Types of Pacemakers and the Hemodynamics of Pacing
Permanent Pacemaker Types
Pacemaker Code
The pacemaker code is a mechanism to briefly describe types of pacemakers (Table 5-1). The code has evolved over several years to accommodate changes in pacing systems and there have been recommendations for up to a five-position code with multiple letters. From a practical point of view, the four-position code described here represents the general usage.
Position I refers to the chamber(s) being paced. V stands for ventricle, A stands for atrium, and D stands for dual (atrium and ventricle). There is really no O in this setting (an older implantable cardioverter defibrillator that did not have pacing backup could be designated O, but this is of historic interest only). Manufacturers will often designate S for single. This means it can be used to pace either the atrium or the ventricle. They are simply describing it more accurately and not designating it as one or the other since it can be used for either.
Position II refers to the chamber(s) being sensed. Again, V is for ventricle, A is for atrium, and D is for dual (atrium and ventricle). Again, the designation of S is often used by the manufacturer in a generic manner because of its potential application for either atrial or ventricular placement. In position II, the designation O refers to absent sensing (and thus refers to fixed, asynchronous pacing). When a magnet is placed over most pacemakers, the sensing is disabled; for instance, a VVI pacemaker would become VOO.
Position III refers to the device’s response to sensing. I represents the inhibited mode, meaning that when the pacemaker senses an event, it will be inhibited from further pacing; this is the most common form of sensing. T indicates a triggered response. When the pacemaker senses an event, it will trigger the device to deliver a pacing stimulus. In single-chamber situations, the sensed event and triggered impulse occur within the same chamber. This
is rarely used. An example of its use would be to program a VVI pacemaker to a VVT. In that case, a sensed event would also trigger a pacer spike. This would, of course, be useless if a normal QRS were sensed. On the other hand, VVT can be used as a diagnostic device to see if a T wave was being sensed (a spike would appear on the T wave). Modern devices allow evaluation of such problems in other ways and VVT is really of historic interest.
is rarely used. An example of its use would be to program a VVI pacemaker to a VVT. In that case, a sensed event would also trigger a pacer spike. This would, of course, be useless if a normal QRS were sensed. On the other hand, VVT can be used as a diagnostic device to see if a T wave was being sensed (a spike would appear on the T wave). Modern devices allow evaluation of such problems in other ways and VVT is really of historic interest.
TABLE 5-1 Pacemaker code | ||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||
When dual-chamber terminology is introduced, many new to pacing are confused by the third D. The third D refers to the ability to trigger a spike or to inhibit. In particular, a sensed P wave in the atrium allows a triggered ventricular response in the ventricle.
An easier way to explain this is to discuss a type of pacemaker that is no longer available. The VAT pacemaker would sense in the atrium and then after an appropriate AV delay, trigger a spike in the ventricle. The original ideal patient for this would have been an active person with significant heart block. Simply putting in a VVI pacemaker would cause pacing with no relation to the P waves and lose all the potential advantages of AV synchrony. An early pacemaker was designed with a lead to the atrium that would sense the P wave and then, after an appropriate AV delay to allow ventricular filling, the pacemaker triggered a spike in the ventricle. This would lead to AV synchrony. It would have the advantage, in an active person, of tracking the P waves at an increased, appropriate, physiologic heart rate with an appropriate AV interval.
The rest of the VAT pacemaker discussion is simply to describe the term trigger. Even the novice can envision numerous potential problems with this device. Atrial flutter could cause the heart to race inappropriately. If the patient developed sinus node incompetence, there would be no way to pace the atrium. If frequent PVCs occurred or if intermittent normal AV conduction
occurred, the device would be pacing unnecessarily in the ventricle. This is of historic interest only and is basically to describe the concept of the triggered response in a dual-chamber pacemaker.
occurred, the device would be pacing unnecessarily in the ventricle. This is of historic interest only and is basically to describe the concept of the triggered response in a dual-chamber pacemaker.
Position IV, at one point had numerous options, but currently position IV will simply have an R added if the patient has rate modulation, in which a sensor is used to modify the heart rate of the pacemaker based on the patient’s activity or metabolic need (see Chapter 7).
Position V is rarely used nowadays. It refers to antitachyarrhythmia function or functions. 0 = none, P = anti-tachyarrhythmia, S = shock, and D = dual (P + S). This nomenclature is really outdated with modern ICDs and from a practical point of view, only the first three letters are in common use and an R is placed at the end if rate modulation is an option with the device. Virtually all modern pacemakers contain rate modulation as an option (although it can be turned off if it’s not clinically necessary).
Single-Chamber Permanent Pacemakers
There are essentially only two forms of single-chamber pacing: VVI and AAI, with the former being the most common. Rate modulation is an option for either chamber. AAI pacing is selected for patients in whom the bradyarrhythmia is a sinus mechanism and AV block is not a problem and who do not have chronic or frequent atrial tachyarrhythmias. They also should not have silent atria, in other words, large dilated atria which cannot be stimulated.
VVI pacing is most commonly used for patients with chronic atrial fibrillation and a slow ventricular response. Pacing or sensing the atrium in these patients is of no value. VVI pacing could be used in a patient with sick sinus syndrome as “backup pacing,” but during those times of pacing, AV synchrony would not be maintained (if the episodes of asystole are very rare and/or the patient is extremely inactive, this may not present a significant clinical problem). The addition of rate modulation (AAIR or VVIR) is indicated when sinus node function is abnormal. Chronotropic incompetence is a common form of abnormal sinus node function in which appropriate increases in sinus rate do not occur.
As noted above, the AAT and VVT modes are mainly of historic interest only. A patient could have a pacemaker programmed to AAT or VVT to see if any extraneous electrical activity is being sensed by the pacemaker. Extraneous electrical activity would cause a pacemaker spike at the time of sensing and could be used for diagnostic purposes. Generally, other approaches are used in the more modern pacemaker era.
In the past, one use of the AAT mode was in the assessment of atrial sensing with some DDD devices in patients who were not pacemaker dependent. For example, first reprogram to the AAT mode with an atrial pacing rate less than sinus rate and a unipolar atrial pacing configuration (bipolar can also be used, but as noted before, unipolar is easier to visualize on an ECG strip or monitor). The atrial sensitivity setting is then progressively reprogrammed
from the least to the most sensitive values while simultaneously observing the ECG. As soon as atrial sensing is reached, triggered atrial stimuli will begin to appear within the P wave on the ECG. Until then (at less sensitive values), clinicians will observe atrial stimuli, at the programmed rate, that are dissociated from the native P waves. In this way, one can determine at what level atrial sensing occurs and program the appropriate sensitivity. Most current pacemakers have built-in automatic sensing threshold determination as a standard feature. New technology, such as the availability of visualizing the intracardiac atrial electrogram and the use of marker channels, has replaced the more cumbersome AAT mode technique.
from the least to the most sensitive values while simultaneously observing the ECG. As soon as atrial sensing is reached, triggered atrial stimuli will begin to appear within the P wave on the ECG. Until then (at less sensitive values), clinicians will observe atrial stimuli, at the programmed rate, that are dissociated from the native P waves. In this way, one can determine at what level atrial sensing occurs and program the appropriate sensitivity. Most current pacemakers have built-in automatic sensing threshold determination as a standard feature. New technology, such as the availability of visualizing the intracardiac atrial electrogram and the use of marker channels, has replaced the more cumbersome AAT mode technique.
Dual-Chamber Permanent Pacemakers
Benefits of Maintaining AV Synchrony
Engineers and electrophysiologists have attempted to mimic sequential atrial and ventricular electrical activation of the heart with artificial pacemakers for decades. A permanent AV sequential cardiac pacing became reliable only with advances in pulse generator technology, battery longevity, stable atrial lead systems, and miniaturization of circuitry. The benefits of maintaining AV synchrony are discussed briefly in the next section.
Physiologic Timing of Atrioventricular Valve Closure
With a patient in sinus rhythm and VVI pacing, the possibility exists of poorly timed atrial contraction in relation to ventricular contraction. If the atria contract at or about the same time that the ventricles contract, low cardiac output and pulmonary congestion result. Inappropriate AV synchrony can result in the pacemaker syndrome. Symptoms may include fatigue, lightheadedness, shortness of breath, chest pain, and even syncope. These symptoms can be related simply to AV dissociation or to the development of retrograde AV nodal conduction. Symptoms that were supposed to be alleviated by the implantation of a pacemaker may recur in the form of pacemaker syndrome.
Improved Cardiac Output
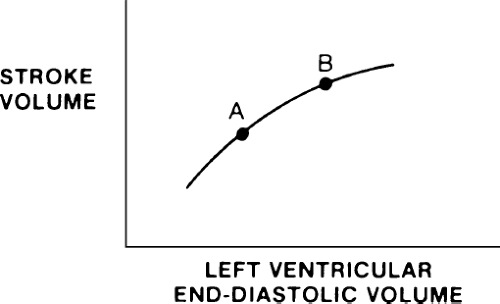
An increase in stroke volume and cardiac output occurs when ventricular filling is augmented by atrial contraction as a result of the Frank–Starling relationship. When the atrium quickly contracts, ventricular volume at the end of diastole is greater so the ventricle begins its contraction higher on its function curve (Fig. 5-1). Augmentation of ventricular stroke volume by atrial contraction is most important in stiff, noncompliant hearts, as may be seen in patients with congestive heart failure, chronic hypertension, and so forth. The improved stroke volume with properly timed atrial contraction carries no significant additional myocardial oxygen demand and allows the heart to
work higher on its ventricular function curve without an appreciable increase in mean pulmonary capillary pressure. Thus, the improved cardiac output occurs without increased risk for pulmonary congestion.
work higher on its ventricular function curve without an appreciable increase in mean pulmonary capillary pressure. Thus, the improved cardiac output occurs without increased risk for pulmonary congestion.
If the patient has normal sinus node function with a normal chronotropic response to exercise, the dual-chamber pacemaker can allow the sinus node to increase normally in response to exercise and “track” with appropriate ventricular pacing to increase cardiac output and improve the sense of well-being in a patient who is exercising.
A potential benefit of maintaining AV synchrony is a reduction of supraventricular tachyarrhythmias. This benefit, however, is not well established.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree