Transcervical–Transsternal Maximal Thymectomy for Myasthenia Gravis
Joshua R. Sonett
Alfred Jaretzki III
The combined transcervical–transsternal maximal thymectomy procedure (T-4), employing wide exposure in the neck and mediastinum, routinely and predictably enables maximal removal of thymic tissue within the cervical–mediastinal compartments. Cooper and coauthors1 have labeled this procedure the benchmark against which other resectional procedures should be measured. On the basis of the defined anatomic extent of the thymus and accessory thymic tissue, a comprehensive resection is required, and regardless of innovations in surgical and incisional approaches, removal of the entire thymus remains the goal of thymectomy in the treatment of autoimmune nonthymomatous myasthenia gravis (MG). Accordingly, whether or not the T-4 thymectomy technique is employed in the treatment of nonthymomatous MG, we believe that the details of this resectional technique should be the goal of the thymectomy technique employed regardless of the surgical approach or the incision selected.
Operative Technique
All tissue is resected that anatomically has been shown by Jaretzki and Wolff 3 to contain thymus (e.g., visible thymus, suspected thymus, and anterior cervical–mediastinal fat). The procedure is performed as an en bloc dissection to ensure complete removal of all thymus-containing tissue as well as to avoid the potential seeding of thymus in the wound. A photograph of a typical maximal thymectomy specimen confirms the extent of the “maximal” resection (Fig. 186-1). A video by Jaretzki4 that depicts the operative procedure in detail is available. Regardless of the surgical approach, however, injury to the phrenic, left vagus, and recurrent laryngeal nerves must be avoided, since injury to these nerves can be especially devastating in the myasthenic patient. Accordingly, regardless of the surgical technique selected, we believe that it is far preferable to leave behind potential thymus-bearing tissue than to injure these nerves.
Exposure
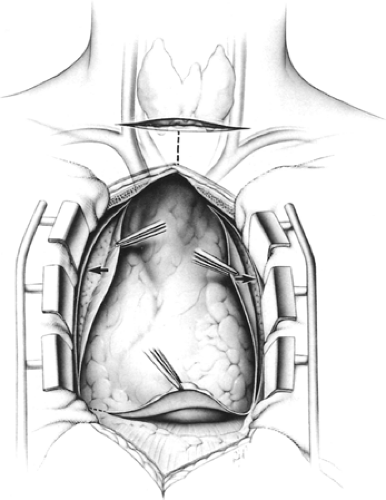
Wide exposure in the neck and mediastinum is obtained, using a cervical incision and a median sternotomy (Fig. 186-2). The skin incisions may be kept separate for cosmetic considerations or may be combined into a T for better exposure; both ways, the cervical and mediastinal surgical fields are confluent (in continuity) below the subcutaneous level. The confluence of the two surgical fields has not been made clear previously. The T incision is recommended for obese patients with short necks, for reoperations, and when large or malignant thymomas are also present.
Initial Neck Incision
A collar incision is created, platysmal flaps are elevated for wide exposure, and the strap muscles are mobilized. The remainder of the neck exploration and dissection is delayed until after the mediastinal dissection is completed.
Mediastinal Incision and Dissection
A vertical skin incision is carried from within 2 to 3 cm of the sternal notch or joined with the low collar incision into a T, as noted previously, and extended caudad to the level of the xyphoid. A median sternotomy is performed.
The retrosternal portions of the strap muscles are then elevated and the lateral portions of the innominate vein and the internal mammary veins are identified by bilaterally sweeping this portion of the thymus medially. Each sternal edge is then elevated, and the fat behind the sternal edges (to be removed with the specimen) is swept away from the incision (laterally) in order to expose the retrosternal portions of the mediastinal pleura.
Starting caudally, the mediastinal pleura, which is now exposed just behind the sternum, is incised bilaterally from the level of the diaphragm to the thoracic inlet (Fig. 186-2, arrows). Superiorly during this maneuver, care must be taken to avoid injury to the phrenic nerve and internal mammary vein, since these structures are anterior at this level and close to the line of this incision. The sternotomy retractor is then inserted.
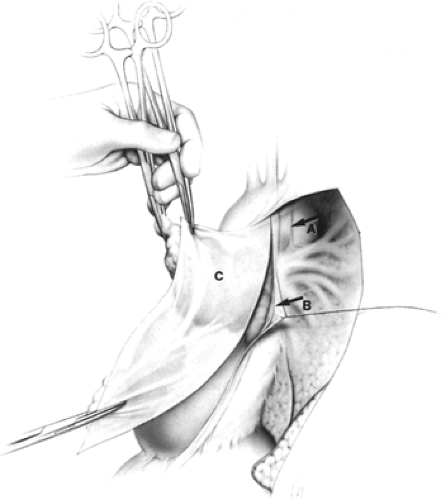
The mediastinal pleura is incised again, this time posteriorly approximately 1 cm anterior and parallel to the phrenic nerves (Fig. 186-3). To facilitate this incision, starting superiorly where the pleural incision is to be made, the mediastinal pleura is first carefully and bluntly separated from the underlying thymus with
closed Metzenbaum scissors at this site. If the thymus is removed and the mediastinal pleural sheets are left in the patient or these sheets are separated from the underlying thymus, microscopic thymus may be left on the mediastinal pleura.
closed Metzenbaum scissors at this site. If the thymus is removed and the mediastinal pleural sheets are left in the patient or these sheets are separated from the underlying thymus, microscopic thymus may be left on the mediastinal pleura.
The mediastinal pleura posterior to this second pleural incision, with the adherent phrenic nerve, is then elevated and teased away from the underlying thymofatty tissue. The artery accompanying the nerve is preserved to avoid devascularization and possible injury to the phrenic nerve. The small phrenic vessel branches are divided using miniclips, not unipolar cautery, to avoid thermal injury to the nerves. During the superior portion of this dissection on the left, the phrenic nerve must be exposed and protected (Fig. 186-3B). The location of the left vagus nerve must also be noted and this nerve also avoided (Fig. 186-3A); it lies 1 to 2 cm posterior to the phrenic nerve and contains the left recurrent laryngeal nerve at this level. Throughout this portion of the dissection, extreme care must be taken to avoid injury to the nerves.
Starting at the level of the diaphragm and using sharp dissection on the pericardium, with division of the “fingers” of pericardium that enter the thymus (Fig. 186-4) (blunt dissection leaves microscopic thymus on the pericardium), an en bloc dissection is undertaken from diaphragm to innominate vein and from hilum to hilum. The fingers of pericardium that enter the thymus must be divided and included in the specimen to remain in the correct plane; this is well demonstrated in the Jaretzki4 operative video. All thymus, suspected thymus, and mediastinal fat, including both mediastinal pleural sheets, are removed en bloc. Included in this portion of the specimen are (a) all encapsulated and unencapsulated thymic lobes without individual identification; (b) the anterior mediastinal and pericardiophrenic fat; (c) the thymofatty tissue behind and beyond the phrenic nerves when present, including tissue lying in the sulcus between the cava and the ascending aorta on the right, tissue behind the innominate vein, and tissue lying in the region of the aortopulmonary window on the left; and (d) the tissue removed from the cervical portion of the dissection as subsequently developed.
The thymus is then separated from the innominate vein by sharp dissection and the thymic veins are divided using clips or ties. The mediastinal dissection above the innominate vein is completed by elevating the strap muscles at this level, sweeping
the thymic lobes medially, and then dissecting them off the lower portion of the innominate artery. At this point, laterally and bilaterally and only at this point, the dissection is adjacent to the capsule of the thymus.
the thymic lobes medially, and then dissecting them off the lower portion of the innominate artery. At this point, laterally and bilaterally and only at this point, the dissection is adjacent to the capsule of the thymus.
Completion of Cervical Dissection
The cervical dissection is then undertaken. This requires experience in neck surgery to avoid injury to the recurrent nerves and preserve the parathyroid glands. The en bloc mobilization cephalad to the innominate artery is resumed, posterior to the strap muscles, medial to the recurrent laryngeal nerves, and anterior to the trachea. The anatomic relationship of the cervical thymus and its variations, the parathyroid glands, and the recurrent laryngeal nerves are illustrated in Figure 186-5.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree