Animal and imaging study evidence favors early reperfusion for acute myocardial infarction. However, in clinical trials, the effect of symptom-onset-to-balloon (S2B) time on clinical outcomes in patients with ST-segment elevation myocardial infarction (STEMI) undergoing primary percutaneous coronary intervention (pPCI) has been inconsistent. Moreover, there are few data regarding the ischemic time in China. A total of 3,877 consecutive patients with STEMI with available S2B time undergoing pPCI from January 2013 to September 2014 at 108 hospitals that participated in the China Acute Myocardial Infarction registry were included and stratified into 3 S2B groups: <6 hours, 6 to 12 hours, >12 hours S2B time was tested in multivariate logistic regression analyses as an independent risk factor of mortality (primary outcome), major adverse cardiovascular and cerebrovascular events (MACCE), and impaired myocardial perfusion (secondary outcomes). The median S2B time was 5.5 (3.75 to 8.50) hours. Longer S2B time was associated with higher in-hospital mortality (<6 hours: 2.7%; 6 to 12 hours: 3.4%; >12 hours: 4.9%; p = 0.047) and ST-segment resolution <50% (<6 hours: 16.7%; 6 to 12 hours: 19.2%; >12 hours: 24.3%; p = 0.002) but not MACCE. In multivariate-adjusted analysis, S2B >12 hours remained associated with ST-segment resolution <50% (odds ratio 1.53, 95% confidence interval 1.16 to 2.01, p = 0.002) but not with in-hospital mortality (odds ratio 1.673, 95% confidence interval 0.95 to 2.94, p = 0.073). In conclusion, median S2B time in patients with STEMI undergoing pPCI was longer than that in registry studies from other countries. Longer S2B time was associated with impaired myocardial perfusion but not with in-hospital mortality or MACCE.
Myocardial infarction, with its high mortality, remains a serious public health threat. Evidence from animal and magnetic resonance imaging studies has underscored the importance of total time delay in acute myocardial infarction (AMI). However, evidence from clinical trials is insufficient, as reflected in current guidelines for the treatment of ST-segment elevation myocardial infarction (STEMI), which mainly focus on time subintervals such as the first medical contact-to-device (FMC-to-device) time or door-to-balloon (D2B) time rather than symptom onset-to-balloon (S2B) time. Moreover, clinical studies have yielded inconsistent results on the effect of S2B time on mortality: some have failed to find an association and thereby have inferred that S2B time may be less important to primary percutaneous coronary intervention (pPCI) compared with fibrinolysis because pPCI can achieve high proportions of Thrombolysis In Myocardial Infarction (TIMI) 3 flow even in late comers. In positive studies, findings on the relation between S2B time and mortality were variable: a linear relation in 2 studies or 1 with 2 peaks in another ; in some studies, mortality increased sharply after a certain time point, whereas in another, S2B time appeared to only have an effect on mortality during the first few hours. To date, there are little data on S2B time in China; the present study aimed to investigate the Chinese real-world treatment delay and its effect on in-hospital outcomes in patients with STEMI undergoing pPCI by analyzing a consecutive national sample derived from the Chinese acute myocardial infarction (CAMI) registry.
Methods
The CAMI registry is a prospective, nationwide, multicenter observational study of patients with AMI. The registry includes 3 levels of hospitals (provincial-, prefectural- and county-level hospitals) covering all the provinces and municipalities across mainland China, which render it likely representative of routine real-world clinical practice of AMI care in China. Provincial-, prefectural- and county-level hospitals are founded following Chinese vertical governmental model and are similar to the hierarchy of tertiary, secondary, and primary care hospitals but are not exactly the same; they represent not only the heath care level but also geographic region hierarchy. Each institution was instructed to enroll consecutive patients with AMI, within 7 days of acute ischemic symptoms. Final inclusion criteria met the third University Definition for Myocardial Infarction (2012). This study was registered with ClinicalTrials.gov ( NCT01874691 ) and was approved by the institutional review board of all participating hospitals. All patient data were protected at all time. Detailed descriptions about data management and quality control can be found in the methodological article about CAMI registry published previously.
