Transradial Approach for Percutaneous Coronary Intervention
Adhir Shroff MD, MPH, FSCAI, FACC
Traditionally, percutaneous coronary intervention has been performed using the femoral artery as the point of entry. Femoral artery access has many advantages, including a relatively superficial location, large caliber, and lying above a stable surface to hold pressure (the head of the femur). In the United States, over 90% of diagnostic and interventional coronary procedures are performed via the femoral artery (1). There are well-known limitations of the approach, including bleeding and vascular complications, postprocedure pain, and prolonged immobility. Since the mid-1990s, it has been possible to use radial access to perform these procedures (2, 3 and 4). Despite relatively widespread adoption elsewhere, the United States has lagged in adoption of this technique (1). However, a growing interest in reducing bleeding complications in partnership with improved equipment has led to a surge in interest. In this chapter, the reader will gain an understanding of many of the basic concepts of performing coronary interventions using the transradial approach.
With the growing literature highlighting the adverse impact of bleeding coupled with improved equipment, there has been increased interest and adoption of the technique in the United States. There are several published reports now that have shown how specific US programs have successfully converted to predominantly radial access (5, 6, 7, 8 and 9).
CLINICAL EVIDENCE
In a large trial where patients were randomized by access site to either the femoral or the radial artery, the authors noted no difference in procedural success between approaches, while access-related complications were higher in the transfemoral group (3.71% vs. 0.58%, p = 0.0008). They did note a higher rate of access failure (3.5% vs. 0.2%, p < 0.0001) and radiation exposure (41.9 Gy cm2 vs. 38.2 Gy cm2, p = 0.034) among the radial patients in comparison with the femoral cohort (10). In terms of efficacy, Agostini et al. reported in a meta-analysis of 12 randomized trials that there was no difference in the rate of adverse cardiovascular events (2.1% vs. 2.4%; OR: 0.92; p = 0.7), despite a higher rate of procedural failure (7.2% vs. 2.4%; OR: 3.30; p < 0.001) between radial and femoral access strategies, respectively (11). In terms of safety, they demonstrated less entry site complications with the radial approach (0.3% vs. 2.8%; OR: 0.2; p < 0.0001). In the US-based National Cardiovascular Data Registry (NCDR), although the overall rate of transradial PCI was low (1.32%), there was a statistically significant lower risk of bleeding complications (OR: 0.42; 95% CI: 0.31-0.56) with similar procedural success (OR: 1.02; 95% CI: 0.92-1.12) (1). They noted that the reduction in bleeding complications was more pronounced in patients <75 years old, women and acute coronary syndrome patients.
There have been two meta-analyses that have studied the impact of access site on the treatment of acute myocardial infarction. Vorobcsuk et al. reviewed 12 prospective studies comprising 3,324 patients. Similar to prior studies of PCI, there was significantly less bleeding in the transradial group (p = 0.0001); however, they also noted a reduction in mortality (2.04% vs. 3.06%; OR: 0.54; p = 0.01) among patients in the transradial as compared with the femoral group (12). In a subsequent analysis of only randomized trials of access site for patients undergoing primary PCI, the radial approach was associated with lower mortality (OR: 0.53; 95% CI: 0.33-0.84) and reduced vascular complications (OR: 0.35; 95% CI: 0.24-0.53) than the femoral approach (13).
These observations were recently corroborated in a prospective, randomized trial. Jolly et al. reported the results of a large randomized trial of patients with acute coronary syndrome who were randomized to either radial or femoral access strategies. They observed no difference in the overall composite primary endpoint of death, myocardial infarction, stroke, or major bleeding at 30 days. However, among patients with STEMI, there was a benefit for radial over femoral access for the primary endpoint (p = 0.011) as well as for death (p = 0.001) (14). It should be noted that operator and institutional PCI volume had an impact on outcomes.
ANATOMICAL CONSIDERATIONS
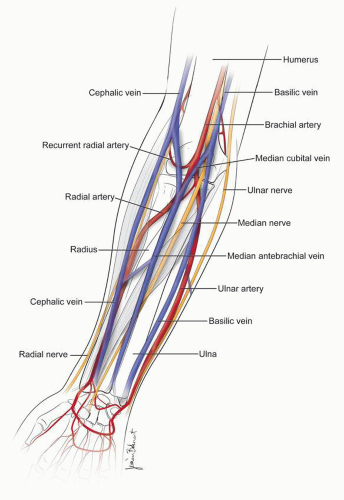
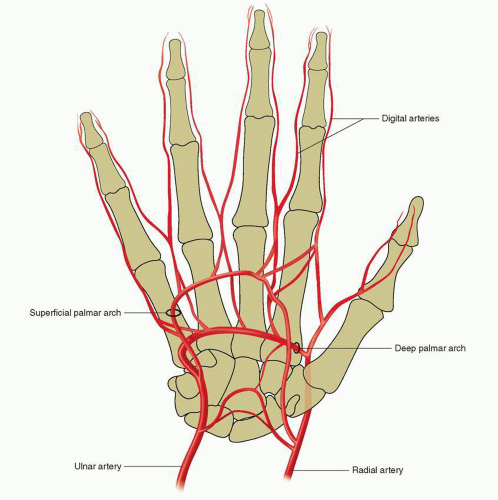
The brachial artery bifurcates near the antecubital space at the level of the elbow. With the hand supinated, the radial artery courses along the lateral surface toward the thumb, while the ulnar artery passes medially as it approaches the hand (Fig. 28-1). There are several variations of this anatomy, including radial-ulnar loops, brachial loops, stenotic lesions, excessive tortuosity, and anomalous origins of the radial artery (15) (Fig. 28-2). Although the “normal” anatomy is by far the most common, one must be aware of these common variations. After crossing the wrist joint, these arteries divide and form superficial and deep arches (Fig. 28-3), but several variations exist (16). The radial artery is relatively superficial even in the most obese patients and lies directly above the distal radius, which offers a reliable compressive surface.
The radial artery is considered a limb artery that is known to be more prone to spasm than somatic arteries such as the internal mammary arteries. The radial artery’s adventitial layer is innervated by sympathetic and parasympathetic nerves that may play a role in arterial spasm (17). The smooth muscle cells in the arterial wall will vasoconstrict in response to local factors and systemic hormones such as noradrenaline and angiotensin II.
CASE SELECTION
A stepwise approach is an important aspect of developing experience with a particular technique. Performing transradial PCI (TR-PCI) is no different. Several features have been associated with procedural failure. Advanced age, short stature, and prior coronary artery bypass graft (CABG) surgery are risk factors for procedural failure (18). Although female gender is not considered a relative contraindication, women are known to have smaller radial arteries and are more prone to spasm (19, 20 and 21).
While there is no definitive number of cases that ensures proficiency with the approach, some have suggested that after 50 cases (22) or 6 months (23), TR-PCI can be performed safely. There are some relative contraindications that may evolve as one’s experience with the technique grows, while the only real “absolute” contraindication is an absent radial artery (Table 28-1).
ANGIOGRAPHIC FEATURES
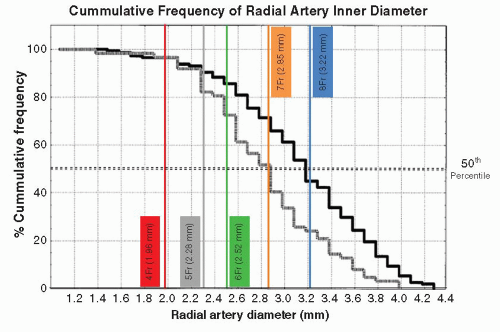
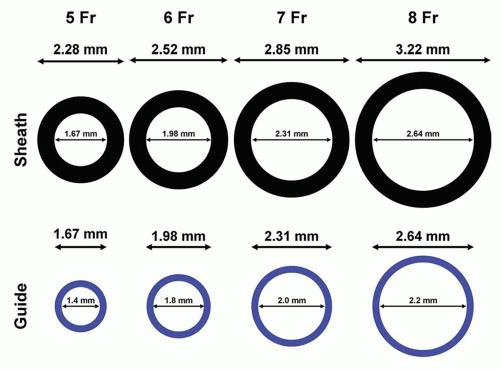
With respect to TR-PCI, this access site is limited by the relatively small caliber of the radial artery as compared with the femoral artery. In a study of Japanese patients, men were found to have larger average radial artery inner diameters compared with women (3.1 ± 0.6 mm vs. 2.8 ± 0.6 mm) (20) (Fig. 28-4). The variation in the diameter of radial artery is likely influenced by body size. In a study of American men and women, the mean radial artery diameter was 3.57 ± 0.28 mm for men and 3.18 ± 0.21 mm for women (24). At the current time, certain procedures require large caliber guiding catheters such as dual-stent strategies and large diameter rotational atherectomy. Guiding catheters larger than 6 Fr in women and 7 Fr in men may be beyond the acceptable caliber of most radial arteries.
ANTICOAGULATION
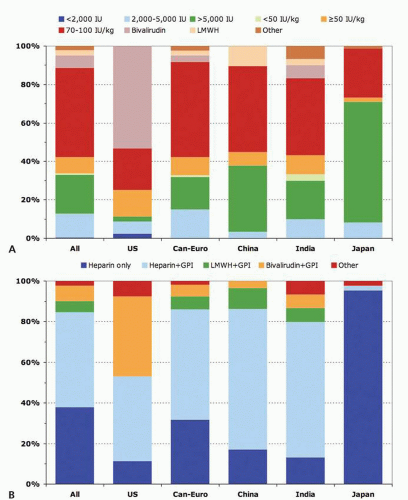
There is great variation in anticoagulation regimens among TR operators across the world, reflecting local practices. For elective and urgent PCI procedures, US operators utilize a heparin-based strategy at nearly similar rate as bivalirudin. In contrast, outside the United States, the majority of PCI procedures are performed with heparin (25) (Fig. 28-5). It is important to note that choice of access site does not eliminate all sources of bleeding.
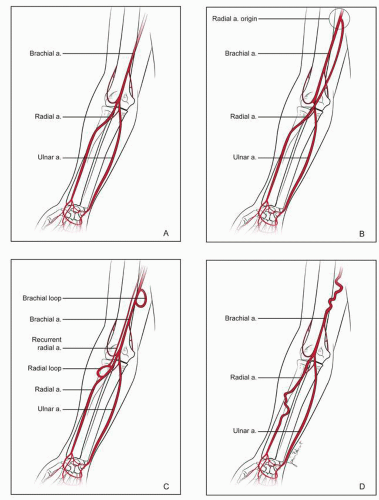 FIGURE 28-2 Common anatomical variations of upper extremity arterial circulation. A: Normal anatomy. B: High bifurcation of the radial artery. C: Arterial loops. D: Tortuosity. |
GUIDING CATHETER SELECTION
Use of the left radial approach affords the ability to utilize similar catheters as when using the femoral approach. Because of the angle of insertion of the brachiocephalic artery into the ascending aorta, optimal guiding catheter selection may differ from the femoral approach when using the right arm. Support is generated from a combination of intrinsic guide stiffness, guide size, and apposition to the opposite wall of the aorta. It is this last feature that is altered when approaching the coronary arteries from the right radial approach. For left coronary interventions, back-up catheters such as the XB series (Cordis Corporation, Bridgewater, NJ) and EBU series (Medtronic, Minneapolis, MN) are the most commonly used guiding catheters for TR-PCI (25). Other options include the Amplatz left (1.0), Ikari (Terumo Medical Corporation, Somerset, NJ), and the Judkins left. For native RCA interventions, a Judkins 4 is the most common guiding catheter (25). Alternatives include Amplatz left (0.75), Amplatz right, or a multipurpose shape (Fig. 28-6).
BYPASS GRAFT INTERVENTIONS
When using the left radial approach, operators can select guiding catheters that are utilized when using the femoral approach. With right radial access, some challenges exist. Primarily, for grafts where the aortic anastomosis is located on the left side of the aorta, an Amplatz left, multipurpose, or hockey stick guiding catheter will often engage the ostium and offer adequate support. For grafts that insert relatively high in the ascending aorta, engagement with
any catheter will be extremely challenging, if not impossible. This is related to the proximity of the graft and the insertion of the brachiocephalic. For typical right-sided grafts, a multipurpose, JR4 or Amplatz left guiding catheter provides for stable working platforms.
any catheter will be extremely challenging, if not impossible. This is related to the proximity of the graft and the insertion of the brachiocephalic. For typical right-sided grafts, a multipurpose, JR4 or Amplatz left guiding catheter provides for stable working platforms.
TABLE 28-1 Relative Contraindications for Transradial PCI Stratified by Operator Experience | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
“UNIVERSAL” GUIDING CATHETER
There are several catheters that are able to engage both the right and the left main coronary ostia and can thus serve as a “universal” guiding catheter. With respect to PCI, “universal” guiding catheters are most commonly employed during STEMI cases where time pressures are present. Examples of “universal” TR guiding catheters include Kimny (Boston Scientific, Natick, MA), Jacky (Terumo Medical Corporation, Somerset, NJ), Amplatz left, and the Ikari Left (Terumo Medical Corporation, Somerset, NJ).
SHEATHLESS APPROACH
The relatively smaller diameter of the radial artery as compared with the femoral artery is an important limitation of the radial approach. Certain niche cases require 7- or 8-Fr guiding catheters. While some gender and geographic differences exist (20, 24), a high percentage of individuals do not have sufficiently large radial arteries to accommodate this range of catheters (Fig. 28-4). Eliminating the access sheath and using a “sheathless approach” may facilitate the use of larger guiding catheters (Fig. 28-7). Unfortunately, there are no commercially available “sheathless”
guides in the United States. Several groups have published data on modifications to current equipment to allow sheathless delivery (30, 31 and 32).
guides in the United States. Several groups have published data on modifications to current equipment to allow sheathless delivery (30, 31 and 32).
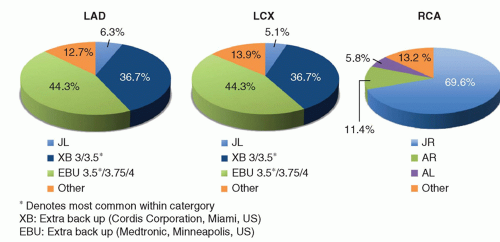 FIGURE 28-6 Commonly used guiding catheters for TR-PCI. (Adapted from J Am Coll Cardiol Intv 2010;3:1022-1031.) |
SPECIAL TOPICS/ISSUES