients, and (when necessary) next of kin. Normally distributed continuous variables were expressed as mean ± SD. Categorical variables were summarized as frequency percentages and absolute numbers. Comparisons between groups were performed with the Student t tests or chi-square tests, as appropriate. Variables not normally distributed were expressed as median (interquartile range). Survival curves were plotted according to the Kaplan-Meier method, and differences between groups were compared with the log-rank test. For multivariate analyses, an epidemiologic approach was adopted, and the following variables were entered in multivariate analyses: New York Heart Association class, logistic EuroSCORE, and preoperative AF. Multivariate logistic regression analysis was performed to evaluate predictors of postoperative LVD. Multivariate Cox proportional hazard analyses were performed to investigate predictors of death during follow-up. A p value of 0.05 was considered significant for all statistical tests. Data were analyzed with SPSS 17.0 (SPSS Inc., Chicago, Illinois).
Results
Posterior leaflet prolapse was the most common mitral valve abnormality (69%, n = 307), 6% of patients had anterior leaflet prolapse (n = 27), and 25% (n = 109) had prolapse involving both leaflets. Thirteen percent of patients (n = 56) had associated coronary artery bypass graft surgery. Demographic, clinical, and echocardiographic data according to the presence of preoperative AF are presented in the Table 1 . One hundred eighty-seven patients (42%) had preoperative AF. These patients were significantly older, had a higher logistic EuroSCORE, greater left atrial (LA) diameter, and lower LVEF than patients in SR. Patients with AF also had more severe symptoms. Digoxin, warfarin, and amiodarone were prescribed significantly more frequently in patients with AF ( Table 1 ).
| Characteristics | Overall study population | Sinus rhythm | Atrial fibrillation | p value |
|---|---|---|---|---|
| (n=443) | (n=256) | (n=187) | ||
| Age (years) | 65.4 ± 11.1 | 63.1 ± 11.5 | 68.5 ± 9.7 | <0.0001 |
| Men | 316 (71.3%) | 191 (74.6%) | 125 (66.8%) | 0.074 |
| NYHA | 0.004 | |||
| I | 51 (11.5%) | 35 (13.7%) | 16 (8.6%) | |
| II | 174 (39.3%) | 113 (44.1%) | 61 (32.6%) | |
| III | 162 (36.6%) | 84 (32.8%) | 78 (41.7%) | |
| IV | 56 (12.6%) | 24 (9.4%) | 32 (17.1%) | |
| Height (cm) | 170.8 ± 8.8 | 171.1 ± 8.5 | 170.4 ± 9.2 | 0.481 |
| Weight (kg) | 74.6 ± 14.6 | 75.0 ± 13.9 | 74.0± 15.6 | 0.552 |
| Heart rate (bpm) | 75.3 ± 16.0 | 74.0 ± 13.8 | 77.2 ± 18.5 | 0.062 |
| Logistic EuroSCORE | 3.2 ± 3.6 | 3.0 ± 3.0 | 3.6 ± 4.2 | 0.050 |
| Hypertension | 168 (38.3%) | 95 (37.7%) | 73 (39.0%) | 0.775 |
| Diabetes mellitus | 29 (6.6%) | 15 (6.0%) | 14 (7.5%) | 0.522 |
| Echocardiography data | ||||
| Left atrial diameter (mm) | 49.3 ± 8.6 | 47.4 ± 7.3 | 51.5 ± 9.5 | <0.0001 |
| LV end-diastolic diameter (mm) | 61.3 ± 6.6 | 61.2 ± 6.2 | 61.4 ± 7.2 | 0.745 |
| LV end-systolic diameter (mm) | 36.8 ± 6.9 | 36.2 ± 6.7 | 37.6 ± 7.2 | 0.057 |
| Ejection fraction (%) | 67.3 ± 9.1 | 68.5 ± 8.9 | 65.7 ± 9.2 | 0.002 |
| MR grade | 0.375 | |||
| II | 5 (1.1%) | 3 (1.2%) | 2 (1.1%) | |
| III | 170 (39%) | 106 (41.7%) | 64 (35.2%) | |
| IV | 261 (59.9%) | 145 (57.1%) | 116 (63.7%) | |
| Prolapse site | 0.701 | |||
| Anterior | 27 (6.1%) | 14 (5.5%) | 13 (7.0%) | |
| Posterior | 307 (69.3%) | 381 (70.7%) | 126 (67.4%) | |
| Both leaflets | 109 (24.6%) | 61 (23.8%) | 48 (25.7%) | |
| Pulmonary artery systolic pressure ∗ (mmHg) | 46.4 ± 14.6 | 45.9 ± 14.7 | 46.9 ± 14.4 | 0.538 |
| Therapy | ||||
| Angiotensin receptor blockers | 27 (6.6%) | 15 (6.5%) | 12 (6.7%) | 0.941 |
| Angiotensin conversion enzyme inhibitors | 232 (56.4%) | 126 (54.3%) | 106 (59.6%) | 0.267 |
| Beta blockers | 132 (31.9%) | 68 (29.2%) | 64 (35.4%) | 0.181 |
| Digoxin | 73 (17.6%) | 5 (2.1%) | 68 (37.6%) | <0.0001 |
| Warfarin | 156 (36.8%) | 23 (9.6%) | 133 (71.9%) | <0.0001 |
| Antiplatelet | 82 (20.1%) | 43 (18.2%) | 39 (22.7%) | 0.277 |
| Calcium blocker | 82 (20.2%) | 42 (17.9%) | 40 (23.4%) | 0.171 |
| Diuretic | 158 (38.3%) | 79 (33.2%) | 79 (45.4%) | 0.012 |
| Amiodarone | 65 (16.0%) | 26 (11.1%) | 39 (22.8%) | 0.002 |
| Cardiopulmonary bypass time (minutes) | 135.6 ± 40.3 | 135.9±41.5 | 135.2 ± 38.7 | 0.872 |
| Aortic cross clamp time (minutes) | 94.7 ± 25.2 | 94.5 ± 24.2 | 95.0 ± 26.5 | 0.832 |
| Concomitant coronary bypass | 56 (12.7) | 33 (12.9) | 23 (12.3) | 0.841 |
Of the 187 patients with preoperative AF, 101 had permanent AF and 86 had only paroxysmal AF. Compared with those with paroxysmal AF, patients with permanent AF were significantly older (71 ± 9 vs 66 ± 9 years, p = 0.001), had higher logistic EuroSCORE (4.3 ± 5.3 vs 2.9 ± 2.4, p = 0.024), greater LA diameter (54 ± 10 vs 48 ± 9 mm, p = 0.001), higher heart rate (82 ± 22 vs 72 ± 13 beats/min, p = 0.001), and lower LVEF (64 ± 10% vs 68 ± 8%, p = 0.007).
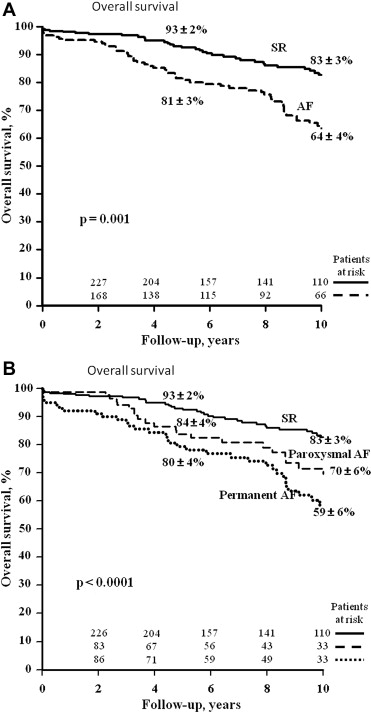
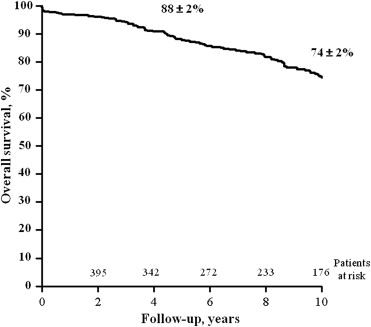
The perioperative mortality rate (2%, n = 9) was similar between patients with preoperative AF and those in SR (2.7% vs 1.6%, p = 0.41). Overall, 117 deaths (26.5%) occurred during follow-up resulting in 10-year overall survival of 74 ± 2% ( Figure 1 ).
Among the 187 patients with preoperative AF, 66 died during follow-up (25 had paroxysmal AF before surgery and 41 presented permanent AF). In univariate analysis, postoperative 10-year overall survival was significantly better in patients in SR compared with those with AF ( Figure 2 ). On multivariate analysis, AF (hazard ratio [HR] 1.67, 95% confidence interval [CI] 1.15 to 2.42; p = 0.007) was identified as an independent predictor of postoperative overall mortality. Further adjustment for LVEF (HR 1.75, 95% CI 1.20 to 2.53; p = 0.003), LV end-systolic diameter (1.81, 95% CI 1.22 to 2.68; p = 0.003), or coronary artery bypass (HR 1.68, 95% CI 1.16 to 2.43; p = 0.006) did not influence this independent relation. The 10-year overall survival in patients with permanent AF and in those with paroxysmal AF was significantly lower compared with patients in SR (both p <0.0001) ( Figure 2 ). However, in patients with AF, postoperative overall survival in patients with permanent AF compared with those with paroxysmal AF tended to be lower (p = 0.091).