Contrast-induced nephropathy (CIN) after percutaneous coronary interventions (PCI) in patients with acute myocardial infarction (AMI) is associated with high morbidity and mortality, whereas there are no reliable predictive tools easy to use. We evaluated the association of pre-procedural high-sensitivity C-reactive protein (hsCRP) with the development of CIN and integrated this variable in a new risk CIN prediction model. Consecutive patients (348 AMI subjects) who underwent PCI were recruited. Creatinine levels were detected on admission, at 24, 48, and 72 hours after PCI. CIN was defined using the Kidney Disease: Improving Global Outcomes criteria. In our study population (348 subjects), CIN developed in 54 patients (15.5%). Patients with CIN were older and had higher hsCRP at admission, whereas their ejection fraction (EF) and glomerular filtration rate (GFR) were lower. In multivariate analysis after incorporating potential confounders, hsCRP at admission was an independent predictor of CIN (OR for logCRP 2.00, p = 0.01). In receiver-operating characteristic curve analysis, a model incorporating hsCRP, age, GFR, and EF showed good accuracy in predicting the development of CIN (c statistic 0.84, 95% confidence interval 0.793 to 0.879). A total risk score derived from the proposed model yielded significant positive and negative predictive values and classified 85.8% of our patients correctly for CIN. In conclusion, measuring hsCRP levels at admission in patients who underwent PCI for AMI may offer additional assistance in predicting the development of CIN. A model incorporating age and admission hsCRP, EF, and GFR emerged as an accurate tool for predicting CIN in this context.
We examined the association of pre-procedural high-sensitivity C-reactive protein (hsCRP) levels with the development of contrast-induced nephropathy (CIN) in a prospective cohort of patients who underwent coronary intervention for acute myocardial infarction (AMI) and evaluated its ability in predicting CIN. Furthermore, we have assessed the predictive value of a model incorporating hsCRP along with established clinical risk factors and evaluated its diagnostic performance.
Methods
From November 2006 to March 2009, we prospectively collected inhospital data from consecutive patients who underwent emergency percutaneous coronary intervention (PCI) for AMI within 12 hours from symptoms onset as previously described. Diagnosis of ST-segment elevation myocardial infraction (STEMI) or non-STEMI (NSTEMI) was established according to the contemporary guidelines. We excluded patients on chronic peritoneal or hemodialysis treatment and those who had undergone a renal transplantation or were exposed to contrast injection within 7 days before PCI. Patients with active infection or chronic inflammatory disease, any significant systemic disease, severe hepatic dysfunction, known malignancy, or major surgery in the previous month were not included. Patients who presented with cardiogenic shock or died during the first 72 hours of their hospital stay or during revascularization were also excluded from the study. During the study period, 348 patients who fulfilled the earlier mentioned criteria were finally enrolled.
The study was approved by our institution human research committee, and informed consent was obtained from each patient. Moreover, the study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki.
The patients’ baseline characteristics and inhospital and follow-up data were recorded in pre-designed case report forms. In all patients, a detailed medical history was recorded, including presence and management of hypertension, hypercholesterolemia, diabetes mellitus, family medical history of coronary artery disease, and smoking status. Patients whose average blood pressure levels were ≥140/90 mm Hg or were under antihypertensive medication were regarded as having arterial hypertension. Diabetes mellitus was considered to be present if a patient had been informed of this diagnosis and/or was on prescribed treatment for diabetes. Patients that smoked at least 1 cigarette/day were defined as active smokers.
On admission, venous blood samples were obtained before administration of any medication. Serum creatinine concentration was measured in all patients apart from admission at 24, 48, and 72 hours after PCI. hsCRP levels were measured by nephelometry (BNII Siemens System, Marburg, Germany), with the lower detectable values being 0.2 mg/L. Glomerular filtration rate (GFR) was estimated by Chronic Kidney Disease Epidemiology Collaboration equations (ml/min/1.73 m 2 ). CIN was defined using the Kidney Disease: Improving Global Outcomes (KDIGO) criteria for contrast-induced acute kidney injury, according to the most recent recommendations. In brief, CIN was defined as any of the following: increase in serum creatinine by ≥0.3 mg/dl within 48 hours, increase in serum creatinine to ≥1.5 times compared with baseline values, or urine volume <0.5 ml/kg/h for 6 hours.
Left ventricular ejection fraction (LVEF) was assessed on admission with 2-dimensional echocardiography by applying the modified Simpson’s rule, using a Vivid e cardiovascular ultrasound system (General Electric, Milwaukee, Wisconsin) equipped with a 2.0 to 3.6 MHz (harmonics) phased array transducer.
Significant coronary artery disease was diagnosed in the presence of ≥50% luminal diameter narrowing in at least 1 major coronary artery. Coronary angiographies were interpreted by at least 2 experienced interventional cardiologists.
Categorical variables were summarized using frequencies and percentages and were compared using Fisher’s exact test. Continuous variables were summarized either as mean ± SD or as median (interquartile range), depending on data normality. Comparisons were performed with unpaired Student’s t test or Mann-Whitney U test as appropriate. A multivariable logistic regression model was used to evaluate the independent contribution of hsCRP and other established risk factors (age, history of diabetes, admission systolic blood pressure, GFR, hemoglobin, and LVEF) to the development of CIN. Receiver-operating characteristic (ROC) curve analysis was used to examine the accuracy of the model to predict development of CIN.
To create and validate a clinical prediction rule for identifying subjects at risk for acute kidney injury after PCI procedures, a set of most relevant predictors was selected on the basis of the best predictive multivariable logistic model. Backward elimination variable selection was used, and variables were dropped because of nonsignificance (p >0.1) or collinearity. Model selection was based on nonmissing data. Four predictors were selected (age, GFR, LVEF, and hsCRP), and subsequently, continuous variables were recoded into ordinal ones. The cut-off values for categories were derived from previous literature and the sampling distribution (median and percentiles) of the aforementioned variables. Especially for estimated glomerular filtration rate (eGFR) and hsCRP, a combined technique of graphical modeling of the association of the continuous variable with the outcome and iterating minimization of likelihood ratio tests of all possible cut-points in alternative logistic models regressed on CIN was implemented for optimal cut-off determination. Bonferroni and Benjamini-Hochberg corrections were used to adjust derived p values in the loop techniques for cut-point selection. To derive a simple-to-calculate risk score, the regression coefficients for the ordinal variables were divided by the smallest coefficient and then rounded to the nearest integer. The individual risk score of the 4 predictors was summed and a total risk score assigned to each patient of our sample for presenting CIN.
External validation of our score was not performed because data were available only from our hospital. Therefore, we proceeded to internal validation by the bootstrap method that validated the weights assigned to the 4 variables of our risk score from the final logistic regression model. The correctly classified percentage of subjects and the positive and the negative predictive values were selected as indexes of the performance rule and were calculated from bootstrap iterations and subsequent application to the resample.
Differences were considered statistically significant at the 2-sided p <0.05 level. Comparison of ROC curves was performed with MedCalc Statistical Software, version 14.8.1 (MedCalcSoftware bvba, Ostend, Belgium). All other statistical analyses were performed using STATA statistical software, version 11.0 (StataCorp, College Station, Texas).
Results
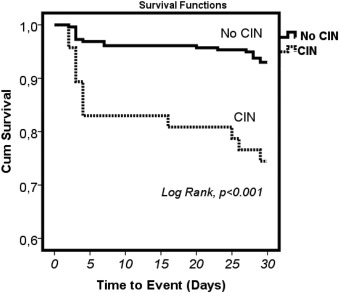
Baseline clinical characteristics of the study population are presented in Table 1 . Of the 348 included patients, 54 (15.5%) developed CIN. The incidence of all-cause mortality within 30 days from hospital admission was higher in patients with CIN (25.5% vs 7%, p = 0.001), and in Kaplan-Meier analysis, CIN development was associated with 30-day mortality ( Figure 1 ).
| Variables | Contrast-Induced Nephropathy | P value | |
|---|---|---|---|
| Yes (n = 54) | No (n = 294) | ||
| Men | 45 (83.3%) | 259 (88.1%) | 0.37 |
| Age (years) | 69.1 ± 12.1 | 59.3 ± 11.7 | <0.001 |
| Systolic Blood Pressure (mm Hg) | 130±29 | 136±27 | 0.13 |
| Diastolic Blood Pressure (mm Hg) | 76±10 | 78±13 | 0.32 |
| Smokers | 50% | 62% | 0.09 |
| Hypertension | 74% | 53% | 0.005 |
| Diabetes | 33% | 24% | 0.14 |
| Dyslipidemia | 56% | 61% | 0.49 |
| White Blood Cell Count/μL | 11821±4366 | 11403±3461 | 0.51 |
| Hemoglobin (g/dL) | 12.9±2.0 | 14.1±1.7 | 0.001 |
| Serum creatinine (mg/dL) | 1.2(0.9-1.7) | 1.0(0.9-1.2) | 0.005 |
| Estimated glomerular filtration rate (ml/min/1.73 m 2 ) | 71±38 | 98±26 | <0.001 |
| High sensitivity C-reactive protein (mg/L) | 30.6(9.2-77.0) | 10.2(3.3-29.9) | 0.007 |
| Troponin I (ng/mL) | 1.31(0.28-11.6) | 0.42(0.05-3.97) | 0.09 |
| Left ventricular ejection fraction (%) | 39±10 | 45±10 | <0.001 |
| ST-segment elevation myocardial infarction | 61% | 67% | 0.42 |
| Primary or emergency percutaneous coronary intervention | 91% | 91% | 0.99 |
| Number of narrowed coronary arteries | 2.2±0.9 | 2.1±0.9 | 0.34 |
| Contrast medium volume (mL) | 173±42 | 161±34 | 0.05 |
As it is listed in Table 1 , patients who developed CIN were older and had higher hsCRP levels. Admission creatinine levels were higher in patients who developed CIN. In contrast, eGFR, hemoglobin levels and LVEF were all lower in patients with CIN.
A multivariable logistic regression model incorporating age, history of diabetes, admission systolic blood pressure, eGFR, hemoglobin, and LVEF was used to evaluate the independent contribution of each factor in the development of CIN. This model revealed that independently of other confounders, admission LVEF and eGFR were inversely associated with the development of CIN, whereas age and hsCRP levels were positively associated with CIN development ( Table 2 ).
| Variable | Odds ratio | 95% Confidence Interval | P value | |
|---|---|---|---|---|
| Lower | Upper | |||
| Age (Years) | 1.06 | 1.03 | 1.10 | <0.001 |
| Estimated Glomerular filtration rate (ml/min/1.73 m 2 ) | 0.96 | 0.92 | 0.99 | 0.001 |
| Log(high sensitivity C-reactive protein) (mg/L) | 2.00 | 1.17 | 3.43 | 0.01 |
| Left ventricle ejection fraction (%) | 0.96 | 0.93 | 0.99 | 0.02 |
Using ROC curve analysis, the resulting model incorporating hsCRP, age, eGFR, and LVEF showed good accuracy in predicting the development of CIN (c statistic: 0.84, 95% confidence interval [CI] 0.79 to 0.88) according to KDIGO criteria. Compared with a model incorporating only age, eGFR, and LVEF (c statistic: 0.79, 95% CI 0.76 to 0.83), the model with the addition of hsCRP demonstrated a significantly improved accuracy (p = 0.007).
Table 3 summarizes the derivation of the risk score (Athens CIN score) for CIN development from the 4 aforementioned predictors (i.e., eGFR, LVEF, hsCRP, and age). hsCRP was used as the reference regression coefficient and was assigned a weighted value of 1 per category above the baseline. Age was assigned a weight of 2 per category above the baseline, whereas the rest of the predictors received a weighted risk score of 1 per category below the reference. The range of the risk score was 0 to 11. Figure 2 depicts both observed and expected probabilities for CIN across the 12 categories of the total risk score.
| Predictor | Multivariable Odds Ratio | Weight for Risk Score ∗ | Assigned Points per Predictor | |
|---|---|---|---|---|
| Regression Coefficient | 95% CIs | |||
| Age (years) | 2.71 | 1.52-4.83 | 2 | |
| <50 † | 0 | |||
| 50-75 | 2 | |||
| >75 | 4 | |||
| Estimated Glomerular filtration rate (ml/min/1.73 m 2 ) | 2.1 | 1.22-3.53 | 1 | |
| <60 | 2 | |||
| 59.9-89.9 | 1 | |||
| >90 † | 0 | |||
| Left ventricle ejection fraction (%) | 1.87 | 1.2-2.91 | 1 | |
| <35 | 2 | |||
| 35-50 | 1 | |||
| >50 † | 0 | |||
| High sensitivity C-reactive protein (pg/dl) | 1.56 | 1.16-2.1 | 1 | |
| <3.6 † | 0 | |||
| 3.61-11.5 | 1 | |||
| 11.51-33 | 2 | |||
| >33 | 3 | |||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


