Cardiac resynchronization therapy (CRT) is often deferred in dialysis-dependent patients with heart failure (HF) because of a perceived lack of benefit and potentially higher risks, although the outcomes associated with CRT in dialysis have not been reported. We therefore studied our center’s experience with CRT in dialysis-dependent patients. We constructed a descriptive assessment of these patients (n = 15) and performed a case-control analysis matching for age, gender, bundle branch morphology, diabetes mellitus, cardiomyopathy origin, and β-blocker and angiotensin-converting enzyme inhibitor or angiotensin II receptor blocker use. Baseline and 6-month echocardiograms were assessed for evidence of reverse remodeling. No periprocedural or long-term complications were observed among dialysis patients. Heterogenous improvement in ejection fraction (+3.1 ± 9.2%) was noted and 2 patients derived absolute improvements of 8% and 22%, respectively. Dialysis patients demonstrated the following 3-year event rates: HF hospitalization, 31%; all-cause hospitalization, 100%; mortality, 73%; and HF hospitalization or death, 82%. In the case-control analysis, controls demonstrated superior reverse remodeling (+9.2 ± 9.5% increase in ejection fraction), decreased mortality (73% vs 44%, p = 0.038), and all-cause hospitalizations (76% vs 100%, p = 0.047), with no difference in HF hospitalizations (p = 0.39), compared with dialysis patients. In conclusion, at our center, the dialysis-dependent patients with HF who underwent CRT implantation did so safely and no serious complications were observed. Certain dialysis patients demonstrated compelling improvement after device implantation. Compared with matched controls, dialysis patients were at increased risk for adverse events and worsened echocardiographic outcomes.
Medication refractory heart failure (HF) and end stage renal disease (ESRD) represent 2 of the more challenging and resource-intensive chronic conditions for today’s physicians and health-care systems. Both conditions are linked by multiple risk factors including ischemic heart disease, obesity, hypertension, diabetes mellitus, tobacco abuse, and increasing age. Furthermore, the presence of HF increases the risk of chronic renal insufficiency and vice versa. Importantly, approximately 50% of patients with ESRD will develop HF. Although cardiac resynchronization therapy (CRT) has represented an important advance in the care of patients with HF, its use in patients with ESRD has been associated with considerable controversy. The major randomized control trials of CRT have either formally excluded patients with ESRD or not reported enrollment of these patients, and to our knowledge, there are no published nonrandomized studies in the published works assessing this important population. Thus, it is not clear whether this highly co-morbid population derives benefit from CRT and whether there are an excess of device related complications. As such, it is an area in need of study from a clinical practice and comparative effectiveness research standpoint. In this study, we systematically reported outcomes associated with CRT in dialysis-dependent patients with HF implanted at our institution. We subsequently compared outcomes with matched controls.
Methods
We identified a cohort of patients with ESRD on dialysis who were implanted with CRT for traditional indications: left ventricular (LV) ejection fraction (EF) <35%, New York Heart Association (NYHA) III or IV symptom class, and QRS duration of >120 ms. Patients with newer CRT indications (NYHA class I or II) were not well represented in this patient cohort, although they were not specifically excluded. QPID software (QPID Health, Boston, Massachusetts) was used as an electronic medical record search platform to perform an automated natural language query of the electronic medical record of all patients who underwent a CRT procedure from May 24, 2002 to February 9, 2012 at the Massachusetts General Hospital (as determined by billing data) to identify patients who were on permanent dialysis at the time of device implantation. Those with CRT implanted at other institutions were excluded from this analysis. Automated query followed by manual review of tagged patients identified a total of 15 patients.
For our secondary case-control analyses, controls were selected from a previously established patient database of patients at our institution and were matched based on age (within 5 years), gender, bundle branch morphology, cardiomyopathy origin, diabetes mellitus, and baseline use of β blockers, angiotensin-converting enzyme inhibitor or angiotensin II receptor blocker, and spironolactone. Two controls were selected for each case. In situations when there were >2 complete matches, those with the closest age match were selected. When a complete match was not available, we prioritized matching medical co-morbidities, age, bundle branch morphology, and gender, over medication use. Patients who began dialysis after CRT implantation were eligible to be a control.
Standard echocardiographic, clinical, and demographic data were collected. LV diameter measurements were made using the parasternal long-axis view and EFs measurement was obtained using the modified Quinones method or biplane method of discs at the discretion of the echocardiographer. Follow-up echocardiograms were obtained 6 months after device implantation.
The co-primary end points of the study were all-cause mortality and echocardiographic response. Survival status was assessed by way of chart review and query of the national death index. Echocardiographic response was defined as ≥5% absolute increase in EF. Secondary end points included time until HF hospitalization, time until all-cause hospitalization, and the combined end point of HF hospitalization or death. Mortality was assessed by way of chart review and query of the national death index. Other clinical events were assessed by way of chart review.
Statistical analyses were performed using SPSS, version 20.0 (IBM, Chicago, Illinois) and SAS Enterprise Guide 4.3 (SAS Institute Inc., Cary, North Carolina). Baseline characteristics of patients are presented as mean ± SD for continuous variables and as proportions for categorical variables. Differences among proportions were assessed using Pearson chi-square or Fisher’s exact test where appropriate, and differences in mean values were compared with Student t tests. Kaplan-Meier curves were constructed to compare event rates among different groups and differences were formally assessed using the log-rank test. Cox proportional hazard modeling was used to assess relative hazards. A p value of <0.05 was required for statistical significance.
Results
We identified 15 dialysis-dependent patients with HF who were implanted with CRT devices at our institution. Study subjects demonstrated a reduced EF of 21 ± 7%, prolonged QRS of 171 ± 29 ms, and advanced NYHA symptom class (mean, 3.2 ± 0.7); 20% of the subjects were women. Baseline QRS morphology was predominantly left bundle branch block (53%); 27% had an underlying paced rhythm and 20% had an intraventricular conduction delay. Most patients had chronic atrial fibrillation (60%), ischemic cardiomyopathy (67%), diabetes (53%), history of coronary artery bypass grafting (67%), and CRT with defibrillator (87%). All patients underwent successful transvenous lead implantation, although 1 patient ultimately had an epicardial lead placed because of incessant diaphragmatic pacing. Individual patient level information is listed in Table 1 . Dialysis patients did not experience any procedural complications including pocket hematoma (requiring treatment), lead dislodgement, pneumothorax, or cardiac perforation.
| Age (yrs) | Gender | Dialysis | ICD | BBB | QRS (ms) | EF (%) | NYHA Class | Generator vs Fistula Side | CS Lead | ICM | DM | HTN | Revascularization | AF | Valve Surgery | Medications | Echo Responder (Absolute Change in EF) | Device Complications | CRT to Death in Days | Renal Transplant (CRT to Transplant in Days) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 52 | M | HD | + | IVCD | 180 | 20 | III | R/L | + | + | + | + | CABG | CAF | 0 | Dig | 0 (−5%) | 0 | 1,215 (Alive) | 0 |
| 62 | M | HD | + | Paced | 212 | — | — | L/R | + | + | + | + | CABG | CAF | + | AA/BB/Dig | — | 0 | 469 | 0 |
| 63 | M | HD | + | IVCD | 118 | 15 | IV | R/L | + | 0 | 0 | + | 0 | CAF | 0 | BB/ACE | D | 0 ∗ | 78 | 0 |
| 66 | F | HD | + | IVCD | 124 | 23 | III | R/L | + | + | + | + | PCI | 0 | 0 | BB | — | 0 | 967 (Alive) | 0 |
| 69 | M | PD | + | Paced | 213 | 30 | IV | R/PD | + | 0 | + | + | CABG | CAF | + | BB | + (+8%) | 0 | 464 | 0 |
| 70 | M | HD | + | LBBB | 142 | 15 | IV | R/L | + | + | 0 | + | CABG/PCI | CAF | 0 | BB/ACE | D | 0 | 102 | 0 |
| 71 | F | HD | + | LBBB | 176 | 16 | — | R/L | + | 0 | + | + | 0 | 0 | + | Dig | 0 (−3%) | 0 | 588 † | 0 |
| 71 | M | HD | + | LBBB | 160 | 29 | II | L/R | + | + | + | + | CABG | 0 | + | BB | 0 (0%) | 0 | 550 (Alive) | + (550) |
| 72 | M | HD | 0 | LBBB | 188 | 18 | III | R/L | + | 0 | 0 | + | 0 | PAF | 0 | Dig/BB | + (+22%) | 0 | 3,016 (Alive) | + (642) |
| 72 | M | HD | + | LBBB | 179 | 17 | — | R/L | + | + | + | + | CABG | 0 | 0 | AA/BB/ACE | — | 0 ‡ | 1,053 | 0 |
| 75 | F | HD | + | LBBB | 152 | 25 | III | R/L | 0 | + | 0 | + | CABG | CAF | 0 | BB/ACE | — | +, DS | 2,641 (Alive) | 0 |
| 75 | M | HD | + | LBBB | 178 | 23 | — | L/tunneled | + | + | 0 | + | CABG | CAF | 0 | AA/Dig/BB/ARB | 0 (0%) | 0 | 181 | 0 |
| 75 | M | HD | + | LBBB | 162 | 13 | — | R/L | + | + | 0 | + | CABG | PAF | 0 | BB | D | 0 | 17 | 0 |
| 81 | M | HD | + | Paced | 166 | 35 | III | R/L | + | + | + | 0 | CABG | CAF | 0 | Dig/BB/ARB | D | 0 | 175 | 0 |
| 94 | M | HD | 0 | Paced | 213 | 21 | — | L/tunneled | + | 0 | 0 | 0 | 0 | 0 | 0 | BB/ACE | 0 (0%) | 0 | 998 | 0 |
∗ Patient had a preimplant history of recurrent arteriovenous graft thrombosis due to a stenosed venous anastamosis. He underwent placement of a defibrillation coil in the left subclavian vein after defibrillation threshold testing failed to convert to sinus rhythm despite high-output shocks. This patient had an arteriovenous fistula thrombosis the day after CRT placement, the second thrombosis in 2 weeks.
