The present study tested whether in patients with type 2 diabetes mellitus (DM) the combination of increased waist circumference and increased plasma triglyceride (TG) levels can predict the presence of coronary artery disease (CAD) as assessed by multidetector computed tomographic coronary angiography (CTA). In 202 patients with type 2 DM who were clinically referred for CTA, waist circumference and TG levels were measured. Patients were divided into 4 groups according to waist circumference measurements and TG levels. Increased waist circumference and TG levels (n = 61, 31%) indicated the presence of the hypertriglyceridemic waist phenotype. Patients with low waist circumference and TG (n = 49, 24%) were considered the reference group. Physical examination and blood measurements were performed. CTA was used to determine presence and severity of CAD. In addition, plaque type was evaluated. Plasma cholesterol levels were significantly increased in the group with increased TG levels and waist circumference, whereas high-density lipoprotein cholesterol was significantly lower than in the reference group. There was a significant increase in the presence of any CAD (odds ratio 3.3, confidence interval 1.31 to 8.13, p <0.05) and obstructive CAD (≥50%, odds ratio 2.9, confidence interval 1.16 to 7.28, p <0.05) in the group with increased TG level and waist circumference. In addition, a significantly larger number of noncalcified and mixed plaques was observed. In conclusion, in patients with type 2 DM, presence of the hypertriglyceridemic waist phenotype translated into a deteriorated blood lipid profile and more extensive CAD on CTA. Accordingly, the hypertriglyceridemic waist phenotype may serve as a practical clinical biomarker to improve risk stratification in patients with type 2 DM.
The aim of the present study was to test whether the hypertriglyceridemic waist phenotype in patients with type 2 diabetes mellitus (DM) can predict the presence of coronary artery disease (CAD) as assessed by multidetector computed tomographic coronary angiography (CTA). A second aim was to assess differences in atherosclerotic plaque characteristics in diabetic patients with and without the presence of hypertriglyceridemic waist phenotype using CTA.
Methods
All patients were asymptomatic and were referred from a routine outpatient diabetes clinic for cardiovascular risk stratification. Patients were diagnosed as having type 2 DM according to American Diabetes Association criteria. As a result, 202 diabetic patients (120 men and 82 women, mean age 54 ± 11 years) were enrolled in the study population. Exclusion criteria for CTA were (1) (supra)ventricular arrhythmias, (2) renal insufficiency (glomerular filtration rate <30 ml/min), (3) known allergy to iodine contrast material, (4) severe claustrophobia, and (5) pregnancy. At physical examination, waist circumference and blood pressure measurements were performed. In addition, blood samples were obtained in the morning after a 12-hour fast. Triglyceride (TG), low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, apolipoprotein B, and C-reactive protein levels were measured.
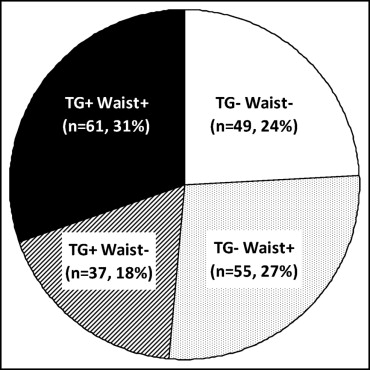
Patients were divided into 4 groups using threshold values for waist circumference measurements (≤88 or >88 cm for women and ≤102 or >102 cm for men) and TG levels (<1.7 or ≥1.7 mmol/L for men and women) as previously described by National Cholesterol Education Program Adult Treatment Panel III. Figure 1 illustrates patient distribution over the 4 groups. Type 2 diabetic patients with a large waist circumference and increased TG levels, signifying the presence of the hypertriglyceridemic waist phenotype, were denoted TG + waist + . Diabetic patients with a small waist circumference and low TG levels were considered the reference group, denoted TG − waist − , to which a CAD odds ratio of 1.0 was designated for comparison purposes.
CT coronary angiographic studies, including calcium scores, were performed using 2 different systems: 64-row CTA (Aquilion 64, Toshiba Medical Systems, Otawara, Japan) and 320-row CTA (Aquilion ONE, Toshiba Medical Systems) with 64 and 320 simultaneous detector rows, respectively (each 0.5-mm wide). Unless contraindicated, oral β-blocker medication (metoprolol 50 or 100 mg) was administered to patients with a heart rate ≥65 beats/min 1 hour before the investigation. The total amount of nonionic contrast medium (Iomeron 400; Bracco, Milan, Italy) injected into the antecubital vein was 60 to 100 ml (depending on body weight and scanner type) at a flow rate of 5.0 or 6.0 ml/s, followed by a saline flush of 25 to 50 ml. To synchronize the arrival of contrast medium, bolus arrival was detected using a real-time bolus-tracking technique. All images were acquired during a single inspiratory breath-hold of maximally 12 seconds. For 64-row CTA, a helical-scanning technique was used, and for 320-row CTA, a volumetric scanning technique was used. Average investigation time for CT acquisition was approximately 20 minutes.
To examine the relation between hypertriglyceridemic waist and CAD in patients with type 2 DM, all CT coronary angiographic scans were evaluated for presence of CAD. CT coronary angiographic reconstructions were transferred to a remote workstation with dedicated analysis software (for 64-row CT coronary angiographic reconstructions: Vitrea 2, Vital Images, Minnetonka, Minnesota; for 320-row CT coronary angiographic reconstructions: Vitrea FX 2.0, Vital Images). Coronary arteries were evaluated using the reconstruction dataset with the fewest motion artifacts, typically acquired during a mid-diastolic phase. When multiple reconstructions from different cardiac phases were available, reconstruction with the best image quality was evaluated. CT coronary angiographic scans were evaluated by 2 experienced observers. Discrepancies in the interpretation of CT coronary angiographic examinations were immediately resolved by consensus. Presence of CAD was assessed by scrolling through axial images, followed by visual assessment of curved multiplanar reconstructions in ≥2 orthogonal planes. Coronary segments, vessels, and patients were classified as having (1) no CAD, (2) nonsignificant CAD (luminal narrowing <50% in diameter), or (3) obstructive CAD (≥50% luminal narrowing), as previously described. Plaque types were determined by scoring plaque in each diseased coronary segment as noncalcified, calcified, or mixed. Calcium score was assessed using dedicated software (Vitrea 2 or Vitrea FX 1.0 for 64-row detector or 320-row detector CTA, respectively). An overall Agatston score was registered for each patient.
Statistical analysis was performed using SPSS 16.0 (SPSS, Inc., Chicago, Illinois). Quantitative data were expressed as mean ± SD and compared between groups using 2-tailed unpaired Student’s t test. Categorical variables were described as numbers and percentages and comparison was performed by chi-square test. Multivariate logistic regression analysis was performed (using backward elimination method) to determine the relation of waist circumference and TG levels to presence of CAD and obstructive CAD, correcting for clinical variables (age, gender, obesity, hypertension, smoking, and family history of CAD). A p value <0.05 was considered statistically significant.
Results
Baseline patient characteristics for the TG + waist + and TG − waist − groups are listed in Table 1 . The TG + waist + group had a significantly larger proportion of women and an increased prevalence of hypertension and obesity compared to the TG − waist − group. Furthermore, clinical baseline measurements were performed ( Table 2 ). Blood pressure measurements and all lipid and cholesterol blood measurements were significantly increased in the TG + waist + group, except high-density lipoprotein cholesterol levels, which were significantly lower in the TG + waist + group. In addition, C-reactive protein levels ≥3.0 mg/L, indicating an increased inflammatory profile, were present in a significantly larger proportion of patients in the TG + waist + group compared to the reference group. However, hemoglobin A 1c , a marker for glycemic control, was not significantly different between the 2 groups.
| TG − waist − | TG + waist + | |
|---|---|---|
| (n = 49) | (n = 61) | |
| Men/women | 37/12 § | 26/34 § |
| Age (years) | 54 ± 10 | 55 ± 10 |
| Known coronary artery disease | 0 | 3 (4.9%) |
| Previous myocardial infarction | 0 | 2 (3.3%) |
| Previous coronary artery bypass grafting | 0 | 1 (1.6%) |
| Previous percutaneous coronary intervention | 0 | 1 (1.6%) |
| Family history of coronary artery disease ⁎ | 21 (43%) | 25 (41%) |
| Hypertension † | 17 (34.7%) § | 44 (72.1%) § |
| Obesity (body mass index ≥30 kg/m 2 ) | 3 (6.1%) § | 37 (60.7%) § |
| Smoking | 10 (20%) | 31 (21%) |
| Medication ‡ | ||
| β Blockers | 3 (7%) | 4 (7%) |
| Diuretics | 4 (9%) § | 14 (25%) § |
| Statins | 21 (49%) | 25 (46%) |
| Calcium-antagonists | 3 (7%) | 10 (19%) |
⁎ Defined as presence of coronary artery disease in first-degree family members at <55 years of age in men and <65 years of age in women.
† Defined as systolic blood pressure ≥140 mm Hg and/or diastolic blood pressure ≥90 mm Hg and/or use of antihypertensive medication.
‡ In 13 patients medication information was not available.
| TG − waist − (n = 49) | TG + waist + (n = 61) | p Value | |
|---|---|---|---|
| Waist circumference (cm) | 89 ± 7.4 | 113 ± 13.8 | <0.001 |
| Triglycerides | |||
| mmol/L | 1.1 ± 0.29 | 3.0 ± 1.53 | <0.001 |
| mg/dl | 97 ± 26 | 266 ± 136 | <0.001 |
| Total cholesterol | |||
| mmol/L | 4.2 ± 0.87 | 5.1 ± 1.04 | <0.001 |
| mg/dl | 162 ± 34 | 197 ± 40 | <0.001 |
| Low-density lipoprotein cholesterol | |||
| mmol/L | 2.6 ± 0.90 | 3.1 ± 0.90 | <0.05 |
| mg/dl | 101 ± 35 | 120 ± 35 | <0.05 |
| High-density lipoprotein cholesterol | |||
| mmol/L | 1.5 ± 0.42 | 1.2 ± 0.45 | <0.05 |
| mg/dl | 58 ± 16 | 46 ± 17 | <0.05 |
| Apolipoprotein B (g/L) | 0.73 ± 0.29 | 0.94 ± 0.27 | <0.001 |
| Hemoglobin A 1c (%) | 7.4 ± 1.3 | 7.8 ± 1.8 | NS |
| C-reactive protein level ≥3.0 mg/L | 21 (35%) | 40 (80%) | <0.001 |
| Systolic blood pressure (mm Hg) | 131 ± 17 | 144 ± 17 | <0.001 |
| Diastolic blood pressure (mm Hg) | 78 ± 8 | 88 ± 10 | <0.001 |
To investigate the relation between the hypertriglyceridemic waist phenotype in patients with type 2 DM and CAD, CTA was performed. There was a significant increase in the presence of CAD in the TG + waist + group compared to the TG − waist − group. In 79% of patients with TG + waist + CAD was present on CT coronary angiogram compared to 55% of patients with TG − waist − (p <0.05). In addition, presence of obstructive CAD was examined on a patient basis. A significant increase in obstructive CAD in the TG + waist + group compared to the TG − waist − group was observed. Obstructive CAD was observed in 43% of patients with TG + waist + compared to 25% of patients with TG − waist − (p <0.05).
Figures 2 and 3 show the results of multivariate logistic regression analysis performed to determine the independent relation between waist circumference and TG levels versus the presence of CAD and obstructive CAD, respectively. The odds ratio of finding any CAD and obstructive CAD were significantly increased in diabetic patients with the hypertriglyceridemic waist phenotype compared to diabetic patients without this phenotype. CT coronary angiographic characteristics of the 2 groups were compared on a coronary segment and vessel basis ( Table 3 ). Patients with TG + waist + had a significantly larger number of narrowed coronary segments and vessels compared to those with TG − waist − . In addition, prevalence of 3-vessel coronary disease was significantly higher in the TG + waist + group. Furthermore, patients with TG + waist + had a significantly larger number of obstructed coronary vessels. Although an increased percent obstructive 3-vessel coronary disease was found in the TG + waist + group compared to the TG − waist − group, the difference was not significant. In addition, patients with TG + waist + had a significantly greater noncalcified and mixed plaque burden compared to the reference group. However, neither number of calcified plaques nor Agatston calcium score was significantly different between the 2 groups ( Table 3 ).