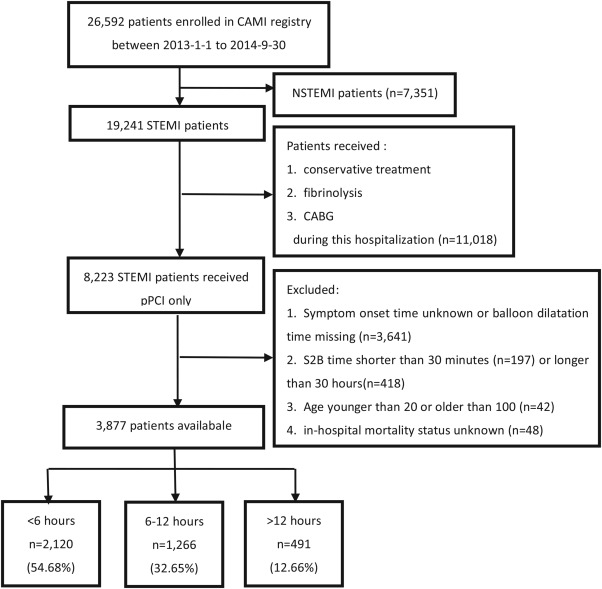
Overall, 26,592 patients from 108 hospitals were enrolled in the CAMI registry from January 1, 2013, to September 30, 2014. All 8,223 patients with STEMI undergoing pPCI were included in the present study. The following patients were excluded sequentially: patients with unknown symptom onset time or missing balloon dilatation time (n = 3641); patients with S2B time <30 minutes (n = 197) or >30 hours (n = 418); patients aged <20 or >100 years (n = 42); and patients with unknown in-hospital mortality status (n = 48). The final cohort of 3,877 patients was stratified into 3 groups based on the clinical significance of S2B time and the median S2B time in China: ≤6, 6 to 12, and ≥12 hours ( Figure 1 ). S2B time was defined as the time from symptom onset to the first balloon inflation during percutaneous coronary intervention, and the starting time of symptom was collected by asking the patient or relatives about the time for initiation of continuous chest pain. The primary outcome was in-hospital mortality, which was defined as death during hospitalization. The secondary outcomes were ST-segment resolution <50% and major adverse cardiovascular and cerebrovascular events (MACCE), a composite of death, reinfarction, and stroke.
Continuous variables are expressed as mean ± standard deviation or median (twenty-fifth and seventy-fifth percentiles), and categorical variables are presented as percentages. Differences in baseline characteristics and in-hospital outcomes in 3 S2B time groups were assessed using the chi-square test or Fisher’s exact test for categorical variables and analysis of variance test or the Wilcoxon rank test for continuous variables. The p value for linear trend was estimated using Cochran–Armitage trend test between S2B time groups and in-hospital mortality. Multivariate logistic regression analyses were conducted to evaluate the adjusted effect of S2B time on in-hospital mortality, MACCE, and ST-segment resolution. Clinically and statistically significant covariates were all entered into the model, and results were reported as adjusted odds ratios together with corresponding 95% confidence intervals (CI). For all analyses, a 2-sided p value <0.05 was considered significant. Because of the large sample size, comprehensive consideration of absolute disparity and p value is necessary. Statistical analysis was performed using SAS 9.4.
Results
In the overall CAMI study cohort, patients had a mean age of 60.28 ± 11.99 years and were mostly men (78.6%). Among the 19,241 patients with STEMI, 8,233 (42.8%) received pPCI. The median S2B time was 5.5 hours (3.75 to 8.50 hours). Rate of successful pPCI, defined as achievement of TIMI 3 flow, was 94.2%. Demographic, clinical, and angiographic characteristics according to S2B time groups are presented in Table 1 . Patients with longer S2B time delay were more likely to be women, with diabetes or multivessel disease, whereas early arrivers had worse pre-PCI TIMI flow, with a greater proportion of myocardial infarction history or previous PCI. In addition, the total time delay differed according to hospital level: province-level hospitals had longer S2B time delay than prefecture- and county-level hospitals ( Figure 2 ).
| Variables | Symptom to Onset (Hours) | P value | ||
|---|---|---|---|---|
| <6 (2120) | 6-12 (1266) | ≥12 (491) | ||
| Age(mean±SD) [years] | 59.60 ±12.00 | 61.20 ±11.84 | 60.84 ±12.21 | 0.0004 |
| Women | 400 (18.9%) | 296 (23.4%) | 131 (26.7%) | 0.0001 |
| Body mass index [Kg/m 2 ] | 24.56 ±3.06 | 24.45 ±8.91 | 24.52 ±3.53 | 0.8759 |
| Hypertension | 1010 (47.8%) | 597 (47.2%) | 244 (50.1%) | 0.2418 |
| Dyslipidemia | 219 (10.4%) | 122 (9.7%) | 66 (13.6%) | 0.0088 |
| Smoker | 1305 (61.5%) | 741 (58.4%) | 281 (56.5%) | 0.4195 |
| Diabetes mellitus | 376 (17.8%) | 210 (16.6%) | 112 (23.0%) | 0.0002 |
| Angina pectoris | 413 (21.1%) | 245 (21.8%) | 102 (23.7%) | 0.4782 |
| Previous myocardial infarction | 119 (5.6%) | 56 (4.4%) | 21 (4.3%) | 0.0000 |
| Prior percutaneous coronary intervention | 72 (3.4%) | 32 (2.5%) | 14 (2.9%) | 0.0000 |
| Anterior wall involved | 1029 (48.7%) | 634 (50.3%) | 249 (50.7%) | 0.5840 |
| Cardiac shock | 86 (4.1%) | 34 (2.7%) | 18 (3.7%) | 0.2438 |
| Cardiac arrest | 34 (1.6%) | 17 (1.4%) | 7 (1.4%) | 0.8245 |
| Killip class | 0.3950 | |||
| Ⅰ/Ⅱ | 1996 (94.7%) | 1207 (95.7%) | 463 (94.9%) | |
| Ⅲ/Ⅵ | 112 (5.3%) | 54 (4.3%) | 25 (5.1%) | |
| Heart rate at admission [beats/minute] | 74.97 ±17.09 | 75.99 ±17.34 | 75.67 ±18.05 | 0.2365 |
| Systolic blood pressure at admission [mmHg] | 127.35 ±25.30 | 127.65±25.38 | 127.74 ±26.20 | 0.9252 |
| Baseline creatinine concentration>133mg/mL | 86 (4.1%) | 47 (3.8%) | 25 (5.2%) | 0.4508 |
| Hospital level | 0.0000 | |||
| Province | 641 ( 30.2%) | 565 ( 44.6%) | 199 ( 40.5%) | |
| Prefecture | 1280 ( 60.4%) | 641 ( 50.6%) | 271 ( 55.2%) | |
| County | 199 (9.4%) | 60 (4.7%) | 21 ( 4.3%) | |
| Left main disease | 47 (2.3%) | 15 (1.2%) | 13 (2.7%) | 0.0401 |
| Multi-vessel disease ∗ | 1319 (64.0%) | 805 (65.1%) | 336 (70.1%) | 0.0358 |
| Number of stents implanted | 0.0515 | |||
| 0-1 | 1595 (82.6%) | 927 (80.6%) | 351 (80.4%) | |
| ≥2 | 336 (17.4%) | 223 (19.3%) | 86 (19.6%) | |
| Pre-PCI TIMI flow | <.0001 | |||
| 0-Ⅰ | 1770 (83.9%) | 1053 (83.6%) | 38 (78.8%) | |
| Ⅱ-Ⅲ | 340 (16.1%) | 207 (16.4%) | 104 (21.1%) | |
| Post-PCI TIMI flow Ⅲ | 2009 (95.4%) | 1190 (94.7%) | 454 (93.6%) | 0.2416 |
∗ Multi-vessel disease: more than one coronary artery lesion.
Clinical outcomes are presented in Table 2 . One hundred twenty-five patients (3.22%) died in hospital. There was a significant stepwise progressive increase in mortality with increasing S2B time, and the relation between S2B time and mortality was linear as shown by linear-by-linear association. However, no significant differences or particular trends with S2B time were observed for MACCE. As an indicator of impaired myocardial perfusion, the percent of ST segment resolution <50% increased as time delayed.
| Variables | Symptom-onset-to-balloon Time (hours) | P value | ||
|---|---|---|---|---|
| <6 (2120) | 6-12 (1266) | >12 (491) | ||
| Death | 58 (2.7%) | 43 (3.4%) | 24 (4.9%) | 0.0470 |
| Linear-by-linear association | 0.017 | |||
| MACCE ∗ | 113 (5.3%) | 75 (5.9%) | 29 (5.9%) | 0.7300 |
| Stroke | 11 (0.5%) | 8 (0.6%) | 3 (0.6%) | 0.9065 |
| Re-infarction | 7 (0.3%) | 8 (0.6%) | 2 (0.4%) | 0.4516 |
| Heart failure(new onset or worsen) | 242 (11.4%) | 142 (11.2%) | 56 (11.4%) | 0.9852 |
| ST-segment resolution <50% | 294 (16.7%) | 208 (19.2%) | 208 (24.3%) | 0.0022 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


