Indications for Pacing
Indications For Permanent Pacemaker Therapy
Any physician implanting pacemakers must be familiar with the American College of Cardiology/American Heart Association/North American Society Pacing Electrophysiology (now termed the Heart Rhythm Society) Guidelines that are published intermittently in their various journals. Only a brief summary of basic concepts is discussed here.
Symptoms of a slow heart rate may include syncope, dizziness, and transient confusion. Less commonly, a chronically slow heart rate can lead to fatigue, dyspnea, poor exercise ability, and rarely, frank congestive heart failure. All of these clinical manifestations are more commonly caused by other etiologies. The decision to place a pacemaker must be based on an understanding of the indications for pacing, as well as knowledge of anatomy and physiology, put in context of the individual patient. For instance, syncope is clinically most often due to “neurocardiogenic syncope”—a sudden drop in blood pressure and/or heart rate that leads to fainting. The young healthy person who has had a single episode of fainting at the sight of blood does not need pacemaker implantation even if transient asystole were to accompany the event. Transient asystole in an elderly person with sick sinus syndrome could cause serious injury due to syncope with collapse.
The tools to evaluate the patient are the history and physical, the EKG, and the monitoring rhythm strip, ideally a rhythm strip taken during the symptomatic episode (although this is often not possible). Twenty-four-hour ambulatory monitoring can be useful in patients with daily symptoms. Usually, a more productive approach is to use an event monitor in an attempt to capture a rhythm during symptoms over a period of time, typically 4 weeks. An implantable loop recorder, which is placed beneath the skin, can monitor for tachy- or bradyarrhythmias for many months.
Electrophysiologic testing for bradyarrhythmias due to sick sinus syndrome is currently suboptimal. Pacing the atrium in the area of the sinus node and checking the length of time it takes for the sinus node to recover is not a
particularly sensitive or specific test for sick sinus syndrome. Types of heart block can be more accurately assessed with a His bundle study, discussed in the section, “His-Purkinje System.”
particularly sensitive or specific test for sick sinus syndrome. Types of heart block can be more accurately assessed with a His bundle study, discussed in the section, “His-Purkinje System.”
The Cardiac Electrical System
Automaticity
All of the electrically active cells of the heart have an inherent automaticity, meaning that with time they will gradually depolarize and then “fire.” The sinus node is a small collection of cells in the upper portion of the right atrium near the insertion of the superior vena cava. This is the normal pacemaker of the heart, the top of the hierarchy. A typical heart rate would be 70 beats per minute (bpm) in a healthy person. The sinus rate responds to various physiologic events and increases in rate with exercise, fever, emotional stress, or other factors and decreases in rate with rest or increased vagal tone. The majority of these changes are mediated by the sympathetic and the vagal system.
The cells of the atrial myocardium, excluding the sinus node, are not particularly good pacemakers themselves. Occasionally there can be areas in the atrium that can become automatic or fire early leading to an atrial premature contraction or an atrial tachycardia.
A slow sinus heart rate can allow the AV node to fire and pace the heart with a junctional rhythm. This tends to be a very steady rhythm often at a rate of about 40 or 50 bpm. Even if the sinus node were surgically removed, the junctional rhythm would take over in a normal person. Digitalis toxicity, myocarditis, cardiac surgery, and ischemia can lead to a more rapid junctional rhythm called “nonparoxysmal junctional tachycardia.”
At the bottom of the hierarchy is the ventricle. The ventricular escape rhythm in the setting of complete heart block is an ominous rhythm, usually at a very slow rate, perhaps in the 20s or 30s. This rhythm is potentially lethal if it becomes too slow, mainly due to prolongation of the QT interval resulting in polymorphic ventricular tachycardia.
Sinus Node and Atrium
The sinus node itself is, physically, a relatively small group of cells and is not routinely recorded with electrophysiologic studies and standard intracardiac catheters. The sinus node responds to various physiologic stimuli, going slow or fast, as appropriate. Rate-adaptive pacemakers try to reproduce this with varying degrees of success.
The atrium conducts electricity from the sinus node down to the AV node. This forms a P wave on the electrocardiogram. The atria push blood into their respective left and right ventricles improving cardiac output through the Frank–Starling mechanism (See Chapter 5, Fig. 5-1). Maintaining
atrial–ventricular synchrony is an important goal with dual-chamber pacemakers. The atria are the location of two of the most common pathologic rapid rhythms: atrial fibrillation and atrial flutter. Sometimes with atrial fibrillation and flutter, rapid rhythms may alternate with episodes of bradycardia (bradycardia-tachycardia syndrome). Also, pharmacologic attempts to control a rapid ventricular response associated with atrial fibrillation and atrial flutter can lead to episodes of inappropriately slow ventricular responses requiring a pacemaker.
atrial–ventricular synchrony is an important goal with dual-chamber pacemakers. The atria are the location of two of the most common pathologic rapid rhythms: atrial fibrillation and atrial flutter. Sometimes with atrial fibrillation and flutter, rapid rhythms may alternate with episodes of bradycardia (bradycardia-tachycardia syndrome). Also, pharmacologic attempts to control a rapid ventricular response associated with atrial fibrillation and atrial flutter can lead to episodes of inappropriately slow ventricular responses requiring a pacemaker.
AV Node
The atria are separated from the ventricles by the two atrioventricular valves and the supporting fibrous tissue (essentially acting as an “insulator” separating the upper and lower chambers). The only normal electrical pathway is through the AV node. This can be viewed, teleologically, as the source of a brief delay in conducting the depolarization wave from its atria to the ventricles, which allows blood to be pumped from the atria into the ventricles, for more efficient cardiac output. Electrical conduction through the AV node is so slow and of such small amplitude that is does not show up on even intracardiac electrodes. The AV node is responsive to vagal and sympathetic input. A highly trained athlete can have asymptomatic episodes of intermittent block in the AV node due to high vagal activity as a normal variant. The node itself, like all electrically conducting tissue, can become fibrotic and develop conduction block severe enough to require pacemaker therapy.
His-Purkinje System
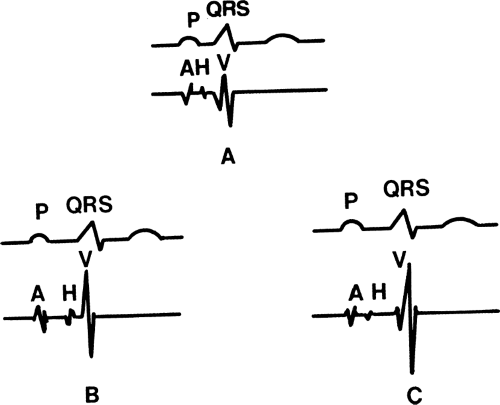
After electrical activity has been slowed in the AV node, it enters a very rapidly conducting set of specialized conducting tissue, the His-Purkinje system. The bundle of His is the initial portion and is a fairly thick bundle of cells. Its electrical activity routinely shows up on an appropriately done intracardiac electrophysiologic evaluation (but not on the surface ECG), as the His spike (Fig. 1-1). Isolated heart block in this particular anatomic structure is relatively uncommon. When it occurs it is categorized as infranodal block and is a potentially dangerous form of heart block. The bundle of His almost immediately splits into components of the Purkinje system. These are the left and right bundles. The left bundle is divided into the left anterior and left posterior fascicles (thus the term trifascicular block for infranodal complete heart block). This could be viewed, again teologically, as a rapidly conducting electrical system that spreads through the left and right ventricular myocardium to allow almost simultaneous, synchronized, contraction of the ventricles (the newer approach of cardiac resynchronization therapy for congestive heart failure represents an effort to reproduce this effect). Disruption of these bundles is quite common and left bundle branch block
(LBBB) and right bundle branch block (RBBB) are routinely diagnosed on EKGs. The clinical significance of this block is dependent on the clinical scenario and can range from completely benign to pathologic as discussed below.
(LBBB) and right bundle branch block (RBBB) are routinely diagnosed on EKGs. The clinical significance of this block is dependent on the clinical scenario and can range from completely benign to pathologic as discussed below.
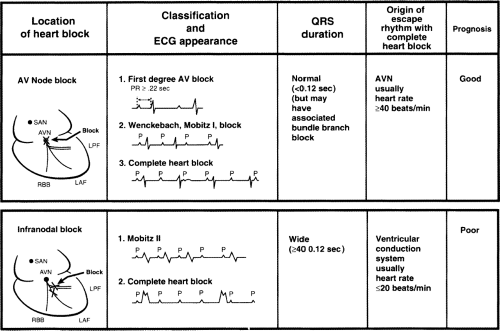
Nomenclature of AV Block
Mobitz type I block is characterized by gradual lengthening of the PR interval in sequential beats until there is a nonconducted P wave (Fig. 1-2). One important way to identify this is to look for a difference in the PR interval of the beats preceding and following the dropped beat. With Mobitz I second-degree AV block, the AV node has had time to recover after the dropped beat and the PR interval will be shortest after the dropped beat, compared to all other PR intervals. This type of block usually occurs in the AV node and the native QRS complex is narrow, unless there is coincidental bundle branch block present. The term Mobitz I block can be a description of block in other parts of the conduction system. For our purposes, we will assume the more common occurrence, block in the AV node.
Mobitz type II second-degree AV block is described as a dropped P wave, but with no progressive lengthening of the PR interval before the dropped P wave and no difference in the PR interval before or after the dropped beat (Fig. 1-2). This type of block occurs almost exclusively in the His bundle or the Purkinje system. Block in the isolated His bundle is quite rare. If this did occur, then the subsequent QRS could be narrow. The much more typical situation is block in the Purkinje system and this is usually associated with wide QRS complex. A logical way to view this is that it is unlikely that all three major branches of the Purkinje system (right bundle, left anterior fascicle, and left posterior fascicle) would conduct simultaneously and then block simultaneously. Almost always two of the three fascicles are “broken” or not conducting, leading to a wide QRS complex and the third fascicle conducting intermittently.
It is of note that patients with 2-to-1 block, ventricular conduction with every other P wave, cannot be categorized into Mobitz I or Mobitz II block simply because you cannot tell if there is prolongation of the PR. On the other
hand, a long rhythm strip will often locate consecutively conducted beats and clarify the type of block.
hand, a long rhythm strip will often locate consecutively conducted beats and clarify the type of block.
Third-degree AV block, also known as complete heart block, describes the failure of any depolarizations to pass from the atria through the AV node and His-Purkinje system to the ventricle. The atria may beat regularly in response to the SA node (or the patient could be in atrial fibrillation). The ventricles beat independently in response to whatever intrinsic rhythm has taken over: the AV node, the His bundle (junctional rhythm), the Purkinje system, or cells in the ventricle. The escape rate below the AV node may be about 50 bpm with junctional rhythm (although this may be highly variable) or 0 to 40 bpm in the ventricle with a ventricular escape rhythm. Third-degree AV block is a potentially dangerous rhythm, depending on the clinical setting. For example, third-degree AV block can occur in the setting of an acute inferior wall myocardial infarction (MI) with block in the AV node and an adequate junctional rhythm. This is virtually always a transient event. If the heart rate is unduly slow, a temporary pacemaker is required. There are clinical situations in which observation is adequate with standby transcutaneous pacemaker and immediate availability of atropine to speed up conduction through the AV node, if required. This would be a relatively benign form of third-degree AV block. On the other hand, third-degree AV block due to chronic degenerative disease of the His-Purkinje system can lead to syncope or sudden cardiac death.
His Bundle Electrogram
Much of our understanding of the conduction anatomy of the heart has come from study of the intracardiac electrogram, often referred to as the His bundle electrogram. Depolarization of the AV node and the His bundle produces no deflection on the surface ECG; however, a closely spaced bipolar electrode can be positioned across the anterosuperior portion of the septal tricuspid valve leaflet, in close proximity to the His bundle. A depolarization spike originating from the common His bundle can be recorded (refer to the H spike in Fig. 1-1). On the intracardiac ECG, atrial (A) depolarization precedes the H spike, and ventricular (V) depolarization follows the H spike. The interval between the atrial and His depolarizations (AH interval) reflects conduction through the AV node. The HV interval is the result of conduction in the Purkinje system between the His bundle and the ventricles. Thus, AH interval prolongation indicates a conduction abnormality within the AV node (above the His bundle), and HV interval prolongation indicates an infranodal conduction abnormality in the Purkinje system (left and/or right bundle). A potential value of measuring the His bundle electrogram is to document an abnormally long HV interval. An interval of greater than 100 msec, implies a significantly diseased Purkinje system that, in the presence of worrisome symptoms, may even warrant pacing. Pacing the atrium rapidly with the development of infranodal block can also be an indication of a significantly diseased His-Purkinje system.
Indications for Pacemakers
Sick Sinus Syndrome
The sinus node itself may simply develop fibrosis and lose effectiveness, leading to bradycardia. If the heart rate is slow enough to cause symptoms and is not due to medication such as beta-blockers, verapamil, diltiazem, or other multiple drugs that may slow the heart rate, then pacemaker therapy is indicated. Normally this would include pacing the atrium (and possibly having a ventricular lead in case heart block occurs later) in order to maintain atrio ventricular synchrony. Some patients with sick sinus syndrome may require medications that slow the heart rate and this would also be an indication for pacemaker therapy. The term bradycardia-tachycardia syndrome applies to patients with rapid heart rates but who also have episodes of slow heart rate (this can occur even without medications that tend to slow the rapid rate). Such patients often require beta-blockers or calcium channel blockers, and the only way to control the bradycardia portion of the problem is with a pacemaker. Unfortunately, uncertain situations do occur. If a patient has a heart rate less than 40 bpm and symptoms that may be related to the bradycardia, but are not clearcut, then there is “circumstantial evidence” that this is due to the slow heart rate. A pacemaker may be indicated, but clinical judgment is required. No pacemaker is indicated if the heart rate is slow due to medications that can be stopped or exchanged for drugs that do not slow the heart rate, without risk to the patient. Some patients may have symptoms that, on careful evaluation, are clearly not the result of a slow heart rate. A slow heart rate by itself is not an indication for a pacemaker.
Heart Block
Third-degree and advanced second-degree heart block, whether in the AV node or infranodal block, that is associated with slow heart rate and symptoms, episodes of asystole greater than or equal to 3 sec, or “escape rates” less than 40 bpm even if the patient is asymptomatic, require a pacemaker. If the patient has a tachyarrhythmia or other medical problem requiring drugs resulting in symptomatic bradycardia (usually beta-blockers, verapamil, or diltiazem), he or she requires a pacemaker.
An iatrogenic cause of AV block is catheter ablation of an AV junction. The most typical scenario is a patient with atrial fibrillation with a rapid ventricular response that cannot be controlled with drugs, so therefore an ablation is done. This leaves the patient with complete heart block and a pacemaker is always required in this situation.
Some types of cardiac surgery can lead to complete heart block. For instance, aortic valve replacement can lead to injury to the AV node or His bundle. Some types of cardiac congenital operations lead to complete heart block.
Various forms of muscular dystrophy can be associated with heart block. In some situations the unusual step is taken of placing a “prophylactic” pacemaker in these patients with minor conduction system disease, even in the absence of second- or third-degree heart block and symptoms. These are rare indications for permanent pacing and decisions should be made in consultation with a knowledgeable expert. The “ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmic Devices” mentions specifically myotonic muscular dystrophy, Kearns-Sayre syndrome, Erb’s dystrophy (limb-girdle), and peroneal muscular atrophy.
Second-degree AV block leading to symptomatic bradycardia is an indication for a pacemaker. Typically, the more dangerous type of second-degree AV block is Mobitz type II second-degree AV block. On the other hand, particularly in elderly patients, disease in the AV node with Wenckebach phenomenon (Mobitz type I second-degree AV block) can lead to symptomatic bradycardia and the need for pacing. It is not always benign.
Mobitz type II second-degree AV block usually is accompanied by a wide QRS complex implying that two of the three fascicles are nonfunctioning and the third fascicle is intermittently blocked (the escape rhythm would then be a ventricular escape, if there is any escape rhythm at all). This is a strong indication for a pacemaker. There are relatively rare instances of Mobitz II second-degree block with a narrow QRS complex (implying block in the His bundle itself). This is uncommon, but most cardiologists would place a pacemaker in that setting.
Type I second-degree AV block can occur below the AV node and is a potential indication for pacing. This is generally found only with electrophysiologic testing and is rarely encountered or documented in routine practice.
Pacing for first-degree AV block is extremely rare. Occasionally a patient with prolonged first-degree AV block can have such a loss of AV synchrony that symptoms can occur, particularly in the setting of LV dysfunction. Mobitz I second-degree AV block could also lead to a similar clinical situation. If such a patient is symptomatic, it is usually due to the mitral and tricuspid valves being open when ventricular contraction occurs, because of the long PR delay. Pacing may be indicated in the neuromuscular disorders previously mentioned, even with just first-degree AV block, but expert consultation is recommended.
Alternating bundle branch block (episodes of LBBB alternating with RBBB) is an indication for pacemaker therapy. One of the recurrent themes we discuss is that infranodal block is a potentially dangerous type of block and the presence of alternating LBBB and RBBB implies that the entire Purkinje system is at risk.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree