Cardiorespiratory fitness has often been interpreted as a surrogate measurement of physical activity rather than an independent coronary heart disease (CHD) risk factor per se. Fitness is also known to be highly heritable, however, and rats bred selectively for treadmill endurance have low CHD risk phenotypes even in the absence of physical activity. Therefore, I assessed whether cardiorespiratory fitness predicted CHD independent of physical activity in 29,721 men followed prospectively for 7.7 years as part of the National Runners’ Health Study. Specifically, CHD deaths and incident participant-reported physician-diagnosed myocardial infarction, revascularization procedures (coronary artery bypass grafting and percutaneous coronary intervention), and angina pectoris during follow-up were compared to baseline cardiorespiratory fitness (10-km footrace performance, meters/second). Nonfatal end points for the 80% of these men who provided follow-up questionnaires included 121 nonfatal myocardial infarctions, 317 revascularization procedures, and 81 angina pectora. The National Death Index identified 44 CHD deaths. Per meter/second increment in baseline fitness, men’s risks decreased 54% for nonfatal myocardial infarction (p <0.0001), 44% for combined CHD deaths and nonfatal myocardial infarction (p = 0.0003), 53% for angina pectoris (p = 0.001), and 32% for revascularizations (p = 0.002). Adjustment for physical activity (kilometer/day run) had little effect on the per meter/second risk decreases for nonfatal myocardial infarction (from 64% to 63%), combined CHD deaths and nonfatal myocardial infarction (from 34% to 33%), angina pectoris (from 53% to 47%) or revascularizations (from 32% to 26%). In conclusion, the results suggest that cardiorespiratory fitness is a CHD risk factor, largely independent of physical activity, which warrants clinical screening.
Cardiorespiratory fitness has been shown to predict cardiovascular mortality. In 1989, this conclusion was reaffirmed in the seminal report by Blair et al, but with a twist. They suggested that cardiorespiratory fitness may be a more objective measurement of physical activity than self-reported activity, and they postulated that the substantial cardiovascular disease decreases they observed with greater cardiorespiratory fitness may be achievable by becoming physically more active. However, interpreting cardiorespiratory fitness as only a physical activity surrogate discounts studies that show up to 70% of the variation in aerobic capacity is inherited in humans, and selective breeding for fitness produces substantial inherited differences in coronary heart disease (CHD) risk factors in rats even in the absence of training. If cardiorespiratory fitness affects incident CHD due to physical activity, then there will be greater statistical power for demonstrating this in the National Runners’ Health Study than in other population cohorts because (1) 80% of men provided 10-km footrace performance times, a measurement of cardiorespiratory fitness; (2) vigorous physical activity is recognized as being most effective in increasing maximum aerobic consumption (VO 2 max) ; and (3) the range of energy expenditures is substantially greater than that represented in other cohort studies. Demonstrating that cardiorespiratory fitness predicts lower incident CHD independent of physical activity would argue for its recognition as an independent CHD risk factor that warrants clinical screening and the need for public health recommendations that target improved fitness.
Methods
The National Runners’ Health Study cohort was recruited from 1991 to 1993 by nationwide distribution of a 2-page questionnaire to runners identified through subscription lists to running magazine subscribers and participation in foot race events. The questionnaire solicited information on demographics, running history, weight history, smoking habit, previous heart attacks and cancer, and medication use. To be eligible for the study, participants were required to provide signed informed consent, be ≥18 years old, and provide, at a minimum, their name, contact information, gender, birth date, weekly running distance, body weight, and height. Follow-up questionnaires were mailed from 1998 to 2001. The University of California, Berkeley, committee for the protection of human subjects approved the study protocol and all participants provided written informed consent.
