We explored trends in acute myocardial infarction (AMI) event rates in Norway during 1994 to 2009 and trends in the 6-month, 1-year, and 3-year risk of recurrences after an incident AMI during 2001 to 2008 in men and women ≥25 years. Trends in AMI event rates (incident and recurrent) were analyzed using joinpoint regression analyses and expressed as annual percentage change (APC) in rates. Trends in AMI recurrences were explored using conditional risk models for ordered events in Cox regression. Analyses were stratified by gender and age group. Overall, AMI rates were stable during 1994 to 2002 but declined during 2002 to 2009 (APC = −2.0; 95% confidence interval [CI] −3.1 to −0.9 in men; APC = −2.1; 95% CI −3.8 to −0.5 in women). In the younger age group, rates declined during the whole study period in men (APC = −0.6; 95% CI −1.0 to −0.3) but not in women. Among older patients, no changes were observed during 1994 to 2002, whereas rates declined during 2002 to 2009 (APC = −2.6; 95% CI −3.8 to −1.4 in men; APC = −2.4; 95% CI −4.0 to −0.7 in women). During 2001 to 2008, in the older age group, the 6-month, 1-year, and 3-year risks of recurrences were reduced annually by 4.7%, 4.3%, and 5.4% in men and 5.2%, 5.0%, and 5.7% in women (all p trend <0.001), respectively. No changes were observed in the younger age group. In conclusion, favorable trends in AMI event rates and recurrences observed in Norway were mostly seen among patients aged 65+ years, whereas less favorable trends were observed among younger patients, especially among women.
Several studies have examined trends in acute myocardial infarction (AMI) hospitalization rates and found fluctuating trends in rates before the year 2000 and declines afterward. Most studies of AMI recurrences have mainly focused on prognosis after an AMI. Only few studies have examined trends in AMI recurrences; these were either conducted some time ago or restricted analyses to the first recurrence only. In Norway, no nationwide analyses on trends in AMI event rates or recurrences have been conducted to date. In this article, we explore (1) trends in AMI event rates in Norway during 1994 to 2009 and (2) trends in the risk of experiencing AMI recurrences within 6 months, 1 year, and 3 years after an incident AMI occurring during 2001 to 2008, with additional focus on gender and age group differences.
Methods
Cardiovascular disease in Norway (CVDNOR) is a multipurpose research project established in collaboration between the University of Bergen and the Norwegian Knowledge Centre for the Health Services. Detailed information on participants, objectives, and inclusion criteria is given elsewhere. Briefly, all hospital stays with a cardiovascular discharge diagnosis ( International Classification of Diseases (ICD)-9 codes 390 to 459 and ICD-10 codes I00 to I99), as either main or secondary diagnosis wase retrieved from all Norwegian hospitals during 1994 to 2009. Patients’ age and gender, date of admission, and discharge, up to 20 discharge diagnoses and information on medical and surgical procedures are included in the dataset (information used to assess co-morbidity). From the Cause of Death Registry, information on underlying cause of death was obtained for the hospitalized patients until 31 December 2009. Linkages were made possible using the unique 11-digit personal identification number.
For the purpose of this study, we included all hospitalizations with AMI as main or secondary discharge diagnosis and deaths with AMI as the underlying cause (ICD-9 code 410 and ICD-10 codes I21, I22) in men and women ≥25 years during 1994 to 2009. The study protocol was approved by the Regional Committee for Medical and Health Research Ethics, Health Region West.
The “index”AMI was defined as the first AMI hospitalization or AMI death for a given patient identified during 1994 to 2009. A “recurrent” event was defined as a new AMI hospitalization or AMI death occurring >28 days from a previous AMI hospitalization. The term “AMI event” includes both “index” and “recurrent” AMIs, unless otherwise specified. Hospitalizations and deaths occurring ≤28 days after a previous AMI hospitalization were considered to be related to the previous event and are not included in the analyses.
As previously done, “index” AMIs from 2001 onward were considered “incident,” based on the absence of a previous AMI hospitalization for the same patient during the previous 7 years. It has been shown that exclusion of previous AMI hospitalizations by a retrospective search of 7 years can identify with high accuracy the true “incident” event.
Continuous variables are presented as means and SD and categorical variables as counts and proportions. Independent sample t tests were used for comparisons of continuous variables. AMI event rates were calculated as number of AMI events for a given year (numerator) divided by the mid-year population of Norway in that year (denominator) and expressed per 100,000 persons. Similarly, we calculated age group–specific AMI event rates for patients aged 25 to 64 years and 65+ years.
Age-standardized AMI event rates were computed by the direct standardization method using 5-year age strata and the Norwegian population of year 2001 as standard population. The corresponding 95% confidence intervals (CIs) were calculated assuming a binomial distribution of events within the strata and using a normal approximation for the age-standardized rates.
Time trends in age-standardized AMI event rates were explored by joinpoint Regression Analyses using the Joinpoint software (Surveillance Research Program, US National Cancer Institute, version 4.0.1: srab.cancer.gov/joinpoint). The program detects points where trends deviate from being linear and introduces a “joinpoint” in that particular year. The analysis starts with 0 “joinpoints” (e.g., a linear trend) and tests whether any “joinpoints” should be added into the model. The annual percentage change (APC) in rates with 95% CIs is provided for each segment between 2 “joinpoints,” and a permutation test was used to select the model that best fitted the data.
In the analyses of risk of recurrences, patients with an incident AMI during 2001 to 2008 who survived beyond 28 days were followed for recurrences within 6 months, 1 year, and 3 years from their incident AMI. Trends in risk of recurrences were explored by conditional risk set models for ordered multiple failure data in Cox proportional hazard models. All recurrences in a patient (in case of more than 1) were included in the analyses. Calendar year of the incident event (the independent variable) was introduced as a continuous variable in the models. Hazard ratios obtained from the models represent the relative change in 6-month, 1-year, and 3-year risk of recurrences after an incident AMI between 1 calendar year and the previous. To show small differences between periods, we chose to report hazard ratios with 3 digits.
Results
During 1994 to 2009, a total of 291,338 AMI events (39.4% in women) were identified ( Table 1 ). Mean age (SD) at the event was 73.5 years (13.3). Men were on average 8 years younger than women at the time of the event (70.3 versus 78.4 years; p <0.001).
| Gender and Age Group | Index AMIs | Recurrent AMIs | Total AMIs |
|---|---|---|---|
| Men and women | |||
| 25+ yrs | 237,994 (81.7) | 53,344 (18.3) | 291,338 |
| 25–64 yrs | 62,378 (88.2) | 8,094 (11.5) | 70,472 |
| 65+ yrs | 175,616 (79.5) | 45,250 (20.5) | 220,866 |
| Men | |||
| 25+ yrs | 144,013 (82.3) | 30,975 (17.7) | 174,988 |
| 25–64 yrs | 49,718 (88.2) | 6,642 (11.8) | 56,360 |
| 65+ yrs | 94,295 (79.5) | 24,333 (20.5) | 118,628 |
| Women | |||
| 25+ yrs | 93,981 (80.8) | 22,369 (19.2) | 116,350 |
| 25–64 yrs | 12,660 (89.7) | 1,452 (10.3) | 14,112 |
| 65+ yrs | 81,321 (81.2) | 20,917 (20.5) | 102,238 |
∗ The first AMI hospitalization or AMI death in a given patient identified during 1994 to 2009.
† A new AMI hospitalization or AMI death occurring >28 days from a previous AMI hospitalization.
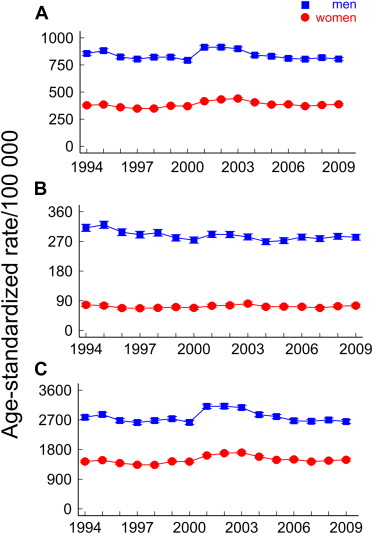
There were no statistically significant changes in AMI event rates during 1994 to 2002 in either men or women when both age groups were combined. During 2002 to 2009, overall event rates declined annually by 2% (APC = −2.0; 95% CI −3.1 to −0.9) in men and 2.1% (APC = −2.1; 95% CI −3.8 to −0.5) in women ( Figure 1 ; Table 2 ).
| AMI Event Rates | First Trend | Second Trend | Third Trend | |||
|---|---|---|---|---|---|---|
| Year | APC ∗ (95% CI) | Year | APC ∗ (95% CI) | Year | APC ∗ (95% CI) | |
| Men | ||||||
| 25+ yrs | 1994–1999 | −1.4 (−3.4, +0.5) | 1999–2002 | +4.0 (−4.6, +13.3) | 2002–2009 | −2.0 (−3.1, −0.9) |
| 25–64 yrs | 1994–2009 | −0.6 (−1.0, −0.3) | ||||
| 65+ yrs | 1994–1999 | −1.1 (−3.2, +1.1) | 1999–2002 | +5.4 (−4.0, +15.7) | 2002–2009 | −2.6 (−3.8, −1.4) |
| Women | ||||||
| 25+ yrs | 1994–1998 | −2.6 (−6.8, +1.9) | 1998–2002 | +5.6 (−1.2, +12.8) | 2002–2009 | −2.1 (−3.8, −0.5) |
| 25–64 ys | 1994–2009 | +0.1 (−0.5, +0.8) | ||||
| 65+ yrs | 1994–1998 | −2.4 (−6.5, +2.0) | 1998–2002 | +6.0 (−0.6, +13.0) | 2002–2009 | −2.4 (−4.0, −0.7) |
∗ APC in event rates within indicated periods is obtained from joinpoint regression analyses.
In men aged 25 to 64 years, we observed a small but statistically significant annual average decrease of 0.6% (APC = −0.6; 95% CI −1.0 to −0.3) in AMI event rates throughout the study period (1994 to 2009), whereas in women of the same age group, no changes were observed (APC = +0.1; 95% CI −0.5 to +0.8). In those aged 65+ years, event rates did not change during 1994 to 2002 but declined annually by 2.6% (APC = −2.6; 95% CI −3.8 to −1.4) in men and 2.4% (APC = −2.4; 95% CI −4.0 to −0.7) in women during 2002 to 2009 ( Figure 1 ; Table 2 ).
During 2001 to 2008, a total of 85,456 patients hospitalized for their incident AMI survived the first 28 days (83.5% of all patients hospitalized for an incident AMI), thus being at risk for recurrences. Of these, 6.7% and 9.6% experienced 1 or more recurrences within 6 months and 1 year, respectively. During 2001 to 2006, a total of 63,556 patients hospitalized for their incident AMI survived the first 28 days (82.8% of all patients hospitalized for an incident AMI). Of these 15.9% experienced 1 or more recurrences within 3 years. Results from the age-adjusted Cox regression analyses for trends in recurrences are listed in Table 3 .
| Gender | HR ∗ (95% CI) | ||
|---|---|---|---|
| 6-Month Recurrences † | 1-Year Recurrences † | 3-Year Recurrences ‡ | |
| Men | |||
| 25+ yrs | 0.963 (0.951–0.975) | 0.962 (0.952–0.972) | 0.960 (0.948–0.972) |
| 25–64 yrs | 0.992 (0.967–1.017) | 0.979 (0.958–1.001) | 1.004 (0.978–1.031) |
| 65+ yrs | 0.953 (0.939–0.967) | 0.957 (0.946–0.969) | 0.946 (0.933–0.960) |
| Women | |||
| 25+ yrs | 0.953 (0.939–0.968) | 0.955 (0.943–0.967) | 0.953 (0.939–0.966) |
| 25–64 yrs | 0.980 (0.938–1.023) | 0.990 (0.954–1.029) | 1.040 (0.990–1.092) |
| 65+ yrs | 0.948 (0.933–0.964) | 0.950 (0.938–0.963) | 0.943 (0.929–0.957) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