† Died from presumed S aureus endocarditis that did not appear to be a procedural complication.
‡ A complete occlusion of right subclavian was noted on venography 15 months after implant; it did not impact existing fistula access at the time, but did preclude physicians from creating a new right-sided fistula after recurrent bleeding from the established left-sided fistula.
By 6 months, 1/3 of dialysis patients died. One patient underwent follow-up echocardiography shortly before dying 181 days after CRT implantation. Of the remaining patients, 70% had baseline and follow-up echocardiograms. Those with baseline and follow-up echocardiograms demonstrated a modest mean improvement in EF (+3 ± 9%), although substantial heterogeneity existed. Notably, 2 patients demonstrated robust improvement in EF after device implantation, with absolute improvements of 8% and 22%, respectively. Both of these patients had nonischemic cardiomyopathy and preimplantation QRS morphologies that have been associated with enhanced echocardiographic response: left bundle branch block in one patient and paced rhythm in the other.
At 3 years, Kaplan-Meier modeling predicted a 31% incidence of HF hospitalization, 100% incidence of hospitalization for any cause, 73% mortality, and 82% incidence of HF hospitalization or death. The rate of all-cause hospitalizations was not related to procedural complications. During follow-up, we observed no CRT device related complications (including device or lead infections) except for diaphragmatic stimulation and no patients required device explant. No patients experienced dialysis access site thrombosis associated with a CRT device. Two patients ultimately underwent orthotopic kidney transplantation. One dialysis patient was treated for presumed Staphylococcus aureus endocarditis 13 months after implant; the diagnosis was based on bacteremia with splenic infarcts, although no vegetations were observed on transthoracic or transesophageal echocardiogram. The patient was readmitted 6 months later with S aureus (different strain) bacteremia and presumed endocarditis based on the presence of splenic infarcts; no vegetations were observed on echocardiogram. The patient died from overwhelming sepsis a day after admission. The initial infection occurred over a year after CRT implantation and did not appear to be related to a procedural complication.
We performed a case-control analysis to compare outcomes among dialysis patients and otherwise similar patients who routinely undergo CRT. The cases (n = 15) and controls (n = 30) were well matched and there were no differences in baseline clinical covariates except that controls were more likely to use diuretics and have paroxysmal atrial fibrillation. The mean creatinine of controls was 1.7 mg/dl. At 3 years, Kaplan-Meier modeling of the entire study population (n = 45) predicted a 42% incidence of HF hospitalization, 82% incidence of all-cause hospitalization, 63% incidence of HF hospitalization or death, and a 53% incidence of death.
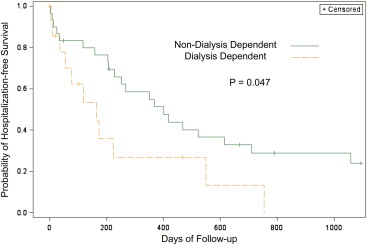
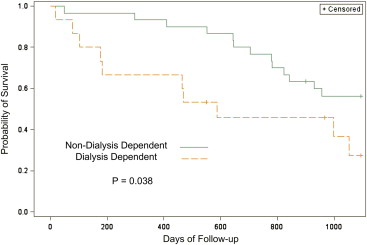
Incidence of HF hospitalization, all-cause hospitalization, death, and a composite outcome of HF hospitalization or death was compared among dialysis-dependent patients and matched controls. Compared with controls, dialysis-dependent patients experienced an increased incidence of all-cause hospitalization (100% vs 76%, p = 0.047; Figure 1 ) and death (73% vs 44%, p = 0.038; Figure 2 ), but not HF hospitalization (31% vs 45%, p = 0.39); there was a trend toward increased rate of HF hospitalization or death (82% vs 54%, p = 0.08). Proportional hazards modeling demonstrated dialysis dependence was associated with a 2× risk (hazard ratio 2.11, confidence interval 1.00 to 4.47, p = 0.05) of all-cause hospitalization and 2.5× increased risk of death (hazard ratio 2.35, confidence interval 1.03 to 5.39, p = 0.044). Of note, discharge summary review revealed that only 1 HF hospitalization in the control group was associated with poorly controlled atrial fibrillation. Paroxysmal atrial fibrillation was not associated with HF hospitalization in a Cox proportional hazards model (p = 0.45). Thus, the difference in paroxysmal atrial fibrillation burden does not appear to mediate the HF hospitalization findings in this study. When paroxysmal atrial fibrillation was considered in a multivariate Cox proportional hazards model, dialysis remained associated with an increased risk of all-cause hospitalization and all-cause mortality.