Baseline cardiorespiratory fitness was assessed as speed in meters per second of the participant’s best 10-km race during the previous 5 years (reported as finish time in minutes). Published data support the use of running performance to estimate VO 2 max. Baseline running distances were reported in usual miles run per week, which correlates strongly between repeated questionnaires (r = 0.89), and has been shown to be related to biomarkers traditionally associated with physical activity. Although other leisure-time physical activities were not recorded for this cohort, data from runners recruited after 1998 (when the question was added to the survey) show running represents (mean ± SD) 91.5 ± 19.1% of all vigorously intense activity, and 73.5 ± 23.7% of total leisure-time physical activity.
In their follow-up questionnaires, participants reported whether they had percutaneous transluminal coronary angioplasty or coronary artery bypass grafting, if they had been diagnosed by a physician as having had a heart attack or angina pectoris since baseline, and the year of the procedure or diagnosis. Participants reporting any of these procedures or conditions in the year of their baseline survey or before were excluded from these analyses. Nonfatal CHD was defined as the earliest myocardial infarction, coronary artery bypass grafting, percutaneous transluminal coronary angioplasty, or angina pectoris. Fatal CHD was defined as an International Classification of Disease, Ninth Revision , diagnosis of codes 410 to 414 and 429.2 or an International Classification of Disease, 10th Revision , diagnosis of codes I20 to I25 as provided by the National Death Index. The end point “all fatal and nonfatal CHD” includes fatal and nonfatal CHD as described.
Cox proportional hazard model (JMP 5.0, SAS Institute, Cary, North Carolina) was used with cardiorespiratory fitness (meters per second) as the independent variable and weekly intakes of alcohol, meat, fish, fruit, and aspirin, pack-years of cigarette use, education, and age (age and age squared) as covariates. Results were then adjusted for physical activity (kilometre per day run) to determine whether activity dose explained the association between fitness and incident disease. In addition, effects of adjusting for participant’s recalled weight when they began running ≥12 km/week (body mass index [BMI] before exercise) were used to assess possible effects of self-selection and adjusted for their baseline BMI to assess whether BMI mediated the relation between cardiorespiratory fitness and CHD. Analyses of nonfatal events included only those participants with follow-up questionnaires, whereas analyses of all fatal and nonfatal CHD invoked the assumption that subjects lost to follow-up were free of CHD at the end of follow-up (a conservative approach because it counted nonfatal CHDs as event-free survival in those lost to follow-up).
Results
There were 30,604 men who had complete data on age, education, diet, aspirin use, BMI, smoking history, running distance, and 10-km performance times, of whom 424 were excluded for baseline cigarette use, 159 for baseline diabetes, and 300 for pre-existing heart disease. Of those remaining, follow-up questionnaires were obtained for 23,939 men (80.6%), and causes of death were obtained from the National Death Index in an additional 243 men with complete baseline data who were nonsmokers, nondiabetic, and without pre-existing heart disease at baseline. Men reported physician diagnoses of 125 myocardial infarctions, 317 revascularization procedures (percutaneous transluminal coronary angioplasty or coronary artery bypass grafting), and 81 incident angina pectoris. The National Death Index identified an additional 44 CHD deaths. Women were excluded because only 35 reported CHD, which were too few for meaningful analyses.
Table 1 presents men’s baseline characteristics by 10-km performance. Their participation in follow-up was unrelated to 10-km performance. The fittest men were generally younger, exercised more, consumed somewhat less meat, fish, and alcohol and more fruit, were leaner before starting to exercise and at baseline, and smoked less before baseline. The 10-km footrace performance did not differ between those providing and not providing follow-up questionnaires (p = 0.58). However, those lacking follow-up questionnaires were significantly younger (41.7 ± 0.13 vs 44.6 ± 0.7 years, p <0.0001), less educated (15.92 ± 0.03 vs 16.52 ± 0.02 years, p <0.0001), ran somewhat more (5.80 ± 0.04 vs 5.65 ± 0.02 km/day, p = 0.001), smoked more previously (6.46 ± 0.17 vs 5.76 ± 0.09 pack-years, p = 0.0003), and ate less beef (2.66 ± 0.03 vs 2.82 ± 0.02 serving/week, p <0.0001) at baseline.
| Cardiorespiratory Fitness (10-km footrace performance, m/s) | |||||
|---|---|---|---|---|---|
| <3.25 | 3.25–3.74 | 3.75–4.24 | 4.25–4.74 | ≥4.75 | |
| Total sample size | 2,711 | 7,924 | 10,396 | 6,227 | 2,463 |
| Ischemic heart disease death | 10 | 20 | 8 | 3 | 3 |
| Follow-up questionnaires | |||||
| Number | 2,154 | 6,370 | 8,436 | 5,015 | 1964 |
| Percentage | 79.5 | 80.4 | 81.1 | 80.5 | 79.7 |
| Nonfatal myocardial infarction | 32 | 45 | 39 | 8 | 1 |
| Angina pectoris | 19 | 32 | 22 | 8 | 0 |
| Revascularization procedure | 58 | 127 | 99 | 28 | 5 |
| Running (km/day) ⁎ § | 3.7 ± 2.3 | 4.5 ± 2.3 | 5.6 ± 2.8 | 7.0 ± 3.4 | 9.0 ± 4.4 |
| Age (years) ⁎ | 51.0 ± 11.3 | 47.5 ± 9.7 | 44.0 ± 9.0 | 40.4 ± 8.7 | 34.7 ± 8.6 |
| Education (years) ⁎ † | 16.5 ± 2.5 | 16.4 ± 2.5 | 16.4 ± 2.5 | 16.4 ± 2.4 | 16.2 ± 2.4 |
| Meat intake (servings/week) ⁎ § | 2.9 ± 2.6 | 2.9 ± 2.6 | 2.8 ± 2.6 | 2.6 ± 2.6 | 2.7 ± 2.9 |
| Fish intake (servings/week) ⁎ ‡ | 1.7 ± 1.5 | 1.6 ± 1.5 | 1.5 ± 1.4 | 1.4 ± 1.4 | 1.3 ± 1.4 |
| Fruit intake (pieces/week) ⁎ § | 10.6 ± 8.9 | 10.6 ± 8.7 | 11.0 ± 8.4 | 11.7 ± 9.5 | 11.5 ± 9.4 |
| Alcohol intake (ml/day) ⁎ | 11.7 ± 16.2 | 12.5 ± 17.2 | 11.9 ± 16.3 | 11.0 ± 15.5 | 9.2 ± 15.0 |
| Aspirin (tablets/day) ⁎ | 0.4 ± 0.8 | 0.4 ± 0.7 | 0.4 ± 0.7 | 0.3 ± 0.7 | 0.3 ± 0.6 |
| Cigarettes (pack-years) † § | 11.0 ± 18.9 | 8.2 ± 15.6 | 5.4 ± 11.9 | 3.4 ± 9.0 | 1.3 ± 5.4 |
| Body mass index (kg/m 2 ) | |||||
| Before exercise ⁎ § | 25.9 ± 3.7 | 25.2 ± 3.3 | 24.3 ± 3.4 | 23.1 ± 3.7 | 20.6 ± 4.1 |
| Baseline ⁎ § | 25.5 ± 3.1 | 24.6 ± 2.6 | 23.8 ± 2.3 | 22.9 ± 2.1 | 22.0 ± 1.9 |
⁎ p ≤0.0001 without adjustment for age.
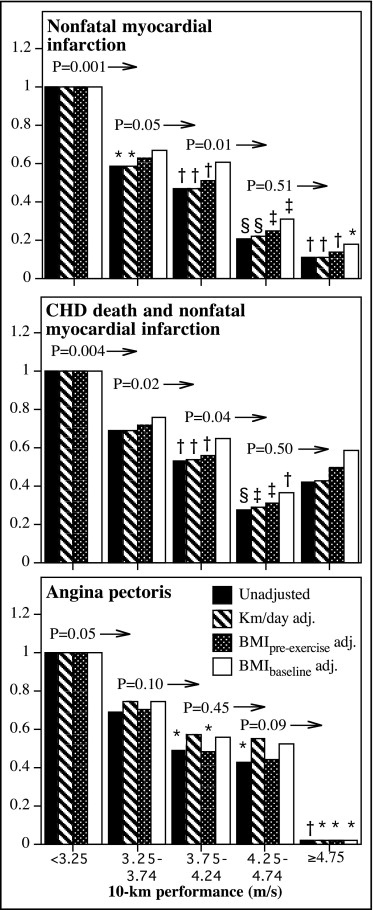
Table 2 presents the hazard ratios for CHD by baseline cardiorespiratory fitness levels. Each meter/second increment in running performance was associated with a 44% lower risk for CHD death and nonfatal myocardial infarction, a 54% lower risk for nonfatal myocardial infarction, a 53% lower risk for angina pectoris, and 32% lower risk for revascularization procedures (percutaneous transluminal coronary angioplasty or coronary artery bypass grafting). Adjustment for physical activity had little effect on the hazard ratios. Fatal CHDs were too few for separate analyses. Adjustment for men’s pre-exercise BMI also had little effect on the hazard ratios, and except for angina pectoris, all remained significant when adjusted for baseline BMI.
| Hazard ratio per Meter/Second (95% confidence interval) and Statistical Significance | ||||
|---|---|---|---|---|
| Unadjusted for km/day or BMI | Adjusted for Physical Activity (km/day) | Adjusted for BMI Before Exercise | Adjusted for BMI at Baseline | |
| Coronary heart disease death and nonfatal myocardial infarction | 0.56 (0.42–0.77) | 0.57 (0.41–0.80) | 0.59 (0.43–0.82) | 0.68 (0.49–0.94) |
| p value | 0.0003 | 0.001 | 0.002 | 0.02 |
| Nonfatal myocardial infarction | 0.46 (0.32–0.66) | 0.46 (0.32–0.69) | 0.49 (0.33–0.72) | 0.58 (0.39–0.86) |
| p value | <0.0001 | 0.0002 | 0.0003 | 0.008 |
| Angina pectoris | 0.47 (0.30–0.74) | 0.53 (0.33–0.89) | 0.45 (0.28–0.74) | 0.52 (0.32–0.85) |
| p value | 0.001 | 0.02 | 0.002 | 0.01 |
| Percutaneous transluminal coronary angioplasty and coronary artery bypass grafting | 0.68 (0.54–0.86) | 0.74 (0.57–0.96) | 0.69 (0.54–0.88) | 0.83 (0.64–1.06) |
| p value | 0.002 | 0.02 | 0.003 | 0.14 |
Figure 1 shows that risk for nonfatal myocardial infarction decreased linearly with increasing fitness. Those runners able to run faster than 4.75 m/s had an 89% lower risk than the least fit (i.e., slowest) men. There was significantly less risk in those running ≥3.25 compared to <3.25 m/s (p = 0.001), ≥3.75 compared to 3.25 to 3.74 m/s (p = 0.05), and ≥4.25 compared to 3.75 to 4.24 m/s (p = 0.01). Adjustment for physical activity had no effect on risk decrease associated with baseline fitness. Adjustment for the men’s BMI when they began running (i.e., self-selection) also had little effect on the risk decrease, as did adjustment for baseline BMI, although adjustment for the latter did eliminate the significance of all fitness intervals <4.25 m/s but not those intervals ≥4.25 m/s. Including fatal CHD with nonfatal myocardial infarctions yielded similar results except for a loss of significance at the highest fitness category. Angina pectoris risk also decreased linearly with cardiorespiratory fitness, and the risk was essentially nonexistent in the fittest men. Risk for revascularization procedures decreased primarily at >4 m/s in race performance ( Figure 2 ) and was only slightly attenuated by adjustment for physical activity. Those who ran 4.5 to 4.9 m/s were at 58% lower risk for revascularization than those who ran <4.0 m/s, and those who ran ≥5.0 m/s had no detectable risk.