The 2 predominant causes of ventricular tachycardia (VT) arising from the right ventricle are arrhythmogenic right ventricular cardiomyopathy (ARVC) and idiopathic VT arising from the right ventricular outflow tract (RVOT). These arrhythmias can be adrenergically mediated and may be difficult to distinguish clinically. A minor criterion for the diagnosis of ARVC is T-wave inversion (TWI) in the right precordial leads during sinus rhythm. However, there have been reports of precordial TWI identified in patients with RVOT tachycardia. The purpose of this study was to determine whether patterns of precordial TWI could differentiate between the 2 groups. A multicenter registry of 229 patients with VT of right ventricular origin was evaluated. After appropriate exclusions (n = 29), 79 patients (58% men, mean age 40 ± 14 years) had ARVC, and 121 patients (41% men, mean age 48 ± 14 years) had RVOT tachycardia. During sinus rhythm, 37 patients (47%) with ARVC and 5 patients (4%) with RVOT tachycardia had TWI in leads V 1 to V 3 . For the diagnosis of ARVC, TWI in leads V 1 to V 3 had sensitivity of 47% and specificity of 96%. In conclusion, in patients with VT of right ventricular origin, the presence of TWI in electrocardiographic leads V 1 to V 3 supports the diagnosis of ARVC.
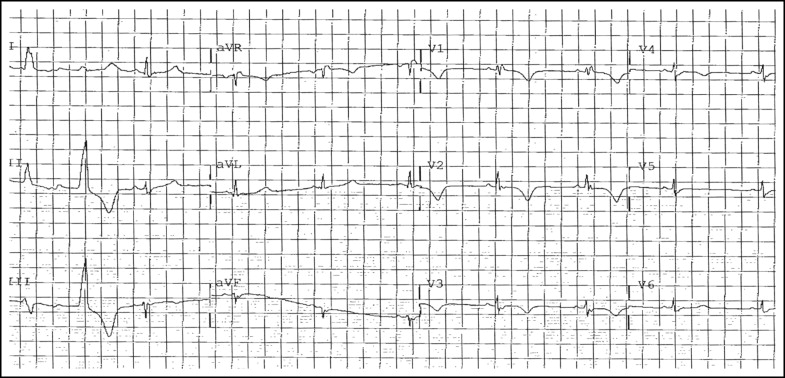
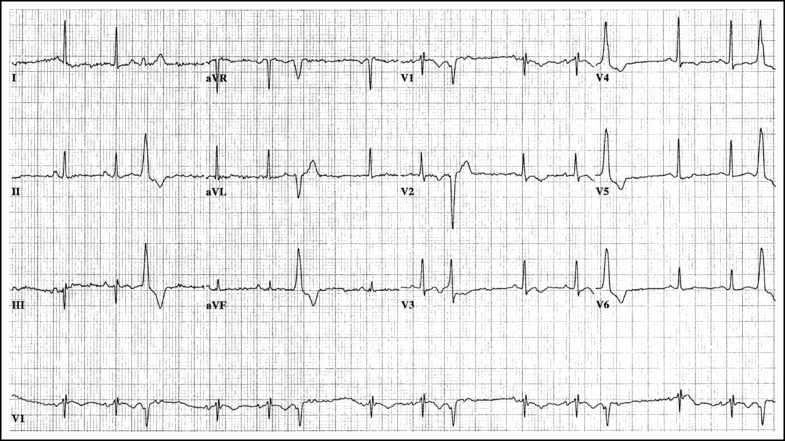
The 2 predominant causes of ventricular tachycardia (VT) arising from the right ventricle are arrhythmogenic right ventricular (RV) cardiomyopathy (ARVC) or dysplasia and idiopathic VT arising from the RV outflow tract (RVOT). Discrimination between these 2 entities is critical, because their prognoses and therapeutic options differ. T-wave inversion (TWI) in the right precordial leads, as seen in Figure 1 , is a minor criterion for the diagnosis of ARVC and recently has been proposed as a major criterion. However, there have been reports identifying precordial TWI in 6% to 20% of patients with RVOT tachycardia ( Figure 2 ). Previous investigations examining the discriminatory utility of precordial TWI included relatively small numbers of patients and did not examine closely the extent of TWI that could best differentiate ARVC from RVOT. In this study, we used data from a large population of patients with VT of RV origin to determine whether patterns of precordial TWI could differentiate between ARVC and idiopathic RVOT tachycardia.
Methods
We evaluated a multicenter registry of patients with VT of RV origin. The source population was derived from the National Institutes of Health–supported Multidisciplinary Study of Right Ventricular Dysplasia (n = 108) and the Cornell University Medical Center registry of idiopathic VT (n = 121).
The clinical testing used to diagnose the ARVC population has been published. Of the 121 patients with RVOT tachycardia, 115 (95%) had undergone echocardiography, with no findings consistent with ARVC. Of the 62 magnetic resonance imaging tests (51%) performed, 5 showed minor abnormalities, but none was diagnostic of ARVC. None of the 19 endocardial biopsies (16%) was consistent with ARVC, and only 1 of the 13 available signal-averaged electrocardiograms (11%) showed abnormal results. On endocardial mapping, all patients with idiopathic VT had normal RV endocardial voltage and focal sources of VT originating in the RVOT. No patient with RVOT tachycardia met task force criteria for the diagnosis of ARVC, and on follow-up, none was diagnosed as affected by ARVC. No patient with RVOT tachycardia had bundle branch block.
We included only ARVC registry patients who had available 12-lead electrocardiograms without complete bundle branch block (n = 94) and excluded those patients who ultimately were classified as “unaffected” (n = 7). To reduce bias in the analysis of sensitivity, we also excluded ARVC registry patients for whom the presence of TWI was crucial for the diagnosis of ARVC on the basis of task force criteria (n = 8). After exclusions, the population examined consisted of 79 patients with ARVC and 121 patients with RVOT tachycardia. A reader unaware of the diagnoses examined each patient’s sinus rhythm 12-lead electrocardiogram for the presence of TWI in the precordial leads.
All statistical analyses were performed using SPSS version 16.0 for Windows (SPSS, Inc., Chicago, Illinois). Analyses of differences between groups were performed using Student’s t tests for continuous variables and chi-square tests for categorical variables. In all analyses, 2-sided p values <0.05 were considered significant. Continuous variables are expressed as mean ± SD and categorical variables as number (percentage).
Results
Patients with ARVC were younger than those with RVOT tachycardia (40 ± 14 vs 48 ± 14 years, p <0.001) and were more likely to be men (58% vs 41%, p = 0.02). Overall, among the 79 patients with ARVC, no TWI was seen in 15 patients (19%). TWI was observed in lead V 1 in 21 patients (27%), leads V 1 and V 2 in 6 (8%), leads V 1 to V 3 in 12 (15%), leads V 1 to V 4 in 14 (18%), leads V 1 to V 5 in 5 (6%), and leads V 1 to V 6 in 6 (8%). One patient (1%) had TWI limited to leads V 4 to V 6 , and 1 patient (1%) had TWI in lead V 6 only. Among the 121 patients with RVOT tachycardia, no TWI was seen in 40 patients (33%), and TWI was observed in lead V 1 in 62 patients (51%), leads V 1 and V 2 in 13 (11%), leads V 1 to V 3 in 1 (1%), leads V 1 to V 4 in 1 (1%), leads V 1 to V 5 in 1 (1%), and leads V 1 to V 6 in 2 (2%). One patient (1%) had TWI in leads V 5 and V 6 only.
A summary of the extent of right precordial TWI in this population is listed in Table 1 . Thirty-seven of 79 patients (47%) with ARVC and 5 of 121 patients (4%) with RVOT tachycardia had TWI in leads V 1 to V 3 or beyond. As listed in Table 2 , TWI in leads V 1 to V 3 had sensitivity of 47% and specificity of 96% for the diagnosis of ARVC.



