Chapter 140
Upper Extremity Aneurysms
M. Shadman Baig, Carlos H. Timaran
Based on a chapter in the seventh edition by Carlos H. Timaran
Upper extremity aneurysms are uncommon relative to other peripheral arterial aneurysms.1 Arch vessel aneurysms, the most frequent type of upper extremity aneurysm, can lead to life-threatening exsanguination as a result of rupture, as well as numerous other complications, including stroke, local nerve compression (leading to hoarseness or brachial plexus palsy), and dysphagia from esophageal compression in cases of an aberrant right subclavian artery aneurysm (ARSA), localized pain, or limb ischemia. More distally located upper extremity aneurysms are manifested almost exclusively by thromboembolic complications of the hand and digits.
The earliest reported attempts at surgical correction of arch vessel aneurysms were common carotid aneurysm ligations by Astley Cooper in 1805 and 1808,2 followed by ligation of the innominate artery by Valentine Mott in 1818 for the treatment of a subclavian artery aneurysm.2,3 Mott’s patient expired within 1 month as a result of hemorrhage from the necrotic aneurysm. The first successful treatment of a subclavian artery aneurysm was achieved in 1864 by Smyth in New Orleans, who ligated the right common carotid and innominate artery.4 The aneurysm recurred and ruptured 10 years later. Halsted was the first to combine ligation successfully with resection of a subclavian artery aneurysm in 1892 at the Johns Hopkins Hospital.5 In 1913, Matas reported 225 cases of aneurysms treated by endoaneurysmorrhaphy, and 7 of these were subclavian aneurysms.6
Arch Vessel Aneurysms
Epidemiology and Etiology
Innominate, common carotid, and subclavian artery aneurysms usually arise from degenerative disease. In a series of 74 patients with arch vessel aneurysms, Cury et al reported that 63% were degenerative in nature with the vast majority in men older than 60 years of age.7 Less commonly, these aneurysms can also result from trauma, fibromuscular dysplasia, syphilis, cystic medial necrosis, vasculitis, invasion of the vessel wall by contiguous tuberculous lymphadenitis, and idiopathic congenital causes. Although only 1% of all peripheral arterial aneurysms involve the subclavian and innominate arteries, 30% to 50% of patients with nonspecific, degenerative arch vessel aneurysms have aortoiliac or other peripheral aneurysms.8,9 Patients presenting with these aneurysms should, therefore, be evaluated thoroughly for concurrent aneurysms.
Aneurysms of the distal subclavian artery, frequently with extension into the first portion of the axillary artery, are usually associated with a thoracic outlet obstruction, cervical rib, and other bony abnormalities that result in arterial compression and poststenotic dilatation. This specific type of aneurysm is discussed in Chapter 127.
Subclavian Artery Aneurysms
True subclavian aneurysms, typically seen in older adult patients, are usually degenerative and are the most common type of arch vessel aneurysm, accounting for 50% of the cases in the two largest series reported.7,10 Pairolero et al8 reported the treatment of 31 patients with subclavian artery aneurysms treated over a 20-year period. True degenerative aneurysms were repaired in 12 patients, traumatic pseudoaneurysm in 10, and aneurysms secondary to thoracic outlet obstruction in 6. McCollum et al9 also reported their 25-year experience with subclavian artery aneurysm repairs, which included 15 patients, over half of whom had true degenerative aneurysms. Pseudoaneurysms frequently occur as a result of blunt and penetrating trauma. Iatrogenic injury from inadvertent cannulation of the subclavian artery with pseudoaneurysm formation is uncommon but increasing in frequency due to subclavian vein catheterization for various indications.11,12 Though many small caliber (<7Fr) misplaced catheters can be removed and simple compression applied, removal of larger catheters such as those used for hemodialysis can lead to significant hemorrhage or pseudoaneurysm formation because of an inability to compress the puncture site beneath the clavicle. Recent reports have described the successful use of endovascular techniques to repair arterial injuries occurring during central venous access using endografts or percutaneous closure devices.11,13–16
Innominate Artery Aneurysms
True aneurysms of the innominate artery are rare, representing 2% to 5% of cases of arch vessel aneurysms. Bower et al10 reported their 40-year experience, which included only 4 patients with true aneurysms of the innominate artery among 73 patients treated surgically for brachiocephalic aneurysms. Similarly, in the series reported by Cury et al,7 2 out of 74 surgically treated supra-aortic aneurysms were of the innominate artery. The largest series of innominate aneurysm repair is by Kieffer et al,17 in which they found 6 degenerative aneurysms among 27 patients with innominate artery aneurysms. Other etiologies included mycotic, dissecting, and connective tissue disorders, extension of arch aneurysms, and traumatic and iatrogenic pseudoaneurysms. Because of the devastating consequences of untreated innominate artery aneurysms, Bower et al10 have recommended operative treatment of all symptomatic and asymptomatic affected patients fit for surgical repair to avoid the natural history that inevitably leads to rupture or thromboembolism.
Common Carotid Artery Aneurysms
True aneurysms of the common carotid arteries are very rare. In fact, pseudoaneurysms of the carotid arteries are considerably more frequent and usually result from complications of carotid reconstructions, blunt or penetrating trauma, carotid dissections, or infection.18,19 The vast majority of the true aneurysms of the carotid arteries are degenerative20; other less frequent causes include fibromuscular dysplasia, Marfan syndrome, Behçet’s disease and Takayasu’s arteritis.19,21 Bilateral common carotid artery aneurysms are extremely unusual, generally associated with Takayasu’s arteritis.22 Carotid bifurcation and internal carotid artery aneurysms are discussed in Chapter 103.
Clinical Presentation
Symptoms
Given the prevalence of imaging in modern medical practice, most arch vessel aneurysm are discovered incidentally and only 25% demonstrate symptoms at the time of diagnosis.7 Presenting symptoms include (1) chest, neck, and shoulder pain from acute expansion or rupture; (2) upper extremity acute and chronic ischemic symptoms from thromboembolism; (3) upper extremity pain and neurologic dysfunction from brachial plexus compression; (4) hoarseness from compression of the right recurrent laryngeal nerve; (5) respiratory insufficiency from tracheal compression; (6) transient ischemic attacks and stroke from thromboembolism in the vertebral and carotid circulations; (7) dysphagia from esophageal compression in cases of aberrant right subclavian artery; and (8) hemoptysis from erosion into the apex of the lung. Tracheobronchial or esophageal fistulization from contiguous arch vessel aneurysms can also occur. In a recent review of published reports on subclavian aneurysms, Vierhout et al12 found that the presenting symptoms were local (pulsating mass, shoulder pain, or nonspecific chest pain) in 51% of reported cases, compressive (dysphagia, dyspnea, brachial plexopathy, Horner’s syndrome, hoarseness) in 36% and embolization (cerebral or digital) in 16%. Hemorrhage (9%) and thrombosis (6%) were relatively infrequent.
Signs
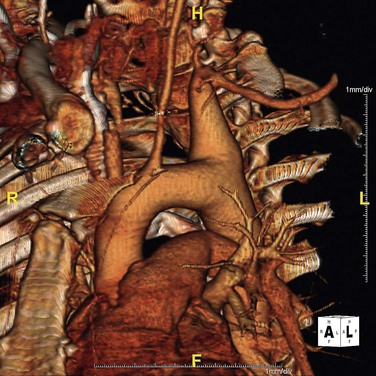
Patients without symptoms may be diagnosed through imaging studies for unrelated conditions (Fig. 140-1). In cases of subclavian artery aneurysms, patients may note the presence of a supraclavicular pulsatile mass. Most asymptomatic pulsatile masses in this area, however, represent tortuous and elongated common carotid and subclavian arteries and not necessarily aneurysmal degeneration. These masses can usually be distinguished from true aneurysms by duplex ultrasonography, computed tomography (CT), or magnetic resonance (MR) angiography. In addition to a supraclavicular mass, physical signs may include (1) a supraclavicular bruit, (2) absent or diminished pulses in the upper extremity, (3) normal pulses with signs of microembolization (“blue finger” syndrome), (4) sensory and motor signs of brachial plexus compression, (5) vocal cord paralysis, and (6) Horner’s syndrome resulting from compression of the stellate ganglion and other contributions to the cervical sympathetic chain at the base of the neck.23
Imaging
Plain films of the chest may reveal a superior mediastinal mass that may suggest the presence of a neoplasm. Ultrasonography, MR or CT imaging establishes the diagnosis. Conventional arch and upper extremity angiography, or MR or CT angiography are important to delineate the extent of the aneurysm, to assess the sites of vascular occlusion in cases complicated by thromboembolism, to note the competency of the contralateral vertebral circulation if the ipsilateral vertebral artery originates from an aneurysmal vessel, and to assess anatomic suitability for endovascular repair. These points are essential in planning appropriate management—that is, surgical reconstruction or endovascular repair.
