Transesophageal Echocardiography
Christian Gring
Brian P. Griffin
Overview
Transesophageal echocardiography (TEE) is a diagnostic ultrasound technique in which images of the heart are acquired from the esophagus rather than from the chest wall. The esophageal window has advantages over the transthoracic approach in that higher-resolution images, especially of posterior cardiac structures and the aorta, are possible, and acoustic shadowing from prosthetic material is less. TEE requires passage of the esophageal probe into the esophagus and stomach by using conscious sedation, and it has a finite if low risk of serious complications. It is usually performed when transthoracic echocardiography (TTE) has failed to resolve an important diagnostic question adequately. Standard planes in which to image the heart from the esophagus and stomach have been described. Multiplane transducers for adult and pediatric use with full Doppler capabilities are now widely available. TEE is frequently indicated for the evaluation of a possible cardiac source of embolism, assessment of native and prosthetic valves, endocarditis, evaluation of the left atrium and atrial septum, in disease of the thoracic aorta especially when acute dissection is suspected, and in patients with uninterpretable TTE studies. TEE is useful in the evaluation of patients with hemodynamic compromise in intensive care units, in adult congenital heart disease, in an assessment of the proximal coronary vasculature, and in interventional procedures such as balloon mitral valvuloplasty. Specific areas in which the superiority of TEE over TTE is best established and in which TEE is usually required for a complete evaluation include suspected prosthetic endocarditis, poorly characterized native or prosthetic regurgitation, aortic root abscess and other pyogenic complications of endocarditis, left atrial appendage thrombus, sinus venosus atrial septal defect, aortic dissection, and aortic atheroma.
TEE is an important tool in the evaluation of cardiac structure and function and in assessing the thoracic aorta. TEE images are acquired from an esophageal or gastric imaging window rather than from the chest wall (Table 52.1); thus, TEE usually permits higher-frequency and higher-resolution imaging than TTE. Moreover, the posterior windows avoid air-filled lung tissue and circumvent acoustic shadowing from strong reflectors of ultrasound such as prosthetic valves. Therefore, TEE is particularly powerful in imaging posterior structures such as the atria, the atrial appendages, the interatrial septum, and the aorta.
TEE is invasive and frequently requires local anesthesia and intravenous sedation. It is also more time consuming, more expensive, and less acceptable to patients than TTE. TTE can provide adequate clinical information in many instances and is therefore usually acquired first. TEE is performed if additional information is required or if transthoracic image quality is suboptimal. In most adult echocardiography laboratories, fewer than 10% of all studies are performed by the transesophageal approach (1,2). Major current indications for TEE are shown in Table 52.2.
Anatomic Considerations
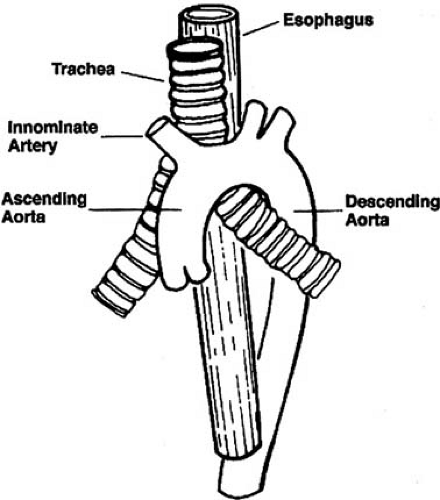
The esophagus is approximately 25 cm in length and extends from the pharynx to the stomach. It descends vertically and slightly to the left, passing behind the trachea, left mainstem bronchus, left atrium, and left ventricle before passing through the diaphragm. The ascending aorta and arch lie anterior to the esophagus (Fig. 52.1). The air-filled trachea and left mainstem bronchus interpose between the esophagus and portion of the ascending aorta and ascending arch, causing a “blind spot”
in imaging the aorta from the transesophageal window. The esophagus twines around the descending aorta, and therefore the transducer must be rotated while imaging the descending aorta to keep the structure in view.
in imaging the aorta from the transesophageal window. The esophagus twines around the descending aorta, and therefore the transducer must be rotated while imaging the descending aorta to keep the structure in view.
TABLE 52.1 Comparison of Transthoracic and Transesophageal Echocardiography | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||
Technology: Transducers and Probes
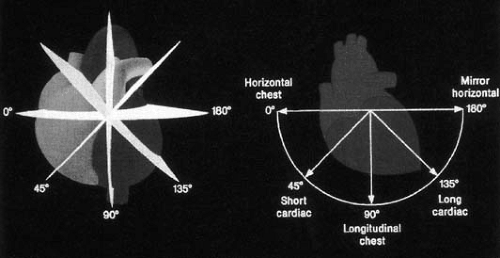
TEE requires the use of a special esophageal probe that interfaces with a conventional cardiac ultrasound system. The esophageal probes currently in use consist of an ultrasound transducer mounted at the end of a 100-cm flexible gastroscope from which the fiberoptic cables and suction capability have been removed. Adult transducers vary in length from 27 to 45 mm, are 14 to 17 mm wide, and are approximately 11 mm thick. The gastroscope cable is approximately 10 mm wide in adult probes, although 7-mm diameter probes are now available and allow imaging even in infants as small as 3 kg (3). Early-generation TEE systems used monoplane or biplane transducers (4,5); current systems, however, use multiplane phased arrays that allow the operator to rotate the transducer around a central axis through 180 degrees (5) (Fig. 52.2). The
horizontal transducer position is by convention at 0 degrees, whereas the longitudinal position is at 90 degrees. These transducers operate at multiple frequencies from 3.5 to 7.0 MHz, and they are capable of performing all Doppler modalities, M-mode, and two-dimensional imaging. Esophageal probes have the standard gastroscope controls that allow anteroflexion and retroflexion of the transducer, as well as side-to-side lateral motion.
horizontal transducer position is by convention at 0 degrees, whereas the longitudinal position is at 90 degrees. These transducers operate at multiple frequencies from 3.5 to 7.0 MHz, and they are capable of performing all Doppler modalities, M-mode, and two-dimensional imaging. Esophageal probes have the standard gastroscope controls that allow anteroflexion and retroflexion of the transducer, as well as side-to-side lateral motion.
TABLE 52.2 Indications for Transesophageal Echocardiography | ||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||
Technique
TEE is performed similarly to upper gastrointestinal endoscopy and requires experience in the safe intubation of the esophagus and stomach. Only operators who have adequate training in esophageal intubation and in echocardiography should perform this procedure.
TABLE 52.3 Transesophageal Echocardiography Procedure | |
|---|---|
|
Patient Selection
Patients should fast for at least 4 hours before the procedure (Table 52.3). A detailed history should be obtained first, with attention paid to a history of dysphagia, esophageal problems, and drug allergies. The esophageal probe is passed blindly in TEE; thus disorders of the esophagus that may interfere with the passage of the probe or that may lead to injury by the probe are considered contraindications (Table 52.4). All oral prostheses and dentures are removed, and intravenous access is acquired. Blood pressure, electrocardiographic monitoring, and oximetry are undertaken throughout the study. Resuscitation equipment, suction, and oxygen should be readily available.
Anesthesia and Sedation
Pharyngeal anesthesia helps to reduce gagging on probe insertion. The pharynx is sprayed with lidocaine (Xylocaine) 4% or 10% Cetacaine. The patient may also gargle viscous lidocaine 2% for additional anesthetic effect. The effects of anesthesia are apparent within a few minutes and persist for 30 to 45 minutes after the procedure. Patients should not eat or drink during this period because of the risk of aspiration. At the Cleveland Clinic in Cleveland, Ohio, we use both fentanyl and a benzodiazepine (midazolam) for sedation, starting with 12.5 to 25 μg of fentanyl and 0.5 to 1.0 mg of midazolam. The sedation is titrated as necessary while one monitors the effects on heart rate, blood pressure, and oximetry. Sedation can lead
to respiratory depression or hypotension; thus, specific antagonists (e.g., flumazenil, naloxone) should be available for use if indicated. Additional sedation may be required throughout the procedure to maintain patient comfort. Ambulatory patients should be accompanied, to prevent their driving home under the influence of sedative and narcotic drugs.
to respiratory depression or hypotension; thus, specific antagonists (e.g., flumazenil, naloxone) should be available for use if indicated. Additional sedation may be required throughout the procedure to maintain patient comfort. Ambulatory patients should be accompanied, to prevent their driving home under the influence of sedative and narcotic drugs.
TABLE 52.4 Contraindications to Transesophageal Echocardiography | |
|---|---|
|
Need for Antibiotic Prophylaxis
Many patients undergoing TEE have valvular or other lesions that pose a risk for endocarditis, and case reports have suggested that TEE was a causative factor in the development of endocarditis (6). However, several studies involving a total of 522 patients failed to detect significant bacteremia of oral flora associated with the TEE procedure or of clinical infection at follow-up (7,8,9). Therefore, the risk of endocarditis with TEE in experienced hands seems low, and routine prophylaxis is not indicated. Antibiotic coverage may be considered if the intubation is unexpectedly difficult or traumatic.
Probe Insertion
After the patient assumes a left lateral decubitus position with the neck flexed, the probe is guided into the upper esophagus. As the patient swallows, the probe is gently but firmly advanced into the distal esophagus. A bite block is inserted between the teeth to protect the probe. In ventilated patients, probe insertion is performed with the patient supine, while flexing the neck and manually retracting the tongue and anterior pharyngeal wall in an anterior direction. The probe should never be forcibly advanced because this risks causing an esophageal tear. If the probe does not pass smoothly, assistance from an endoscopist should be sought. At the end of the procedure, the patient should be monitored until vital signs have returned to baseline or at least normal values and the sedation has begun to wear off. The probe is washed and then sterilized by immersion in an antimicrobial solution (glutaral [Cidex]) for 20 minutes. The probe is rinsed and is allowed to air dry.
Safety and Complications
Although TEE is invasive and is often performed in critically ill patients, successful intubation is possible in more than 98% of appropriately selected patients, and complications are uncommon (1,2). Inability to pass the probe is most often the result of operator inexperience, patient noncompliance, or, rarely, pathologic lesions in the esophagus. Once successful probe passage has occurred, early cessation of the procedure occurs in less than 1% of cases. The most common reason is patient intolerance of the probe, rather than the onset of a complication (1).
Major Complications
Major complications such as death, esophageal perforation, serious arrhythmia, congestive heart failure, and laryngospasm are uncommon and occur in less than 0.3% of patients (1). One death was reported out of 3,827 consecutive patients examined in one series. This was caused by arrhythmia following the procedure in a patient with autopsy-proven myocarditis (2). Another death was reported in a series of 10,419 patients and was the result of esophageal perforation in a patient with an unsuspected esophageal neoplasm (1). A third death following TEE was reported in a patient with acute aortic dissection in whom aortic rupture occurred during a bout of severe retching and nausea after probe insertion (10). Although serious esophageal injuries including perforation and tears have been reported (11), they are very rare. Laryngospasm and severe bronchospasm occasionally occur because of aspiration of anesthetic agents or lubricants used for probe insertion and rarely from inadvertent passage of the probe into the airway (12).
Minor Complications
Minor complications such as transient hypoxia, hypotension, hypertension, angina, bronchospasm, atrioventricular block, supraventricular tachycardia, and nonsustained ventricular arrhythmia occur in less than 3% of cases (2). Transient vocal cord paralysis (13), compression of anomalous vascular structures by the esophageal probe (14), and adverse reactions to the drugs used in patient preparation occur but are uncommon. The most common adverse medication reaction is methemoglobinemia in susceptible subjects receiving topical anesthesia (15). Sore throat and mild dysphagia are common following the procedure but rarely are prolonged for more than 24 hours.
Imaging Planes
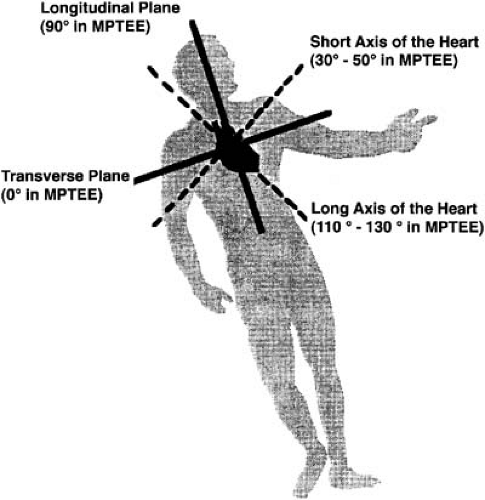
TEE can be challenging, because the esophagus is not usually precisely aligned with the true long and short axis of the heart (Fig. 52.3). Furthermore, the relationship between the esophagus and cardiac structures is variable. Nevertheless, standard imaging planes have been described for TEE, which are greatly facilitated by multiplane technology and endoscope manipulation. The transesophageal examination is usually goal oriented, but it still is important to examine systematically all major cardiac structures and the aorta, so a complete examination is always performed.
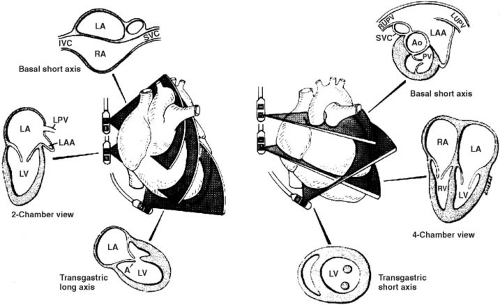
Base of the Heart
At about 30 cm from the incisors, the probe lies behind the left atrium and the base of the heart. In the transverse plane (0 degrees) at this level, the aortic valve is seen in cross section, with portions of the left and right atrium and interatrial septum (Fig. 52.4). Withdrawing the probe slightly from this view allows imaging of the left atrial appendage, the superior vena cava, the right ventricular outflow tract, the ostia of the coronary vessels, the main pulmonary artery to its bifurcation, and a portion of the right pulmonary artery. The proximal
portion of the ascending aorta is imaged in this view, but it and the distal portions of the left pulmonary artery are difficult to image because of the interposition of air-filled large airways.
portion of the ascending aorta is imaged in this view, but it and the distal portions of the left pulmonary artery are difficult to image because of the interposition of air-filled large airways.
The longitudinal imaging plane (90 degrees) at this level provides important images of the great vessels, interatrial septum, left atrial appendage, and pulmonary veins. When the transducer is rotated to the left, a two-chamber view of the left atrium and left ventricle is seen. The left atrial appendage and the left pulmonary veins are often most easily imaged in this view. The mitral valve is also clearly seen in this view, and mitral regurgitation may be sought here. With clockwise rotation of the probe, the right ventricular outflow tract, pulmonary valve, and main pulmonary artery may be imaged. With additional clockwise rotation, the aortic valve and ascending aorta are seen. This view is important in the evaluation of the ascending aorta, particularly with regard to aortic dissection and in assessing aortic regurgitation. Finally, with further clockwise rotation, the right atrium, interatrial septum, and superior vena cava may be imaged. This plane is important in the detection of a communication at the atrial level and in assessing disorders of the superior vena cava. Multiplane imaging is especially useful at this level in allowing the true long and short axis of the aortic valve and ascending aorta to be obtained. Typically, the true short axis is seen at approximately 30 to 60 degrees and the true long axis at 120 to 150 degrees (Fig. 52.5).
Midesophageal Views
By advancing the probe into the midesophagus beyond the base of the heart, portions of both atria and ventricles, the interventricular septum, and the mitral and tricuspid valves are seen in the transverse imaging plane (see Fig. 52.4). A four-chamber view is acquired at this level by flexing the probe
posteriorly. This view is similar to the apical four-chamber view acquired transthoracically, except the imaging plane does not cut through the true apex. This represents an inherent limitation of transesophageal imaging in the acquisition of ventricular volumes and in the detection of apical thrombus. This imaging plane is helpful in detecting regurgitation at the mitral and tricuspid valves and in global assessment of ventricular function. With slight counterclockwise rotation of the transducer, the left ventricular outflow tract and the proximal ascending aorta are seen. Longitudinal imaging at this level produces a two-chamber image of the heart already described. Multiplane images at this level are useful in distinguishing the individual leaflets of the mitral valve and the scallops of the posterior leaflet and in detecting eccentric jets of mitral regurgitation. Optimal differentiation between anterior and posterior mitral leaflet disorders is at about 140 degrees, whereas the full extent of the mitral closure line, from medial to lateral commissure, is at about 50 degrees.
posteriorly. This view is similar to the apical four-chamber view acquired transthoracically, except the imaging plane does not cut through the true apex. This represents an inherent limitation of transesophageal imaging in the acquisition of ventricular volumes and in the detection of apical thrombus. This imaging plane is helpful in detecting regurgitation at the mitral and tricuspid valves and in global assessment of ventricular function. With slight counterclockwise rotation of the transducer, the left ventricular outflow tract and the proximal ascending aorta are seen. Longitudinal imaging at this level produces a two-chamber image of the heart already described. Multiplane images at this level are useful in distinguishing the individual leaflets of the mitral valve and the scallops of the posterior leaflet and in detecting eccentric jets of mitral regurgitation. Optimal differentiation between anterior and posterior mitral leaflet disorders is at about 140 degrees, whereas the full extent of the mitral closure line, from medial to lateral commissure, is at about 50 degrees.
Transgastric Views
To obtain this series of views, the probe is advanced into the stomach. Generally, the tip of the probe must be flexed to bring the transducer in contact with the mucosa of the gastric fundus. In the transverse plane, a short-axis view of the left and right ventricle is acquired (see Fig. 52.4). This view allows an assessment of regional and global left ventricular function. The mitral valve apparatus and leaflets are also well seen in this view. A longitudinal view at this level allows the mitral valve and the left ventricle to be imaged in long axis. The anterior and inferior walls are clearly seen, as are the papillary muscles and chordae. The true apex of the heart is most likely to be displayed in this view. Rotation of the probe in the long axis frequently allows the left ventricular outflow tract to be aligned with the Doppler cursor so a Doppler evaluation of the aortic valve and left ventricular outflow tract may be performed. Further rotation allows examination of the right ventricle and outflow tract. Another series of images is frequently possible by passing the probe further into the stomach and anteflexing (the deep transgastric view). In this view, the transducer is close to the apex, and the images obtained simulate those acquired in a transthoracic five-chamber or subcostal view. This view often optimizes Doppler interrogation of the aortic valve and outflow tract.
Aorta
The aorta may be examined from the ascending aorta to below the diaphragm (Fig. 52.6). The examination of the ascending aorta has already been described. The descending aorta is evaluated by rotating the probe to the left and posteriorly at the midesophageal level. The aorta is seen in cross section using the transverse transducer at this level and in the long axis using the longitudinal transducer. As the probe is withdrawn to approximately 20 to 25 cm, the transverse arch and distal portions of the ascending aorta are seen. The proximal portions of the left subclavian and other head and neck vessels may be imaged with a longitudinal or multiplane transducer.
Indications
Left and Right Atrium
Atrial Thrombus
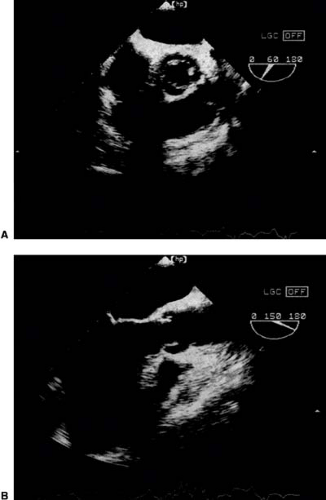
TEE is now the technique of choice for the diagnosis of atrial thrombus (Fig. 52.7) (16,17). The sensitivity and specificity of TEE for the detection of thrombus in both the body and appendage of the left (18,19,20) and right (21) atria are superior to those of TTE and have exceeded 90% in a number of large series with surgical validation (22) as compared with less than 50% for TTE.
Spontaneous Contrast
TEE often identifies spontaneous echo contrast in the left atrium or appendage, especially in patients with atrial fibrillation or atrial thrombus (Fig. 52.8). This feature is reported in as many as 20% of all patients undergoing TEE but is rarely seen by TTE (23). Spontaneous contrast in the left atrium is an independent risk factor for systemic embolization in both mitral stenosis and nonvalvular atrial fibrillation (24,25




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree