■ Details of prior upper and lower gastrointestinal (GI) bleed, findings of upper GI endoscopy to exclude other causes of nonvariceal upper GI bleeding, history of prior endoscopic management of bleeding varices, and frequency of paracentesis or thoracentesis should be obtained. Specific attention should be paid to the history of recent changes in mentation or memory loss indicating encephalopathy.
■ Patients with the preexisting encephalopathy and bleeding gastric varices should be evaluated for balloon-occluded retrograde transvenous obliteration (BRTO) of gastric varices because TIPS can worsen encephalopathy.
■ History of hepatobiliary disease and prior biliary and GI surgery should be documented. Prior surgeries may alter anatomy and can increase the complexity of TIPS placement.
■ History of prior liver resection or liver transplantation and the details of altered anatomy from these surgeries including the type of venous anastomosis must be obtained. Prior liver resection or transplantation is not a contraindication for TIPS. However, knowledge of altered portal and hepatic venous anatomy is essential for proper procedure planning.
■ History pertaining to heart disease, deep vein thrombosis, prior pulmonary embolism and pulmonary hypertension require additional preprocedural cardiac workup because pulmonary hypertension and right heart failure are contraindications to TIPS.
■ History of prior pancreatitis with splenic vein thrombosis may result in focal left upper quadrant portal hypertension and gastric varices. TIPS is not indicated for isolated gastric varices from splenic vein occlusion. Transhepatic recanalization of the splenic vein, BRTO, partial splenic arterial embolization, or splenectomy should be considered to treat this condition.
■ Focal physical examination is performed with special emphasis on assessing the patient’s nutritional status, jaundice, lower extremity edema, splenomegaly, ascites, hydrothorax, and encephalopathy.
■ Detailed and extensive discussion of the risks and benefits of the procedure (in particular encephalopathy) should be carried out with the patient and the family.
IMAGING AND OTHER DIAGNOSTIC STUDIES
■ Complete blood count (CBC), comprehensive metabolic panel, and coagulation profile are essential to evaluate the need for correction of thrombocytopenia or coagulopathy and to evaluate the severity of liver disease.
■ A Model for End-Stage Liver Disease (MELD) score that does not include additional points for cause of liver disease is widely accepted to predict survival following TIPS placement.3 A MELD score of greater than 18 is associated with significantly higher mortality rate at 3 months following TIPS.1
■ Preprocedural imaging of the liver and the portal venous system with ultrasound or other imaging modalities such as computed tomography (CT) and magnetic resonance imaging (MRI) to document patency of the hepatic veins, portal vein, and intrahepatic portal branches should be performed. Chronic occlusion of the portal vein is a relative contraindication of TIPS placement. Contrast-enhanced CT or MRI scans of the liver and portal venous system allow greater understanding of the spatial relationship between the hepatic veins and intrahepatic portal venous branches and should be considered for planned TIPS creation. Cross-sectional imaging with CT and MRI are especially helpful for planned TIPS in patients with prior liver resections.
■ In patients with history of long-term central venous access catheters, ultrasound examination of the internal and external jugular veins bilaterally should be considered.
■ Electrocardiogram (EKG) and surface echocardiography should be performed to assess cardiac function and right heart pressures if there is any suspicion of associated heart disease on history and physical examination.
■ Preprocedure liver biopsy is not essential before TIPS placement. However, if prior liver biopsy is available, it may be useful to differentiate presinusoidal and postsinusoidal causes of liver disease.
■ Evaluation of ascitic fluid should be performed in patients with clinical suspicion of spontaneous bacterial peritonitis.
■ TIPS is contraindicated in the presence of significant intrahepatic biliary dilation. However, TIPS can be performed safely following decompression of the bile ducts.
■ Patients with hepatitis C liver disease should be tested for α-fetoprotein elevation, and if elevated, should have cross-sectional imaging when feasible to rule out intrahepatic tumors.
■ It is common practice to type and crossmatch for blood products prior to TIPS.
SURGICAL MANAGEMENT
Preoperative Planning
■ Risks and benefits of TIPS placement are thoroughly discussed with the patient and family, and informed consent is obtained in the clinic setting. For emergent procedures, the family should be made aware of the morbidity, mortality, and risk of encephalopathy associated with the procedure.
■ Laboratory data and all previous imaging studies should be reviewed to access the extent of liver, renal, and cardiac disease present; to document patency of the portal venous system; and to identify altered anatomy from prior surgeries.
■ Preexisting thrombocytopenia and coagulopathy should be corrected. Blood products should be made available at the blood bank.
■ Patients with active upper GI variceal bleeding should have Blakemore tubes placed for balloon tamponade of varices before transfer to interventional radiology. TIPS can be performed while the esophageal and gastric balloons are inflated. However, the authors recommend deflation of balloons during post-TIPS placement splenoportogram to assess variceal filling and the need for embolization of varices.
■ Thoracentesis and paracentesis followed by recommended albumin infusion is performed the evening prior to the procedure in elective cases.
■ Preprocedural prophylactic broad-spectrum antibiotics are recommended.
Positioning
■ Patient is placed supine on the angiographic table.
■ Preliminary ultrasound examination of the internal and external jugular veins should be performed bilaterally.
■ Following the initiation of conscious sedation or induction of general anesthesia, the planned jugular venous access site is prepped and draped in sterile fashion. Prepping the right upper quadrant (RUQ) and lower abdomen is recommended if paracentesis or transhepatic portal vein access for guidance is anticipated.
■ Paracentesis or thoracentesis should be performed first if there is significant ascites or hydrothorax. Significant ascites reduces fluoroscopic visibility during the procedure and at the same time increases the radiation dose to the patient. Displacement of the liver due to hydrothorax or massive ascites may also result in unfavorable anatomy for portal vein access.
■ An arterial line for continuous pressure monitoring during the procedure is indicated following large volume paracentesis in patients with active GI bleeding or hemodynamic instability.
TECHNIQUES
VENOUS ACCESS
■ TIPS is most commonly performed through right internal jugular vein access. Using standard Seldinger technique, access to the right internal jugular vein is obtained with ultrasound guidance. Over a guidewire, the access is dilated and a 10-Fr dedicated vascular sheath is placed into the inferior vena cava (IVC).
■ Some practitioners prefer the use of the left internal jugular vein, as it may provide more stable access to the right hepatic vein. Alternatively, the right and left external jugular veins can be used.
■ In cases of superior vena cava (SVC) obstruction, right and left common femoral venous access can be used for recanalization of the SVC to facilitate more standard venous access from above. Common femoral access can also be used directly for TIPS creation in extreme situations.
■ Care is taken with guidewires, dilators, and sheaths to prevent cardiac dysrhythmias and right atrial perforation while crossing the right atrium.
■ Right atrial and IVC pressures are not routinely obtained unless there is a clinical reason such as history of cardiac or pulmonary disease.
HEPATIC VEIN SELECTION
■ Selection of an appropriate vein of suitable diameter is important. TIPS creation through the right hepatic vein is most common. A standard nonglide, 5-Fr appropriately shaped catheter (based on prior imaging) is then advanced through the sheath into the mid-IVC. As the catheter is withdrawn, the hepatic vein is cannulated.
■ When the right hepatic vein is considered not suitable due to smaller caliber or other anatomic reason, TIPS can be performed through the middle or even left hepatic veins.
■ It can be difficult to distinguish between the right and middle hepatic veins (MHVs), but it is important to do so. When a wedged hepatic venogram is performed in a steep right anterior oblique (RAO) projection (see Visualization of the Portal Venous System), the right hepatic vein will be posterior and the MHV will be anterior to the right branch of portal vein (FIG 1).

VISUALIZATION OF THE PORTAL VENOUS SYSTEM
■ Indirect visualization of the intrahepatic and extrahepatic portal veins during the TIPS procedure can dramatically decrease procedure time. This can be done in multiple ways.
■ Most commonly, wedged portography using contrast or carbon dioxide (CO2) gas is performed (FIG 2A). CO2 gas is an excellent agent for imaging of the hepatic veins, portal veins, and varices because CO2 can easily flow through the venules and sinusoids due to its low viscosity. CO2 is the contrast agent of choice for wedged hepatic venography and in patients with associated renal impairment. However, use of CO2 is contraindicated in patients with right-to-left intracardiac shunting and should be used with caution in patients with hepatopulmonary syndrome.

■ The right hepatic vein catheter is wedged into a central hepatic venule. Wedge hepatic venogram and indirect portogram is then performed with injection of CO2 gas or contrast. CO2 or contrast will flow through the sinusoids to the portal side resulting in filling of the main portal vein and its branches. Peripheral wedging should be avoided to prevent extravasation and even capsular perforation. Imaging should be performed in both anteroposterior (AP) and steep RAO projections to properly assess the anatomic relation of the hepatic vein and the right branch of the portal vein (FIG 1).
■ Similarly, the intrahepatic portal branches can also be visualized using an occlusion balloon catheter. In this method, the 5-Fr catheter is exchanged over a guidewire for an occlusion balloon catheter. The balloon catheter is inflated in a branch of the hepatic vein and not wedged. The balloon is inflated to obstruct venous outflow from the segment. The injection pressure of CO2 is dissipated in a larger segment of liver minimizing complications and with better filling of the portal branches and the main portal vein.
■ Occasionally, wedge portography may fail to visualize portal vein especially in patients with veno-occlusive disease and intrahepatic portal vein branch thrombosis.
■ When indirect visualization of the portal vein is unsuccessful, direct visualization can be attempted (see “The Difficult Transjugular Intrahepatic Portosystemic Shunt ”).
■ Under ultrasound guidance, a 22-gauge needle can be inserted percutaneously into the intrahepatic portal venous system for injection of contrast or CO2. This method will require embolization of the parenchyma traversed during portal vein access at the end of the procedure with Gelfoam or coils to ensure hemostasis.
■ Other methods include percutaneous cannulation of a paraumbilical vein or trans-splenic access to the portal vein, both of which also require embolization of the access tract at the conclusion of the procedure.
PORTAL VEIN ACCESS
■ A number of commercially available device sets are available for TIPS placement. The most important component of the set is a directional needle with a 30-degree angulated tip and an external marker to show the direction of the tip of the needle developed by Colapinto. Several modifications have been made to this original set, and the commonly used modified set is the Rösch-Uchida set (Cook Medical, Bloomington, IN) and is shown in FIG 2B. This set is designed to be more flexible with a needle tip of smaller caliber to minimize trauma to liver. The original Colapinto needle (Cook Medical, Bloomington, IN) is modified to an angulated blunt end cannula covered with a sheath and is used to direct a smaller Rösch-Uchida trocar needle-catheter combination for portal vein access.
■ The Colapinto cannula is advanced through the sheath and into the right hepatic vein over a guidewire. The outer sheath and directable cannula are slowly retracted to within 2 cm from the IVC while rotating the tip in the direction of portal vein.
■ The cannula is rotated anteromedially from the right hepatic vein, aiming for the right portal vein as seen on portography (typically seen at the level of the 11th rib approximately 0.5 to 1.5 vertebral body widths from the spine). The trocar needle-catheter combination is then advanced through the cannula and into the expected location of the right portal vein. The depth of the pass is most commonly 5 cm or less. After removal of the trocar, aspiration of the catheter is performed as it is gradually withdrawn back toward the right hepatic vein. When blood is aspirated, contrast is injected to confirm portal vein access and to assess the suitability of the accessed portal branch for TIPS creation (FIG 2C).
■ Access into the right branch of the portal vein within 2 to 3 cm from the portal vein bifurcation is desired. The portal vein bifurcation is extrahepatic in up to 50% of patients and puncture in this area may lead to exsanguination. Punctures that are too peripheral in the right portal vein are also not optimal because they result in turbulent flow in the TIPS from undesirable angulation.
■ The right branch of the portal vein is posterior in relation to the MHV, necessitating posterior rotation of the cannula for portal vein access. MHV to left portal vein access may need anteromedial rotation of the cannula. It is extremely important to assess the spatial relationship of the chosen hepatic vein and the portal anatomy visualized on portogram to guide the needle pass.
■ Following confirmation of proper access into the portal venous system, a hydrophilic guidewire is advanced into the superior mesenteric or splenic vein. The catheter is exchanged for a multi–side-hole marking catheter over the guidewire (FIG 2D).
■ The 10-Fr sheath is then withdrawn to the right atrium. Dual pressure measurements are obtained in the portal venous system and the right atrium. The difference between the measurements is the portosystemic pressure gradient.
■ A portosystemic gradient (PSG) of 5 to 7 mm is normal and a PSG of greater than 12 mmHg is abnormal. Note that the measured PSG could be lower in the setting of partial portal decompression from extensive portosystemic collaterals such as spontaneous splenorenal shunt. PSGs are also low when the right atrial pressure is transiently elevated from resuscitative measures with intravenous (IV) fluids and blood products, but the absolute portal pressure may remain high from portal hypertension.
■ Direct splenoportography is then performed in AP and oblique projections with iodinated contrast to delineate the portal anatomy, evaluate the presence of competitive shunts and varices as well as to determine the hepatic parenchymal tract length (FIG 2D).
■ In cases of hepatofugal flow, additional venography is performed through the sheath placed within the parenchymal tract to get an accurate measurement of tract length.
■ If the IVC/hepatic vein confluence cannot be clearly visualized during portography, direct contrast injection in that region should be performed to localize the hepatocaval junction for accurate measurement of tract length.
DILATION OF THE TRACT
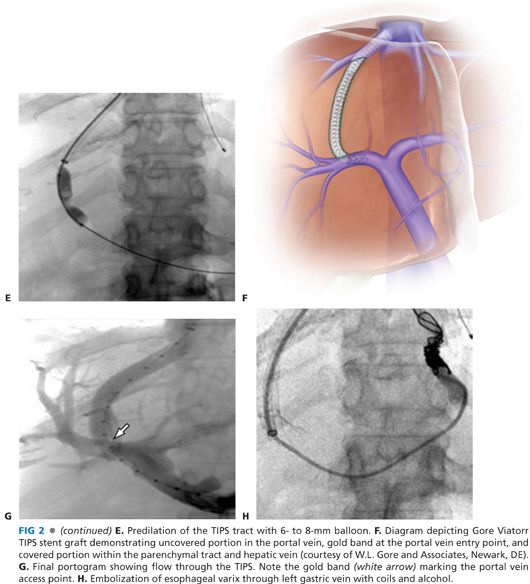
■ A 180-cm long Amplatz Super Stiff guidewire (Boston Scientific, Natick, MA) is then advanced into the splenic vein and the marker pigtail catheter is removed. The 10-Fr sheath dilator is replaced into the sheath and both the sheath and dilator are advanced over the stiff wire and into the portal vein. When the liver is sclerotic and hard, some operators prefer to predilate the hepatic parenchymal tract with a 6- to 8-mm balloon to facilitate advancement of the sheath through the parenchymal tract (FIG 2E).
STENT SELECTION
■ Historically, TIPS was performed with no stent placement within the hepatic parenchymal tract. Tracts were created using only balloon dilation, but patency rates were poor.4 With the development of bare metal stents, long-term patency rates improved to the point that TIPS could be considered a viable alternative to surgical portal decompression. Patency rates improved further with the introduction of polytetrafluoroethylene (PTFE)-covered stent grafts.
■ The most commonly used stent for TIPS placement is the Gore Viatorr PTFE-covered stent graft. The stent is covered with PTFE graft material except for the caudal most 2 cm. The junction between the PTFE covered portion and the bare metal portion is marked with a gold band. The bare stent portion should be placed within the portal vein to allow uninterrupted flow through the interstices and the covered portion is meant to extend through the parenchymal tract and back to the hepatic vein/IVC confluence (FIG 2F). The graft material limits the permeability of bile and mucin into the tract and also eliminates intrastent tissue growth, leading to improved patency rates.5
■ There is still a role for placement of self-expanding bare metal stents, particularly in patients in whom early transplant is expected, when there is single hepatic venous outflow, or when there is concomitant spontaneous bacterial peritonitis.
■ Even though TIPS were created with balloon expandable bare metal stents in the past, their role is currently limited to pediatric TIPS creation to preserve the ability to increase shunt diameter with the growth of the child.6 They can also be used to eliminate kinks during TIPS revision.
■ Typically, a stent diameter of 10 mm is used for all TIPS indications.
■ The stent length is equal to the distance of the hepatic parenchymal tract plus the distance of the hepatic outflow vein to the IVC confluence. One centimeter is often added to this number to account for the loss of length that occurs when a stent is deployed in a curved tract and to compensate for minimal foreshortening during deployment.
STENT PLACEMENT
■ The Gore Viatorr stent graft is advanced through the sheath and into the portal vein. The sheath is then withdrawn to expose the uncovered distal 2 cm. The sheath and stent graft are then retracted as a unit until the gold band marking the covered portion of the stent graft is at the edge of parenchymal tract. The gold band should be held exactly at the junction of the portal vein with the parenchymal tract with gentle traction until deployment. With the stent graft held in this position, the sheath is retracted to the right atrium and the release cord is pulled. The stent graft is now deployed. Following deployment, the stent graft shows an hourglass constriction within the parenchymal tract. The stent graft is then expanded completely by dilating with a balloon of the same diameter as the deployed stent graft.
■ In some patients, such as those with preexisting portal vein stenosis or occlusion, it may be necessary to extend the TIPS into the portosplenic confluence, superior mesenteric vein, or splenic vein to allow effective outflow through the TIPS. This should be performed with self-expanding bare metal stents to preserve inflow into the stent from branches. This may complicate liver transplantation and should be discussed with the transplant team.
■ A correctly placed Gore Viatorr stent graft is easily grasped and removed by a transplant surgeon at the time of liver transplant.
■ The multi–side-hole catheter is readvanced into the portal vein in order to calculate the post-TIPS PSG.
■ When bleeding is the indication, the target PSG is less than 12 mmHg. In the setting of ascites or hydrothorax, gradients under 8 mm are recommended by the Society of Interventional Radiology (SIR) and American Association for the Study of Liver Disease guidelines.2 The risk of hepatic encephalopathy increases significantly when the final gradient is below 5 mmHg. It may be difficult to obtain a truly accurate gradient immediately following emergency TIPS procedure due to the hemodynamic shifts and fluid overload from resuscitative efforts.
■ A final portal venogram is then obtained to ensure proper flow into and out of the TIPS (FIG 2G).
ADJUNCT PROCEDURES
■ When TIPS is performed emergently for refractory variceal bleeding, embolization and sclerosis of gastric and esophageal varices with coils, vascular plugs, or liquid embolic agents such as alcohol should be considered (FIG 2H).
THE DIFFICULT TRANSJUGULAR INTRAHEPATIC PORTOSYSTEMIC SHUNT
■ The left hepatic vein is used for creation of TIPS (FIG 3) in only exceptional circumstances such as when right liver lobe resection is planned in the presence of mild portal hypertension.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