Open Surgical Repair
Contemporary surgical repair of arch vessel aneurysms involves resection or endoaneurysmorrhaphy and reestablishment of arterial continuity with an end-to-end anastomosis (for very small aneurysms) or, more commonly, an interposition arterial prosthetic graft. Although proximal and distal ligation of arch vessel aneurysms occasionally has been successful in the past, ligation without direct or extra-anatomic reconstruction generally should not be performed because ischemic symptoms develop in 25% of cases so treated.8
Innominate Artery Aneurysms
An anatomic classification of the extent of the aneurysm has been proposed by Kieffer et al17 to guide the surgical repair of aneurysms of the innominate artery (Fig. 140-2). Type A is confined to the innominate artery distal its origin. Type B is the most common and involves the innominate artery and its origin, whereas type C involves both the innominate artery and the ascending aorta. The innominate and proximal right subclavian arteries are usually exposed through a median sternotomy extended into the right neck. Proximal control of the innominate is obtained at the aortic arch. The right subclavian and right common carotid arteries are exposed and dissected for distal control. The aneurysm is resected, and reconstruction with a prosthetic graft is usually performed. For type A and B aneurysms, the proximal graft anastomosis is usually performed to the native ascending aorta proximal to the innominate origin. The graft is then anastomosed to the uninvolved distal innominate artery (Fig. 140-3). The origin of the innominate artery is oversewn with a running suture, or patch angioplasty of the aorta may occasionally be required. For lesions extending into the origins of the right subclavian or common carotid artery, a bifurcated graft can be used, or a branch graft to the subclavian artery can be sewn onto the graft going into the common carotid artery. The bifurcated configuration may sometimes be prone to compression or kinking when the sternum is closed, so caution should be taken to perform the proximal anastomosis in the lateral aspect of the ascending aorta. In cases of a bovine arch, additional graft reconstruction of the left common carotid artery may be necessary. Type C innominate artery aneurysms usually require aortic arch and innominate artery prosthetic graft replacement using cardiopulmonary bypass and hypothermic circulatory arrest.
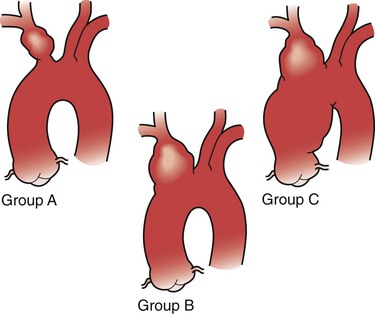
Figure 140-2 Classification of aneurysms of the innominate artery according to extent of involvement. A, Group A, no involvement of origin of the innominate artery. B, Group B, involvement of origin of the innominate artery but not of aorta. C, Group C, involvement of innominate artery and aorta. (From Kieffer E, et al: Aneurysms of the innominate artery: surgical treatment of 27 patients. J Vasc Surg 2:222, 2001.)
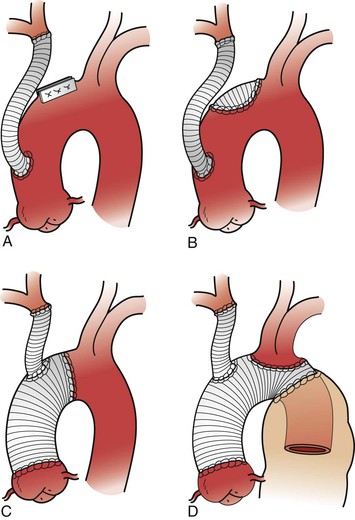
Figure 140-3 Techniques used for treatment of aneurysms of the innominate artery. A, Lateral suture of aorta. B, Patch angioplasty of aorta. C, Replacement of ascending aorta. D, Replacement of ascending aorta and transverse aortic arch in association with distal elephant trunk prosthesis (From Kieffer E, et al: Aneurysms of the innominate artery: surgical treatment of 27 patients. J Vasc Surg 2:222, 2001.)
Subclavian Artery Aneurysms
Subclavian artery aneurysms can be divided into proximal, typically degenerative, or distal, usually related to thoracic outlet syndrome. For proximal right subclavian aneurysms, median sternotomy with extension into the supraclavicular fossa is usually necessary to gain adequate exposure for proximal control. Supraclavicular and infraclavicular incisions may be used to mobilize the proximal and distal subclavian artery. Resection of the clavicle also offers excellent exposure of the subclavian artery. Partial medial clavicular resection is rarely necessary, although it may be helpful for proximal subclavian artery exposure when median sternotomy is not feasible. The supraclavicular incision is extended medially, and the fascia and periosteum are incised. The origins of the sternocleidomastoid and pectoralis major muscles are reflected subperiosteally, the first superiorly, and the second inferiorly. The medial third of the clavicle is disarticulated and subperiosteally resected with care to avoid injury to the subclavian vein. In cases of proximal left subclavian aneurysms, a left thoracotomy combined with supraclavicular exposure may be necessary.
Extra-anatomic reconstruction combined with proximal and distal aneurysm ligation has also been described in unusual circumstances.24 For aneurysms involving the midsubclavian artery and the distal subclavian artery, a supraclavicular incision often gives adequate exposure and may be complemented by an infraclavicular incision for distal control. Alternatively, proximal and distal control may be obtained endovascularly using balloon occlusion catheters placed angiographically. Division or resection of the midportion of the clavicle may be necessary to gain additional exposure; if so, the clavicle may be reconstructed at the completion of the operation. If the aneurysm involves the origin of the vertebral artery, reconstruction by reimplantation or other means is appropriate, particularly if this is the dominant vertebral artery or for cases in which the contralateral vertebral artery is hypoplastic or diseased.
Results
Aneurysm resection with graft replacement is durable and yields excellent long-term results. In one of the largest reported series, normal upper extremity circulation was maintained, and there were no procedure-related complications during a mean follow-up of 9.2 years.8 Although open repair frequently results in durable and excellent long-term outcomes, considerable associated morbidity and mortality has been reported. In-hospital mortality could be as high as 11% according to a report of open repair of innominate artery aneurysms, in which 18% of patients required prolonged ventilation.17 Since many patients with true aneurysms are unfit for open repair because of their advanced age and multiple comorbidities, careful patient selection is mandatory to improve outcomes. Relative contraindications to open repair also include severely compromised pulmonary function, prior sternotomy or left thoracotomy, and hemodynamic instability secondary to multiple trauma.
