Fig. 10.1
Dissection of the subplatysmal flaps well outside the area of skin incision (Reproduced from Zieliński [8], with permission)
10.4.2 Visualization of Both Vagus and Laryngeal Recurrent Nerves
Visualization of both laryngeal recurrent and vagus nerves is obligatory. To achieve this aim, it is necessary to cut the fascial layers of the carotid sheath covering these nerves [5]. The line of division of the fascia runs directly over the course of the carotid artery in the distance of at least 1 cm from the laryngeal recurrent and vagus nerves (Fig. 10.2). Any deviation to the medial side endangers the recurrent nerve localized medially to the artery, and deviation to the lateral side endangers the vagus nerve localized laterally. One must be aware of the possibility of the ima thyroid artery originating from the very distal part of the innominate artery in about 10 % of patients. The ima thyroid artery must be ligated or clipped and divided. After reaching the clean wall of the artery, the dissection of the laryngeal recurrent nerve is easily performed with the use of a peanut sponge. The right laryngeal nerve always runs along the line starting from the origin of the right subclavian artery towards the cricoid cartilage, and the left laryngeal recurrent nerve is localized in the groove between the trachea and the esophagus (Figs. 10.3 and 10.4). Discovery of both nerves is almost instant with a maneuver of retracting of the artery in the lateral direction with retractor and the trachea being retracted medially with a peanut or fingers, which makes the tissue containing the nerves stretched (Fig. 10.5). Due to this maneuver, the nerves are easily dissected with a peanut. During visualization of the recurrent nerves, it is recommended to preserve the last, deepest fascial membrane covering the nerve to avoid its injury. Circumferential dissection of any nerve is not advised.
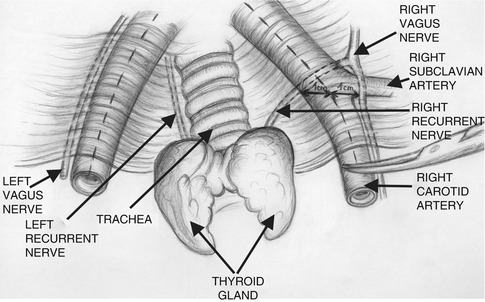
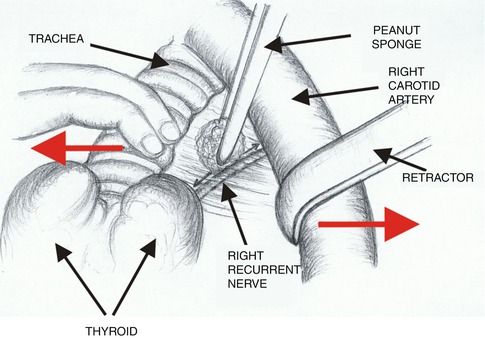
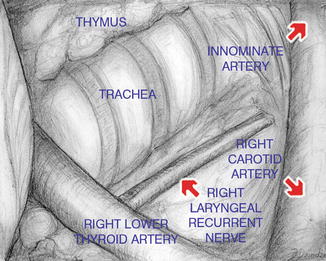
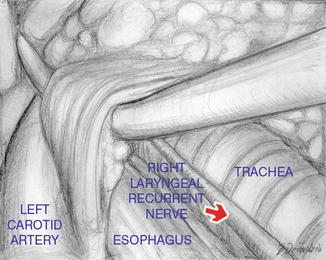
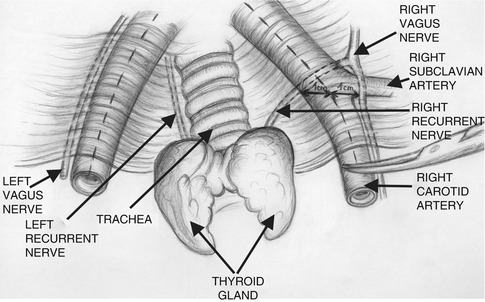
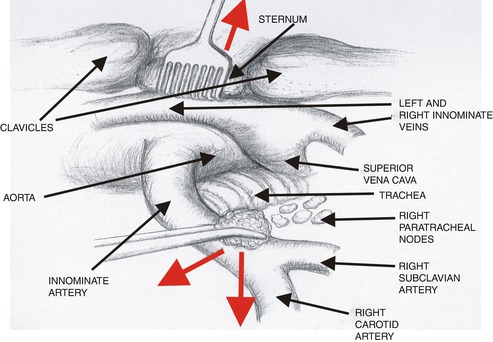
Fig. 10.2
Division of the fascial layers covering the laryngeal recurrent and vagus nerves. The line of division of the fascia runs directly over the course of the carotid artery (Reproduced from Zieliński [8], with permission)
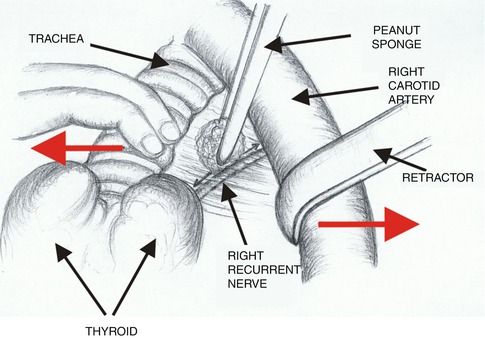
Fig. 10.3
Dissection of the right laryngeal recurrent nerve (Reproduced from Zieliński [8], with permission)
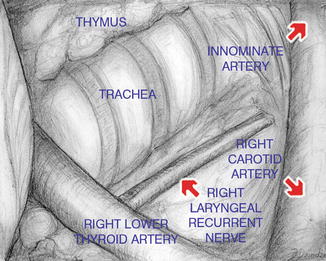
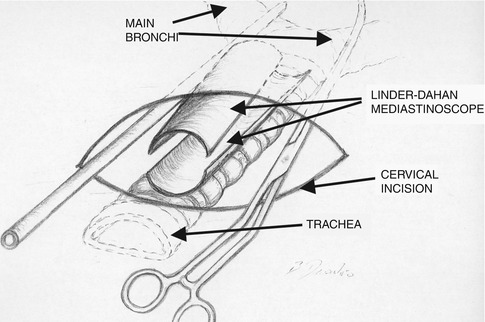
Fig. 10.4
Dissection of the right laryngeal recurrent nerve (Reproduced from Zieliński et al. [9], with permission from the European Association of Cardio-thoracic Surgery. Copyright 2005)
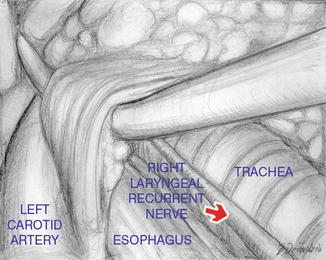
Fig. 10.5
Dissection of the left laryngeal recurrent nerve. To expose the nerve, the vascularized fascial layers covering the nerve must be divided (Reproduced from Zieliński et al. [9], with permission from the European Association of Cardio-thoracic Surgery. Copyright 2005)
Both vagus nerves run laterally to the carotid arteries. To expose these nerves, which are important landmarks of further dissection, one must perform the dissection inside the already opened carotid sheath laterally to the artery (Fig. 10.6).
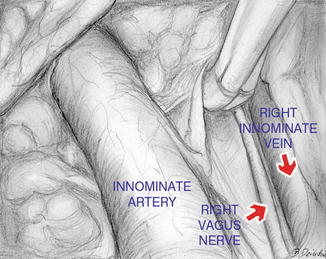
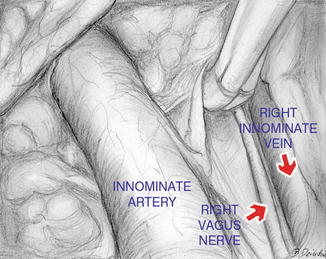
Fig. 10.6
Dissection of the right vagus nerve (Reproduced from Zieliński et al. [9], with permission from the European Association of Cardio-thoracic Surgery. Copyright 2005)
10.4.3 Insertion of the Hook Under the Sternum or Under the Sternoclavicular Joint
Elevation of the sternum with a hook inserted under the manubrium is an extremely important maneuver because it widens the access to the mediastinum (Figs. 10.7). We use a hook with sharp teeth (with one or three teeth) connected to the frame mounted to the operating table. In case of very obese patients, it might be safer to insert a hook under the sternoclavicular joint instead of the manubrium in order to avoid a disruption of the rim of the sternum. The surgeon stands behind the patient’s head and the assistant stands on the surgeon’s right side.


Fig. 10.7
Elevation of sternal manubrium with a hook connected to the modified Rochard frame
10.4.4 Dissection of the Highest Mediastinal Nodes (Station 1)
The next step is dissection of the highest mediastinal nodes (station 1), according to the Mountain-Dressler map and the recent International Association for the study of Lung Cancer Map [6, 7]. The innominate artery, previously dissected, is retracted posteriorly and cranially with a peanut sponge, which creates a wide entrance to the right paratracheal space (Fig. 10.8). Both innominate veins and the superior vena cava (SVC) are easily localized, and station 1 nodes, positioned cranially from the left innominate vein, are removed en bloc with the upper poles of the thymus (Fig. 10.9).
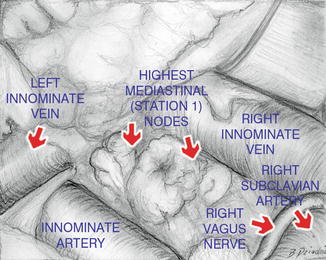
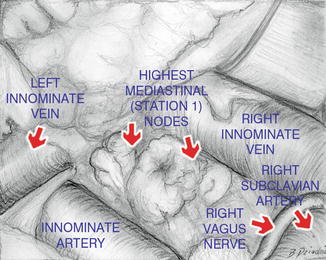
Fig. 10.9
Dissection of the highest mediastinal nodes (station 1) (Reproduced from Zieliński et al. [9], with permission from the European Association of Cardio-thoracic Surgery. Copyright 2005)
10.4.5 Dissection of the Right Paratracheal Nodes (Stations 2R and 4R)
The fatty tissue containing station 2R and 4R nodes is dissected from the trachea and the ascending aorta, medially; from the posterior wall of the SVC, anteriorly (watch out for the small venous tributaries coming from SVC); from the mediastinal pleura, laterally; and the right vagus nerve, posteriorly. Dissection is proceeded caudally until the right main bronchus and the azygos vein are visualized. The use of a long narrow retractor for a gentle lateral retraction of the mediastinal pleura with concurrent medial retraction of the trachea is very helpful in visualization of the azygos vein with further dissection continued deeper, below the azygos vein (Fig. 10.10). The origin of the right upper lobar bronchus and the upper (ascending) trunk of the right pulmonary artery is visualized, and the right hilar (station 10R) nodes are removed (Figs. 10.11 and 10.12).
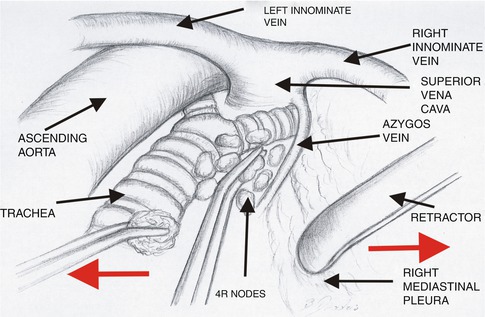
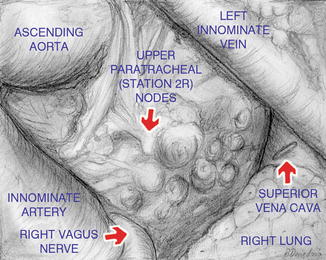
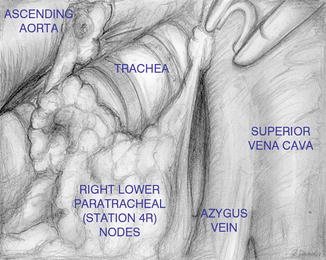
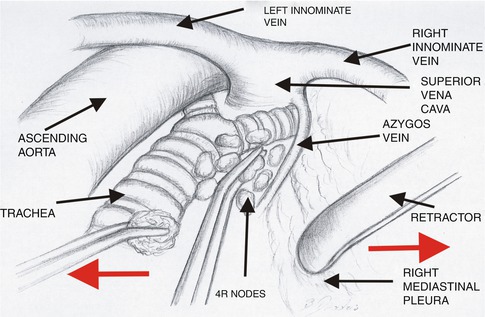
Fig. 10.10
Dissection of the right lower paratracheal nodes (station 4R) (Reproduced from Zieliński [8], with permission)
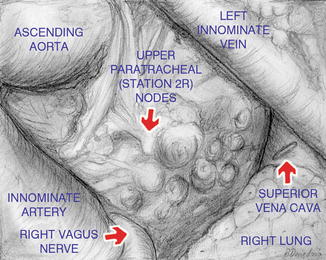
Fig. 10.11
Dissection of the upper paratracheal nodes (station 2R) from the ascending aorta, the azygos vein, the trachea, and the right main bronchus (Reproduced from Zieliński et al. [9], with permission from the European Association of Cardio-thoracic Surgery. Copyright 2005)
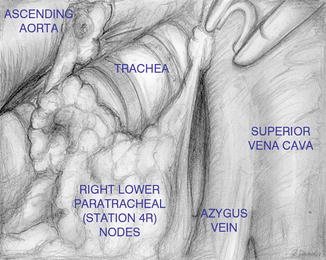
Fig. 10.12
Dissection of the lower paratracheal nodes (station 4R) from the ascending aorta, the azygos vein, the trachea, and the right main bronchus (Reproduced from Zieliński et al. [9], with permission from the European Association of Cardio-thoracic Surgery. Copyright 2005)
10.4.6 Dissection of the Prevascular (Station 3A) and Retrotracheal (Station 3P) Nodes
Station 3A (prevascular nodes) and station 3P (retrotracheal nodes) are removed in selected patients. Station 3A nodes lie below the left innominate vein, in front of the SVC, medially to the right mediastinal pleura, and laterally to the ascending aorta. These nodes are dissected after removal of station 1 nodes (Fig. 10.13). The left innominate vein and the SVC are retracted posteriorly with a peanut sponge, and the fatty tissue containing the 3A nodes is dissected from the structures mentioned above. In our experience, these nodes are rarely the site of metastasis.
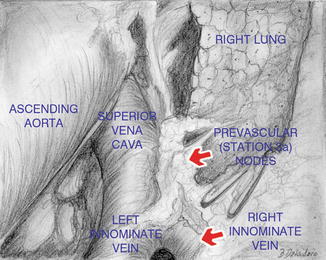
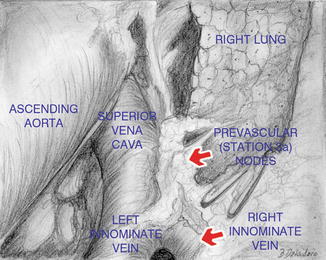
Fig. 10.13
Dissection and removal of the prevascular nodes (station 3A) (Reproduced from Zieliński et al. [9], with permission from the European Association of Cardio-thoracic Surgery. Copyright 2005)
The retrotracheal nodes (station 3P) are located behind the bifurcation of the trachea (Fig. 10.14). This area is approached in the same fashion as the right paratracheal nodes. The tracheal bifurcation is retracted anteriorly, which enables the visualization of the nodes lying in front of the esophagus. The nodes are easily removed; however, we never found any metastatic nodes in this station, and most often there are no visible nodes in this location at all.
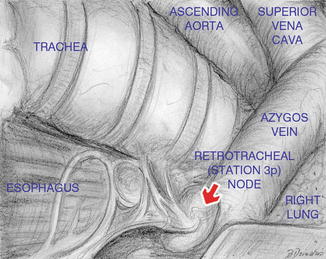
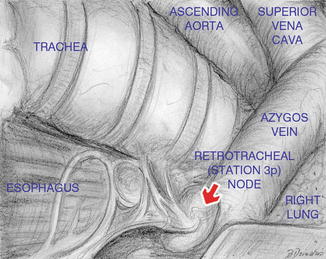
Fig. 10.14
Dissection and removal of the retrotracheal nodes (station 3P) (Reproduced from Zieliński et al. [9], with permission from the European Association of Cardio-thoracic Surgery. Copyright 2005)
10.4.7 Dissection of the Left Paratracheal Nodes (Stations 2L and 4L)
To remove the left paratracheal nodes, a retraction in the left lateral direction is applied on the left carotid artery. The trachea is retracted in the opposite direction with a peanut sponge (Fig. 10.15). The nodes lying above the top of the aortic arch and in front of the left recurrent nerve, previously dissected, are the upper left paratracheal nodes (station 2L) (Fig. 10.16). The adipose tissue containing station 4L nodes is dissected from the trachea, while the lateral connections of the nerve are preserved to avoid ischemic injury of the nerve. Station 4L nodes always lie posteriorly to the left recurrent nerve contrary to station 2L nodes which are localized in front of the nerve (Fig. 10.17). Removal of the distal part of station 4L nodes located along the left main bronchus is postponed until the subcarinal and periesophageal nodes (stations 7 and 8) are removed.
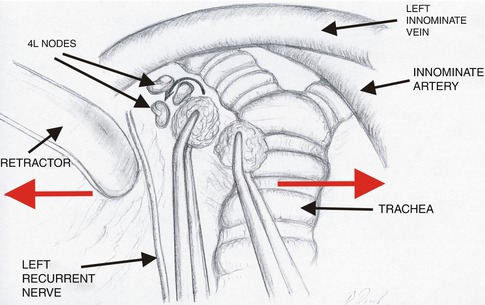
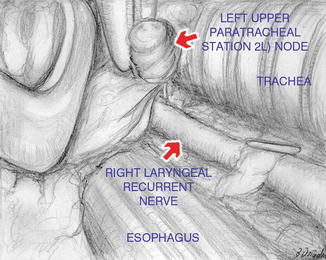
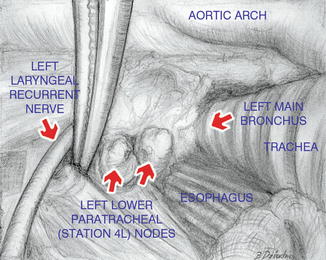
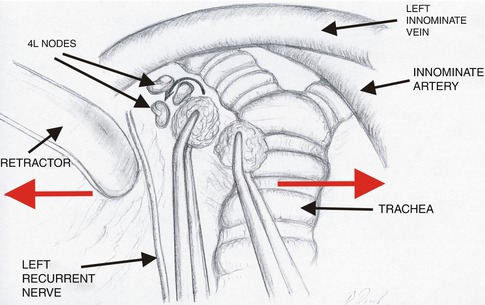
Fig. 10.15
Dissection of the left lower paratracheal nodes (station 4L) (Reproduced from Zieliński [8], with permission)
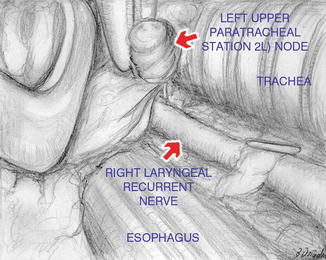
Fig. 10.16
Dissection and removal of the left upper paratracheal nodes (station 2L) (Reproduced from Zieliński et al. [9], with permission from the European Association of Cardio-thoracic Surgery. Copyright 2005)
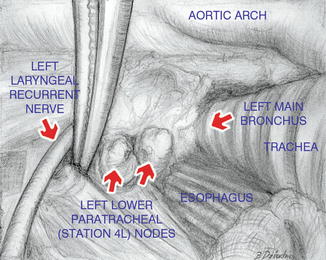
Fig. 10.17
Dissection and removal of the left lower paratracheal nodes (station 4L) (Reproduced from Zieliński et al. [9], with permission from the European Association of Cardio-thoracic Surgery. Copyright 2005)
10.4.8 Dissection of the Subcarinal (Station 7) and Periesophageal Nodes (Station 8)
This part of the TEMLA procedure is performed with use of the Linder-Dahan mediastinoscope (Wolf Company) with two spatulas enabling extension of the scope in two directions. To enter the subcarinal space, one must cut the fascial layer covering these nodes anteriorly. This step is started from the top of the angle made by the division of both main bronchi where usually a branch of the bronchial artery is found and should be coagulated. I found it useful to do it with BiClamp endoscopic dissector. The dissection is proceeded caudally along the medial walls of both main bronchi. The anterior wall of the esophagus is exposed at an early stage of the dissection to avoid injury of this structure. All bronchial arteries are coagulated with BiClamp. More prominent bronchial arteries might be clipped for additional security. The dissection is continued over the distance of several centimeters with the use of the suction cannula for suction of the smog created by coagulation and for stretching of the tissue. The endoscopic BiClamp dissector is used for coagulation of tissue, which is subsequently divided with scissors. Insertion of the instruments not through the lumen of the mediastinoscope but along the mediastinoscope enables clear visualization of the dissected structures and prevents “crowding” of instruments in the limited space (Fig. 10.18).