
Exposure of Carotid Artery
■ In the medial aspect of the wound, the lateral border of the internal jugular vein is identified and sharply defined. The vein is retracted posteriorly and the carotid sheath is entered from the lateral posterior margin. Care must be taken to identify the vagus nerve early, as its usual posterior position places it immediately in the field of dissection as the sheath is opened from this approach.
■ The common carotid artery is dissected circumferentially (FIG 3). Only 5 cm of artery needs to be isolated in order to obtain control and perform the anastomosis. The dissection should stay proximal to the carotid bulb, which minimizes risk of cerebral embolization and injury to more proximal nerves.

Bypass
■ Either Dacron or polytetrafluoroethylene (PTFE) can be used as conduits for extrathoracic bypass with no difference in outcomes.2 Autogenous vein grafts should be avoided, however, as their long-term patency is inferior to prosthetic in this location.3 We favor Dacron given the size ranges available and the relative resistance of the graft to kinking over the short distance of the reconstruction.
■ Prior to arterial clamping, systemic anticoagulation is achieved with intravenous heparin administration. The activated clotting time (ACT) should be monitored and additional heparin administered throughout the procedure to maintain adequate anticoagulation.
■ The subclavian anastomosis is performed first. Arterial control (vessel loops or clamps) is obtained and the vessel is opened with a longitudinal arteriotomy. The anastomosis should be fashioned in the position most favorable to the planned graft. The graft is beveled and trimmed so that the graft lies at an approximately 60-degree angle to the artery. A running Prolene suture is used to perform the anastomosis with completion of the back wall first. Once the anastomosis is complete, the graft is clamped and flow restored to the arm by unclamping the subclavian artery. It is useful to flush through the graft to remove any debris prior to opening to the arm. The graft should also be flushed with heparinized saline and clamped near the anastomosis to avoid any thrombosis of the stagnant blood column within the graft. If repairs are needed, control is restored and pledgeted sutures are used to avoid injury to the fragile artery.
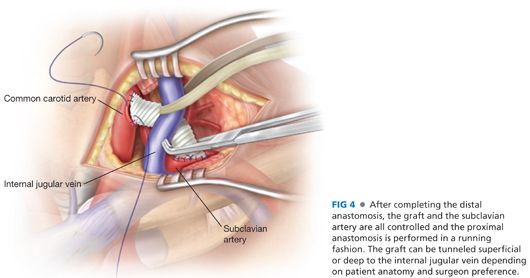
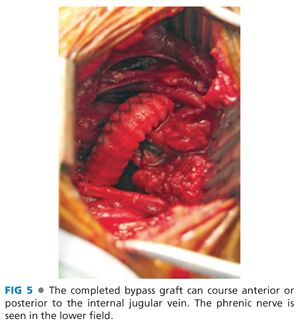
■ The graft is tailored to the appropriate length to prevent redundancy and kinking, and beveled so that the heel of the anastomosis will lie proximally on the carotid artery. As the common carotid artery is clamped, special attention must be directed to neuromonitoring; significantly diminished cerebral perfusion, although very uncommon, mandates shunt placement at this stage of the procedure. A longitudinal arteriotomy is performed and the proximal anastomosis completed with running Prolene suture, again starting with the back wall (FIGS 4 and 5).
■ The final sequence of clamp removal is important to prevent embolism to the brain. Proximal subclavian artery control is again obtained, and the clamp is removed from the graft. The proximal carotid clamp is then removed to allow “flushing” down the arm rather than to the brain. After a few cardiac cycles, the distal carotid clamp is also removed. The proximal subclavian artery is then released as well.
■ When performed in anticipation of thoracic aortic stent grafting, the subclavian artery must be ligated proximal to the origin of the vertebral artery. This can involve dissection deep into the mediastinum and carries an inherent risk of catastrophic bleeding. Alternatively, the proximal subclavian artery can be controlled by placement of an intraarterial occlusion device (e.g., Amplatzer), either during the carotid–subclavian bypass or at the time of subsequent stent graft placement via a left brachial approach.4
Closure
■ If a pneumatic pillow was used to provide exposure, it is deflated prior to wound closure in order to reduce neck extension and assist in allowing the wound to be closed without tension.
■ A closed suction drain is left in the deep wound and brought out through a separate stab incision.
■ In order to provide coverage for the graft, the scalene fat pad is returned to its anatomic location and sutured in place. The SCM is reapproximated with running absorbable sutures.
■ The platysma and subcutaneous tissues are closed in separate layers in a running fashion and the skin is reapproximated with a running dermal suture.
SUBCLAVIAN ARTERY TRANSPOSITION
Exposure
■ The subclavian artery is exposed, as described in the previous section, for carotid–subclavian bypass. The dissection must be carried proximal to the vertebral artery and enough artery must be exposed proximally to allow sufficient length for the anastomosis as well as control the proximal stump. This can often be difficult as an aortic aneurysm can occupy a significant portion of the mediastinum limiting vessel manipulation.
■ The carotid artery is exposed in the same manner as described in the previous section.
Division of the Subclavian Artery
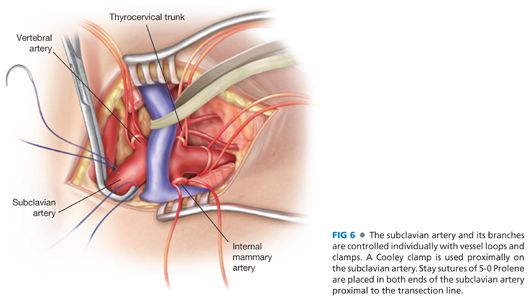
■ Systemic heparin is administered, and maximum arterial length is obtained by advancing a Cooley clamp as deeply as possible into the mediastinum along the subclavian artery. A distal atraumatic clamp is then applied, typically in the midsubclavian artery, with the more proximal branches individually controlled with vessel loops. There must be adequate distance between the proximal clamp and the vertebral artery to allow for proximal control, transposition, and anastomosis. Prior to transection, pledgeted 5-0 Prolene stay sutures are placed on each side of the proximal artery to ensure that if clamp control is lost for any reason, the open artery does not retract into the mediastinum (FIG 6).
■ The proximal subclavian artery is oversewn by extending the stay sutures across the stump. Hemostasis is confirmed by slowly releasing clamp control while maintaining traction on the stay sutures. Only once hemostasis is rigorously ensured are the sutures divided and the proximal subclavian artery allowed to retract into the mediastinum.
Carotid–Subclavian Anastomosis
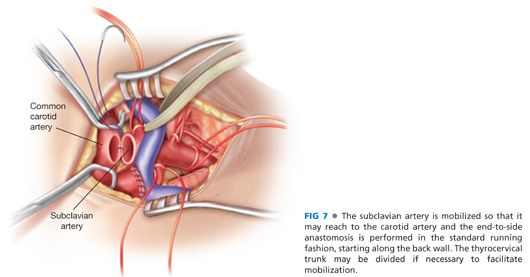
■ The subclavian artery, having been freed circumferentially, is then mobilized toward the carotid artery. It may be tunneled anterior or posterior to the internal jugular vein depending on the length of the artery and patient-specific anatomy. The carotid artery is then clamped proximally and distally and the anastomosis performed in the standard running fashion. Prior control of the subclavian artery is maintained (FIG 7). As the anastomosis is completed, the unclamping sequence should be repeated as described in the preceding section to prevent inadvertent air or particulate embolization to the brain.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