Endovascular Repair
Endovascular repair is an attractive option for patients unfit for open repair because it is associated with lower morbidity and mortality. Many reports of endovascular repair of arch vessel aneurysms, particularly those involving the innominate and the subclavian artery, have been published in recent years.25–31 This has led to treatment of better risk patients with appropriate anatomy, to avoid the morbidity of open surgery. Endovascular treatment can be especially helpful in cases of actively bleeding coagulopathic patients with iatrogenic, catheter-induced, or other penetrating injury of the arch vessels.11,32–37 Aneurysms secondary to connective tissue disorders may also be more suitable for endovascular repair to avoid direct resection and anastomoses to diseased vessels, although long-term outcomes are not known.38
Anatomic Considerations
The proximal portion and midportion of the subclavian artery are most amenable to endovascular treatment. However, several anatomic limitations exist. It is unusual for true subclavian or innominate aneurysms to have adequate proximal and distal landing zones. Also, coverage of branch vessels, such as the right carotid, vertebral arteries, and left internal mammary when it has been used for coronary bypass, may not be feasible. Endografts crossing the first rib may be subject to extrinsic compression. The distal subclavian artery is located between the clavicle and the first rib, and endografts in this location are subject to compression, deformation, and fracture.35–37,39,40 Another potential complication of endograft placement in the right subclavian artery is stroke from embolic debris dislodged into the right common carotid artery.37 The vertebral artery origin is vulnerable on both sides and may be covered during stent-graft deployment. This usually is well tolerated when the contralateral vertebral artery is patent and of adequate size. Posterior circulation stroke may occur, however, when the contralateral vertebral artery is highly stenotic, hypoplastic, or occluded. In this circumstance, the ipsilateral vertebral artery should be revascularized by end-to-side anastomosis to the common carotid artery or other means. Whenever the origin of the vertebral artery is involved by the aneurysm, coil embolization of the ipsilateral vertebral artery is desirable to prevent future branch vessel endoleaks.
Technique
Endovascular repair of subclavian or innominate artery aneurysms is usually performed through a transbrachial or transfemoral approach. A transaxillary approach has occasionally been necessary.38 Both balloon-mounted and self-expandable endografts have been used off label for endovascular repair of arch vessel aneurysms.41 The most frequently used endografts include the Wallgraft (Boston Scientific, Natick, Mass), Viabahn (W.L. Gore & Assoc, Flagstaff, Ariz), or Fluency (C.R. Bard, Inc, Murray Hill, NJ).42 Most contemporary endografts usually require 7F to 9F delivery sheaths, depending on endograft diameter. Larger endografts, however, such as those required for endovascular repair of innominate artery aneurysms, require still large introducer sheaths, usually 11F or 12F. The more flexible Viabahn endograft may be more suitable in cases of considerable arterial tortuosity. Lower-profile devices, such as the balloon-mounted iCast endograft (Atrium Medical, Hudson, NH), which is currently available up to 10 mm in diameter, can be delivered through a 7F sheath. Of note, the largest iCast endograft can potentially be dilatated up to 14 mm in diameter. Because of discrepancy in proximal and distal landing zone diameters, a combination of endografts of different sizes may be necessary. Furthermore, given the rigidity of balloon-mounted endografts, these may be used for accurate proximal deployment at the level of the ostium of the vessel and combined with more flexible distal self-expanding endografts. A novel approach is the use of multilayer stents to cause aneurysm thrombosis while maintaining flow through branch vessels.43 Although technically feasible, mid- and long-term results of these techniques have yet to be reported to accept them as valid alternatives for the treatment of aneurysms.
Hybrid Operations
In this minimally invasive approach, embolization with coils or a vascular plug of a proximal subclavian artery aneurysm (not involving the origin) is combined with subclavian artery transposition or carotid-subclavian bypass, avoiding placement of an endograft.44 Complete exclusion of the subclavian aneurysm is facilitated by ligation of the subclavian artery proximal to the distal anastomosis of the carotid-subclavian bypass. These procedures can be staged or combined in an operating room equipped with high-resolution imaging equipment. As with endograft placement, care must be taken to preserve the vertebral artery, if the contralateral vertebral artery is inadequate, and the left internal mammary when it has been or is anticipated that will be used for coronary bypass.
Off-label use of iliac limb endografts has been reported for the exclusion of right subclavian as well as innominate artery aneurysms combined with carotid-subclavian or carotid-axillary bypass (Fig. 140-4).45–47 This technique introduces the endograft into the innominate artery in a retrograde fashion using the carotid-subclavian bypass limb as a conduit before anastomosis to the subclavian artery. Cerebral embolization is a risk and may be minimized by occluding antegrade carotid flow during endoprosthesis introduction and deployment.45
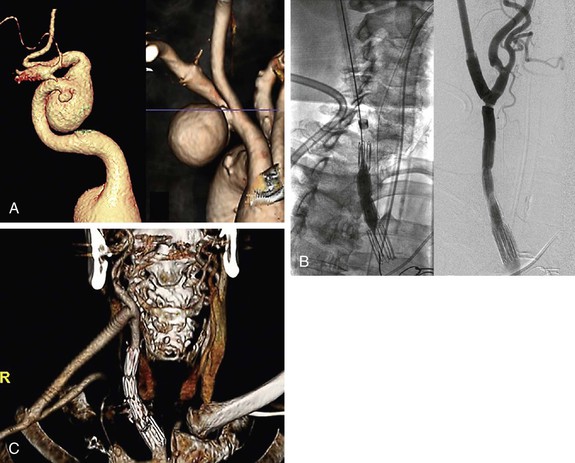
Figure 140-4 A, 3D CT volume rendering of right subclavian artery aneurysm. B, Deployment of iliac extender limb via a right carotid conduit placed for bypass to the right axillary artery after exclusion of right subclavian artery aneurysm. C, Follow-up CTA of the excluded aneurysm and patent carotid-axillary bypass. (From Bruen KJ, et al: Hybrid management of proximal right subclavian artery aneurysms. J Vasc Surg 53:528, 2011).
With the introduction of endografts specific for endovascular treatment of thoracic aortic aneurysms, hybrid procedures have become feasible for more proximal aneurysm of the great vessels extending into the aortic arch. In these procedures, exclusion of the orifice of aneurysmal arch vessels is combined with thoracic endovascular aortic aneurysm repair and extra-anatomic arch vessel revascularization (i.e., carotid-carotid, subclavian transposition and carotid-subclavian bypass).31,48
Results
Because of the low incidence of arch vessel aneurysms, only small case series and case reports are available to assess outcomes of endovascular treatment of these aneurysms. For nonatherosclerotic aneurysms such as those due to connective tissue disorders,41,49 Takayasu’s arteritis,46 or infections such as HIV,47 only case reports are available and reveal acceptable outcomes. However, there is an inherent bias in case reports since successful outcomes are primarily published. Thus the long-term durability of endovascular therapy, particularly endografts, in arch vessels is unknown. Short-term patency for subclavian stent grafts ranges from 83% to 100% over a mean follow-up of 7 to 29 months.29,34–36,50 Endograft compression, deformation, and fracture and stenosis from intimal hyperplasia have been reported and may limit the applicability of endovascular repair in this location.32–34 Bruen et al45 reported a case series of four patients with right subclavian aneurysms treated with carotid-axillary bypass and retrograde placement of iliac limb endografts across the innominate bifurcation into the common carotid artery. Mean follow-up time was 232 days (range, 50-564) with 100% patency of the endograft limbs and bypass grafts. No endoleaks were found on follow-up scans. Two of the four patients suffered a minor stroke.45 Cury et al7 reported on the experience at the Cleveland Clinic in treating supra-aortic vessel aneurysms that included 11 patients treated endovascularly. Eight of these aneurysms were of the subclavian artery. In this series, one death occurred in the endovascular group, with no endoleaks and no sac enlargement in the follow-up period. Patency rates were not reported. In the series of Andersen et al,31 outcomes of 13 hybrid or completely endovascular repairs of intrathoracic subclavian artery aneurysms were reported. All patients underwent repair with thoracic aortic stent graft placement with (10/13) or without (3/13) revascularization. One death (7.7%) occurred within 30 days after urgent zone 0 hybrid arch repair for an aberrant subclavian artery-esophageal fistula. One incidence of stroke was reported. Though these case series are small, they provide encouraging results for continued advancement of endovascular therapy for these complex lesions. Open surgical repair remains, however, the preferred approach for good-risk patients with subclavian and innominate artery aneurysms.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree