Radiologic Evaluation of Lung Cancer
Patrick J. Fultz
Richard H. Feins
The radiologic evaluation of lung cancer is directed at determining the best means for diagnosing and staging the cancer and the best method of treating patients with this diagnosis. Although both the standard chest radiograph and computed tomography (CT) of the chest are the mainstays of radiologic evaluation, neither, alone or in combination, can make a definitive diagnosis of lung cancer. Such a diagnosis requires cytologic or histologic study. Similarly, except for the size criteria (T), neither study nor the addition of position emission tomography (PET)/CT can very often stage a given lung cancer definitively. Such staging usually requires either direct operative examination or cytologic or histologic proof. Yet all too often patients are told they have lung cancer or are assigned to a specific treatment based on radiologic evidence alone. This has been true even of some large-scale cooperative trials. This leap of faith is not only unfounded but also unnecessary, given today’s variety of minimally invasive diagnostic procedures.
Routine Screening for Lung Cancer
With lung cancer being the most common cause of death by cancer in both men and women and with the belief that the earlier the stage of the tumor, the more curable it is, screening for lung cancer by routine chest radiographs or, more recently, CT, has appeared very attractive. Indeed, several studies have been done to test the hypothesis that routine chest radiographs, especially in a high-risk population, lead to earlier discovery of the disease and more curative treatment. Unfortunately this has not proved to be the case. Studies were done of large numbers of cigarette-smoking men at the Mayo Clinic by Fontana and associates,15 at Memorial–Sloan Kettering Cancer Center by Melamed and colleagues,46 at Johns Hopkins University by Tockman and coworkers,73 and in Czechoslovakia by Kubik and coinvestigators.36 All studies found that although screening did indeed lead to earlier detection of tumors, increased resectability, and improved length of survival, overall mortality was not decreased from that of controls. Salomaa and colleagues59 found only 93 men to have lung cancer out of 33,743 male cigarette smokers screened as part of the Alpha Tocopherol, Beta-Carotene Cancer Prevention Study. Although Strauss69 has argued that the “significant stage distribution, resectability, and long-term survival advantages” in this study prove that chest radiographic screening can save lives, the current American Cancer Society guidelines for cancer screening as reported by Smith and associates67 do not recommend routine screening chest radiographs for lung cancer.
Advances in low-dose spiral CT scanning have led to several studies of the ability of these techniques to detect early tumors. Lung cancers were discovered more frequently with spiral CT than with chest radiographs; the radiographs missed 73% of the lesions. However, only a small number of tumors were discovered in a large number of examinations in the report of Kaneko and associates.33 Similarly, in the baseline screening study of chest radiographs and CTs of Henschke and coworkers,23 the radiographs missed 21 (74%) of the 27 malignancies seen by CT.
Management issues regarding the large number of nodules found by CT in at-risk patients are considerable. In the study by Swensen and associates,71 after a baseline CT and 1 year follow-up CT scan, 2,244 uncalcified nodules were found in 1,000 (66%) of 1,520 study participants. Only 1.7% of patients were proved to have lung cancer. As a result of this and other studies, a set of guidelines for management of pulmonary nodules of various sizes found by CT has been put forth by a group of investigators from the Fleishner Society.39
Studies of the overall effect on mortality are under way, but given the higher cost of spiral CT versus chest radiography, it remains to be seen if this modality will be shown to be an effective screening tool under current circumstances.
Diagnosing Lung Cancer
Although definitive diagnosis of lung cancer requires histologic or cytologic confirmation, several aspects of a given radiographic finding may lead one to be more suspicious of lung cancer. The most important of these is probably the radiographic history of the lesion. Lesions that can be shown on older studies (either chest radiographs or CT) to be completely stable in size and shape are unlikely to be cancerous. A search for prior imaging exams should be one of the first steps toward diagnosis. Most films are destroyed after 7 years, however, which makes it
difficult to confirm stability. It is hoped that digital archiving of radiographic studies will eliminate the need to purge studies and make obtaining them for comparison easier. It should be remembered, however, that a change in a lesion, even after a long period of documented stability, could be an indicator of a scar carcinoma or a particularly slow-growing tumor.
difficult to confirm stability. It is hoped that digital archiving of radiographic studies will eliminate the need to purge studies and make obtaining them for comparison easier. It should be remembered, however, that a change in a lesion, even after a long period of documented stability, could be an indicator of a scar carcinoma or a particularly slow-growing tumor.
Radiographic Features
The radiographic findings caused by carcinoma of the lung may result from the tumor itself, from changes in the pulmonary parenchyma distal to a bronchus obstructed by the tumor (atelectasis, infection, or both), and from spread of the tumor to extrapulmonary intrathoracic sites (e.g., hilar and mediastinal lymph nodes, pleura, chest wall, and other mediastinal structures). The findings vary with location, cell type, and length of time the tumor has been present.
Garland17 estimated that when a lung tumor is first detectable on a chest radiograph, it has completed three-fourths of its natural history. Rigler54 observed that the radiographic abnormality frequently antedates the first symptoms or signs of the disease by ≥7 months. These early features are subtle and often appreciated only in retrospect.
Early Radiographic Features
The early signs visible in radiographs of the chest, as Rigler55 noted, are produced directly by the tumor itself. The smallest single, solitary lesion that can be seen is approximately 7 mm in diameter, although multiple smaller lesions (diffuse lung lesions) may be recognized. The single lesion is frequently not identified until it is ≥10 mm in diameter; a smaller lesion may be obscured by overlying or adjacent structures. Muhm and associates50 studied lung cancer in 92 patients in a chest radiographic lung cancer screening study in which at least two observers initially reviewed all radiographs; they found that 90% of the peripheral lung cancers were visible in retrospect on prior radiographs.
The early signs of a lung tumor are as follows:
A focal opacity within the lung parenchyma
A cavitary mass
A segmental, indistinct, poorly defined opacity
A nodular, streaked, local infiltration along the course of a blood vessel
Segmental consolidation
A roughly triangular lesion arising in the apex and extending toward the hilum
A mediastinal mass (an uncommon early sign)
An enlargement of one hilum
Segmental or lobar obstructive emphysema (a rare finding in carcinoma of the lung)
Segmental atelectasis
The relative incidence of these various early changes are difficult if not impossible to discern, because most patients have more advanced disease when first examined. Weiss and associates,76 however, recorded the incidence of these early features in a screening program to detect lung cancer. A peripheral nodule or mass occurred in 33%, a peripheral “infiltrate” in 25%, and hilar enlargement in 28% of patients who developed a lung cancer. Atelectasis and a pleural effusion each occurred in 3%, and obstructive emphysema was seen in only 1%.
Table 108-1 Chest Radiographic Presentations of Lung Cancer | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Usual Radiographic Manifestations
Byrd and associates6 classified the radiographic features as hilar, pulmonary parenchymal, and intrathoracic extrapulmonary. In their review of the chest radiographs of 600 patients with carcinoma of the lung, a hilar abnormality either alone or associated with other abnormalities was present in 41%. Obstructive pneumonitis, collapse, or consolidation was also present in 41%. A large parenchymal mass was present in 21.7% and a small mass was evident in 20.3%; multiple masses were present in only 1.1%. An apical mass was found in 2.6% of the patients, and in no patient was hypertranslucency seen. The various extrapulmonary intrathoracic manifestations were present in 11%, with mediastinal widening and pleural effusion being more common. Table 108-1 lists the usual radiographic findings. Amemiya and Oho1 (Table 108-2) and Swett and associates71 have noted that a peripheral nodular mass is now the most common radiographic presentation of bronchial carcinoma. Many or most of these are ≤3 cm and fall into the category of solitary pulmonary nodule.
Uncommon Radiographic Manifestations
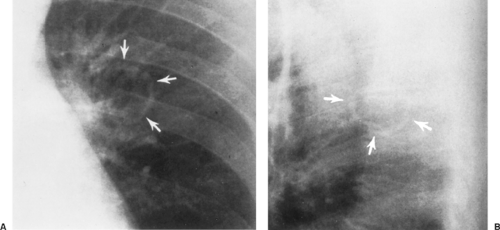
Woodring77 reviewed the uncommon radiologic presentations of lung cancer. The more important of these were (a)
spontaneous regression after initial recognition (extremely rare) or an observed decrease in size of the tumor mass, (b) calcification in psammoma bodies in the tumor or dystrophic calcification in areas of tumor infection or necrosis, and (c) a tumor presenting as a thin-walled cavity (Fig. 108-1). Woodring and Fried79 reported a 6% incidence of primary carcinoma in a series of solitary cavities with a wall thickness of ≤4 mm. Other unusual findings were the radiologic presence of satellite nodules or the occurrence of two separate synchronous primary tumors, one being a possible metastasis of the other, in 1% of the initial radiographs. Other rare findings were the presence of a meniscus or “crescent sign” within the tumor mass and the occurrence of two anatomically separated areas of atelectasis or pulmonary consolidation, which is by far more typical of an inflammatory disease process. Of passing interest is the occurrence of a spontaneous pneumothorax as the initial radiographic feature of a lung cancer. Steinhauslin and Cuttat68 reported this occurrence in 0.46% of lung cancer cases. Although dystrophic calcification is considered uncommon, Mahoney and coworkers41 identified it on CT scans in 13% of lesions that were subsequently proved to be cancer.
spontaneous regression after initial recognition (extremely rare) or an observed decrease in size of the tumor mass, (b) calcification in psammoma bodies in the tumor or dystrophic calcification in areas of tumor infection or necrosis, and (c) a tumor presenting as a thin-walled cavity (Fig. 108-1). Woodring and Fried79 reported a 6% incidence of primary carcinoma in a series of solitary cavities with a wall thickness of ≤4 mm. Other unusual findings were the radiologic presence of satellite nodules or the occurrence of two separate synchronous primary tumors, one being a possible metastasis of the other, in 1% of the initial radiographs. Other rare findings were the presence of a meniscus or “crescent sign” within the tumor mass and the occurrence of two anatomically separated areas of atelectasis or pulmonary consolidation, which is by far more typical of an inflammatory disease process. Of passing interest is the occurrence of a spontaneous pneumothorax as the initial radiographic feature of a lung cancer. Steinhauslin and Cuttat68 reported this occurrence in 0.46% of lung cancer cases. Although dystrophic calcification is considered uncommon, Mahoney and coworkers41 identified it on CT scans in 13% of lesions that were subsequently proved to be cancer.
Table 108-2 Radiographic Findings in 200 Patients with Lung Cancer | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||
Influence of Cell Type
Certain radiographic patterns are characteristic of the various cell types. From the studies of Byrd and associates6 and that of Theros,72 as well as the review by Sider,64 several generalities can be made.
Squamous cell carcinoma most often presents a picture of obstructive pneumonitis, pulmonary collapse, or parenchymal consolidation, because 65% of these tumors occur in a central location in the bronchial tree. A hilar abnormality is often present. Approximately one-third of squamous cell tumors appear as peripheral masses. Many are small lesions (≤3 cm in diameter), but in previous decades, up to two-thirds of the peripheral squamous cell tumors were >4 cm on initial recognition. Cavitation is more common in peripheral squamous cell carcinomas than in other lung carcinomas, occurring in approximately 10% to 20% of patients with these peripheral tumors. Cavitation in this instance results from necrosis in the tumor mass. Cavitation and abscess formation may also occur distal to a bronchus obstructed by tumor. When both types of cavities are combined, they constitute approximately 50% of all lung abscesses seen in patients >50 years of age. In 3% to 4% of patients with squamous cell tumors, the radiograph of the chest may show no abnormality, the tumor being located in a mainstem bronchus and producing no changes in the parenchyma distal to it.
Adenocarcinomas are most often peripheral masses. As with the peripheral squamous cell tumors, a great percentage of these lesions are initially recognized when they are ≤3 cm in diameter. Many still are not discovered, however, until they are >4 cm. Cavitation is rare. These peripheral lesions represent 60% to 70% of all the primary adenocarcinomas of the lung. The lesion most often has a nodular or ill-defined border. A corona radiata, as it was termed by Heitzman and colleagues,22 or sunburst appearance of the border, is often readily appreciated on the standard radiographs and may represent local lymphatic spread. Eccentric calcification may be present within the mass. A hilar abnormality or an obstructive parenchymal lesion is less common than the peripheral mass but appears to be increasing in frequency. Woodring and Stelling80 reported that 28% of adenocarcinomas presented solely as central masses, and 51% of all patients had some degree of central involvement: hilar or mediastinal node adenopathy.
A subtype of adenocarcinoma, bronchioloalveolar carcinoma, may present as a solitary peripheral mass. It represents approximately 35% of all small peripheral masses, a localized area of pneumonic infiltrate that may extend to involve an entire
lobe or even more of the lung, or less commonly as multiple unilateral or bilateral coalescent multinodular infiltrates. In a study of 136 patients with this tumor, Hill26 reported that the presenting radiographic findings were a solitary nodule <4 cm in diameter in 23%, a mass in 20%, a localized area of consolidation (less than one lobe) in 7%, diffuse coalescent consolidation in 23%, and diffuse nodules in 27%. Unlike tumors of other cell types, the presence of air bronchograms in the areas of involvement is common. Less frequently, an interstitial pattern of involvement of the lung is noted, which Berkman3 reported to be the result of secondary lymphatic spread of the tumor. According to Sider,64 pleural effusion may be present in 8% to 10% of patients; rarely, a pneumothorax can occur.
lobe or even more of the lung, or less commonly as multiple unilateral or bilateral coalescent multinodular infiltrates. In a study of 136 patients with this tumor, Hill26 reported that the presenting radiographic findings were a solitary nodule <4 cm in diameter in 23%, a mass in 20%, a localized area of consolidation (less than one lobe) in 7%, diffuse coalescent consolidation in 23%, and diffuse nodules in 27%. Unlike tumors of other cell types, the presence of air bronchograms in the areas of involvement is common. Less frequently, an interstitial pattern of involvement of the lung is noted, which Berkman3 reported to be the result of secondary lymphatic spread of the tumor. According to Sider,64 pleural effusion may be present in 8% to 10% of patients; rarely, a pneumothorax can occur.
Large-cell undifferentiated carcinomas are most likely to be peripheral lesions (approximately 60%); two-thirds of these are >4 cm. Cavitation occurs in approximately 6% of these peripheral large-cell tumors. A hilar abnormality and parenchymal changes are each present in association with approximately one-third of these tumors. Ten percent of patients with this type of tumor have mediastinal widening as one of the presenting features.
Small-cell undifferentiated tumors appear primarily as hilar abnormalities (78%), which usually represent hilar or mediastinal lymph node metastases. These tumors are associated with mediastinal widening in >13% of patients; in some of the patients with this finding, a parenchymal abnormality cannot be recognized. Parenchymal obstructive lesions occur as the result of extrinsic compression of a bronchus in slightly less than 40% of patients. A peripheral mass may occur in somewhat less than one-third of the patients. Carter and Eggleston8 reported that a peripheral mass occurred in only 14%. Three-fourths of the peripheral small-cell tumors may be <4 cm in diameter. This cell type represents the least common cause of a peripheral solitary pulmonary nodule of all cell types of bronchial carcinoma, and the reported incidence, as reviewed by Kreisman and associates,35 varies between 4% and 12%.
Despite these generalizations, no radiographic feature is diagnostic of the cell type or even of the presence of carcinoma. Nonetheless, these features should alert one to the possibility of a malignancy so that proper cytologic or histologic material can be obtained to make a diagnosis.
Special Radiographic Studies
In addition to the routine posteroanterior and lateral radiographs, other radiographs of the chest can be obtained with the patient in the right or left anterior oblique, lordotic, or other special position to delineate further any suspected lesion. Contrast-enhanced study of the esophagus and other radiographic studies (e.g., laminography, 55-degree oblique tomography, bronchography, angiography, azygography, and pneumomediastinography) can be obtained but are rarely indicated in the evaluation of lung cancer patients at present. These techniques are noted mainly for historic interest.
Computed Tomography of Lung Cancer
CT has become a routine examination for patients suspected of having lung cancer. Like any other noninvasive examination, however, it cannot distinguish inflammatory tissue from cancer tissue. In patients with central lesions, CT is useful for demonstrating enlarged hilar lymph nodes, but this finding in itself is not of great import because it does not disqualify the patient for surgical exploration. The demonstration of enlarged nodes may suggest, however, the need for a pneumonectomy as the surgical procedure. The caliber, distortion, and thickening of the wall of the proximal bronchi can also be discerned. Involvement of the pulmonary vessels, even with contrast enhancement, is difficult to determine at times. In patients with peripheral lesions, the margins, presence of calcification, and cavitation can be elicited. Zwirewich and associates82 evaluated high-resolution CT in distinguishing malignant from benign peripheral nodules. They found that spiculation of the borders, pleural tags, and bubble-like areas of low attenuation were present in 87%, 58%, and 25% of malignant lesions, respectively. In benign lesions, these percentages were 55%, 27%, and 9%, respectively. Thus, none of these criteria can be used as an unequivocal sign of malignancy.
Im and associates30 described the CT angiogram sign in patients with bronchioloalveolar carcinoma. With contrast enhancement in patients with segmented or lobar consolidation, enhanced branching pulmonary vessels are seen in areas of homogeneous low attenuation when the consolidation is related to the presence of this tumor. Air bronchograms may also be seen.
With high-resolution and spiral CT, numerous investigators, including Jang and associates,31 have described a ground-glass appearance as typical of small peripheral nodules that are early bronchioloalveolar carcinomas. This haziness is thought to be due to the lepidic growth pattern of these tumors. In addition, bubble-like hyperlucency or pseudocavitation (representing patent airways) can be present. With growth, areas of consolidation with high attenuation values may be seen. These areas represent so-called scar or sclerotic areas within the tumor. According to Noguchi,51 Eto,14 and Yamashiro81 and their colleagues, increasing size of the scar within the tumor portends a worse prognosis.
Calcification occurs as often as 13% of the time in lung cancer, as shown by Mahoney and coworkers40 in a CT study of lesions subsequently proved to be cancer. This calcification is most often eccentric. Concentric laminated calcification centered on the middle of a mass, however, is virtually diagnostic of a tuberculous or fungal granuloma, whereas diffuse calcification throughout the mass (“popcorn” calcifications) is the hallmark of a benign hamartoma.
However, the most important aspect of the radiologic diagnosis of lung cancer is that radiologic studies alone cannot make the diagnosis. Definitive diagnosis can be made only by cytology or histology. Therefore the chest radiograph and CT scan should be used primarily to raise the level of suspicion and to direct diagnostic procedures, such as bronchoscopy for central lesions or removal for peripheral lesions. It has been our practice not to do needle biopsies on new peripheral lesions in otherwise operable candidates without the presence of an alternative reason for a lung mass, thus saving the patient an operation. This is based on a personal review by one of us (R.H.F. in 1989, unpublished) of 2 years of fine-needle aspirations in this population. In it, only 3% of patients had a definitive benign diagnosis. It has far more often been the case that patients, falsely believing that a negative diagnosis meant benignity, were lost to follow-up until such time as they reappeared, only to find themselves inoperable.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree