Tracheostomy
Joseph LoCicero III
Traditionally, tracheostomy was an operation at once lifesaving and dangerous to perform. It was among one of the first operations done in antiquity, and references to tracheostomy are evident in Egyptian artifacts dating back to 3000 Before the Common Era (B.C.E.). Because of the chance for saving lives, particularly in children with acute upper respiratory illnesses, it remained attractive to practitioners. However, the chance for grave harm was ever present. Tracheostomy was used sporadically throughout the Common Era (C.E.) until 1909, when Dr. Chevalier Jackson30 standardized the technique, which remains largely unchanged today.
Indications for Tracheostomy
Simply put, tracheostomy is indicated for upper airway obstruction, airway protection, or protracted or permanent ventilatory support. Airway obstruction most commonly occurs in children with severe acute upper respiratory illnesses such as epiglottitis, but it may also occur in adults as a result of trauma, typically blunt trauma. A tracheostomy may be important in the strategy of correcting complex laryngeal or tracheal pathology, such as laryngeal cancer or tracheal stenosis, to protect the airway during healing. But by far the most common indication for tracheostomy is prolonged ventilatory support for respiratory insufficiency. Examples include severe brain injury, posttraumatic respiratory distress syndrome, respiratory infections, and primary respiratory failure, as in chronic obstructive pulmonary disease (COPD). Sometimes these conditions cause excessive secretions, requiring airway access for frequent and repeated suctioning or bronchoscopy.
Contraindications for Tracheostomy
There are few firm contraindications for tracheostomy. Anatomic defects, severe soft tissue infections, and severe hypoxemia were the only ones listed by Blot and colleagues6 in their 2005 review. The last of these is the most significant. Placement of a new airway device requires a short but real period of apnea. Even in the best of hands, placement of the new tube may be difficult and the apneic period may be protracted. The patient must be able to tolerate this with some safety margin. Relative contraindications include excessive bleeding, large goiter, and severe kyphosis limiting access to the neck.
Advantages of Tracheostomy
Compared with orotracheal or nasotracheal intubation, a tracheostomy is a very stable platform for ventilatory access. The shortness of the tube, both in the airway and outside of the neck, allows for stable anchoring, leading to a very low incidence of accidental extubation. There is less movement of the tube within the trachea and hence limited damage to the tracheal mucosa. Eliminating the tube from the mouth allows for better oral hygiene, even in the sickest patients. If patients are conscious, they may mouth words. With time, families and health-care workers can carry on conversations with patients without additional appliances for speech. Since tracheostomy tubes are short and are placed directly into the trachea, they eliminate about 20 to 30 cm of the dead-space ventilation that is obligate with
endotracheal tubes. Eliminating this much dead space may improve the chances of weaning a patient with marginal pulmonary function from the ventilator.
endotracheal tubes. Eliminating this much dead space may improve the chances of weaning a patient with marginal pulmonary function from the ventilator.
Disadvantages of Tracheostomy
The disadvantages of a tracheostomy are few and are the same as the disadvantages of an endotracheal tube. However, for some family members, placement of a tracheostomy tube signals a finality to hope of recovery. Although this is not based in fact, families often have a tough time transitioning from a hope for rapid recovery to one of protracted rehabilitation. These situations almost always arise with an unexpected illness or event that has led to a period of prolonged critical care. In such cases, the care team must be supportive while also providing helpful information on the meaning of a tracheostomy.
General Preoperative Considerations
Anatomy
Chapter 79 presents a thorough discussion of the detailed anatomy of the trachea. Only a few important features are highlighted here. First, as the trachea enters the chest, it begins to move posteriorly to sit behind the great vessels. Thus, in the supine position, the trachea makes a 45-degree angle to the horizontal. This fact, underappreciated by the occasional surgeon of the trachea, can lead to a disastrous mediastinal intubation.
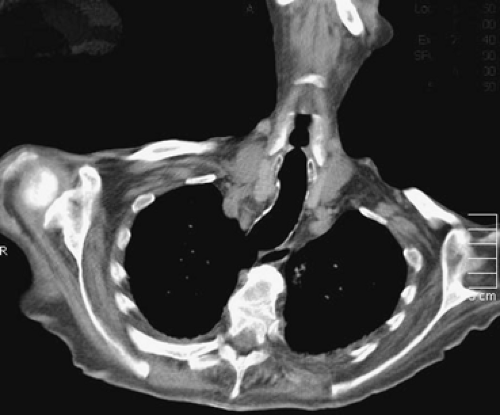
Elderly patients have particular considerations. The larynx and trachea seem to descend into the chest in the elderly. In fact, the trachea has not shortened, but owing to osteoporosis and kyphosis, the neck moves forward over the sternum and is forced further down into the chest. The second and third tracheal rings, marking the traditional insertion point for the tracheostomy tube, may sit beneath the sternal notch. The thyroid isthmus is more prominent in this situation and may have to be divided in an open tracheostomy, leading to the potential for hemorrhage. The angle of descent of the trachea may be even more exaggerated, to the point that the cervical trachea may be 90 degrees to the horizontal, as demonstrated in Figure 78-1. The aorta elongates as elasticity is lost, causing the brachiocephalic trunk to rise toward the neck at the same time that the trachea is descending. As a result, the potential for vascular injury increases.
Although rare (at 0.2%–0.5%), the thyroid ima artery, which originates centrally, ascends into the neck anterior to the trachea to supply the inferior pole of the thyroid gland; it can be a source of significant hemorrhage. However, of more significance in the critically ill patients with poor cardiac function is venous engorgement, which causes most of the operative hemorrhage.
Evaluation
Any patient requiring a tracheostomy should be evaluated, just like any other patient about to have a surgical procedure. One must assess if the patient exhibits cardiopulmonary stability and can tolerate brief (up to 2 minutes) of apnea. The ability to form clot is important, so clotting studies should demonstrate an adequate platelet count and an international normalized ratio (INR) of less than 1.6. Clotting factors can be corrected prior to the procedure with appropriate blood components.
Physical examination should focus on the head and neck to define the patient’s particular anatomy and special considerations. These include evidence of soft tissue integrity and freedom from infection, suppleness and stability of the neck, amount of adiposity, and vascular concerns such as a high-riding brachiocephalic trunk.
Ultrasound evaluation of the neck and airway, currently of increasing interest, may be a simple preoperative diagnostic tool. Sustić52 describes the technology as widely available, portable, repeatable, relatively inexpensive, pain-free, and safe. It is usually available in the emergency department and intensive care unit (ICU) for guidance in the placement of central lines. Greater expertise in evaluation of the airway comes with experience.
Current Preoperative and Operative Controversies
Timing of Tracheostomy
Holevar and colleagues,26 in conjunction with the Eastern Association for the Surgery of Trauma, have developed a consensus statement for the timing of tracheostomies in patients with traumatic injuries resulting in respiratory failure or ventilator dependence. They noted that there is no mortality difference between patients receiving early tracheostomy (3–7 days) and late tracheostomy or extended endotracheal intubation. They observed that early tracheostomy decreases the total days of mechanical ventilation and ICU length of stay in patients with head injuries. Therefore they recommend that patients with a severe head injury receive an early tracheostomy. Finally, they noted
that early tracheostomy may decrease the total days of mechanical ventilation and ICU length of stay in trauma patients without head injuries. Early tracheostomy may decrease the rate of pneumonia in trauma patients. Therefore it is recommended that early tracheostomy be considered in all trauma patients anticipated to require mechanical ventilation for >7 days.
that early tracheostomy may decrease the total days of mechanical ventilation and ICU length of stay in trauma patients without head injuries. Early tracheostomy may decrease the rate of pneumonia in trauma patients. Therefore it is recommended that early tracheostomy be considered in all trauma patients anticipated to require mechanical ventilation for >7 days.
With regard to adults who are critically ill, some data exist. De Leyn and associates15 along with the Belgian Society of Pneumology and the Belgian Association for Cardiothoracic Surgery developed guidelines on tracheotomy for mechanical ventilation in adults. They reviewed several studies. One in particular performed a convincing meta-analysis of five studies. Griffiths et al.22 found that early tracheotomy significantly reduced duration of artificial ventilation by 3 to 20 days and length of stay by 11 to 21 days in the ICU. Based upon this study and others, they recommended that “In critically ill adult patients requiring prolonged mechanical ventilation, tracheotomy performed at an early stage (within the first week) may shorten the duration of artificial ventilation and length of stay in intensive care (level 1B).”
Location of Procedure
As hospital resources wane, operative time becomes more precious, and less invasive techniques improve, there is a push to perform all tracheostomies at the bedside. This is especially true when patients requiring tracheostomies are ill and subject to development of conditions that would prevent the procedure, such as gastrointestinal hemorrhage or sepsis. In addition, many of these patients are scheduled for a variety of studies and procedures that are not well coordinated within a busy hospital. In studying an unpublished survey of 300 tracheostomies performed at Maimonides Medical Center in a year, the operating room executive committee found that the average time from the operating room being ready to accept the patient to the time the patient left the operating room after the procedure exceeded 2 hours. They also noted a 20% cancellation rate, often after the operating room had been prepared and significant complications such as hypoxemia, hypotension, and cardiopulmonary arrest had occurred in over 3% of the scheduled patients. This prompted a policy change to perform tracheostomies at the bedside whenever possible. Still, for open tracheostomy procedures, operating room staff and equipment are used. Particularly in percutaneous dilational tracheostomies, the procedure may be performed at the bedside with little additional staff. At Maimonides, these percutaneous tracheostomies are performed on regular medical–surgical floors with one assistant and the patient’s nurse. To make the areas outside of the operating room safe and effective, planning and education of the staff are necessary. Barba5 summarized the process and enumerated the necessary steps.
Choice of Tracheostomy Size
Large hospital buying groups and market pressures often dictate the manufacturer of the tracheostomy tube. However, the choice of size remains up to the physician. For crycothyroidotomies, much smaller tubes are used to prevent permanent damage. For a standard adult open or percutaneous tracheostomy, the choice is between 6 and 10 mm. In the past, surgeons and intensivists tended to use larger tubes because older bronchoscopic equipment would not fit through a 6-mm inner cannula. Currently, all newly purchased bronchoscopes will pass through a 6-mm tracheostomy inner cannula. With a smaller size, there is less damage to the anterior trachea and thus a theoretically lower rate of stomal complications. For special situations, a Shiley XLT (Nellcor Puritan Bennett LLC, Boulder, CO) tube may be designed to fit a specific neck. This tube can be ordered with varying initial (proximal) lengths, variations in the curved portion of the tube, and varying lengths of the distal tube. All of these tubes may be placed percutaneously with the newer kits.
For children, there are additional considerations. Irving29 and later Wyatt56 and their co-workers described the merits of different types of pediatric tracheostomy tubes and their indications based on patient size. Table 78-1 provides useful information pertaining to pediatric airways and tube selection.
Open Versus Percutaneous Procedures
Arguments among practitioners abound at institutions throughout the country concerning the merits of open versus percutaneous methods of tracheostomy. Because the technique of percutaneous tracheostomy is easily taught and a variety of specialties can perform the procedure, the question is becoming moot. Many thoughtful reviews and meta-analyses overwhelmingly demonstrate that, under protocol-driven controlled conditions with appropriately trained operators and staff, the results of percutaneous tracheostomy are as good and in some instances better than those of open tracheostomy. Some of the reluctance to accept percutaneous tracheostomy was due to an initially high complication rate with the older multiple dilator technique. Kost31 demonstrated that there was as much as a 40% complication rate in the early experience and an overall 14% complication rate for the multiple dilator technique, compared with a 10% early and 6% overall complication rate for the single dilator technique.
Table 78-1 Pediatric Airways and Corresponding Tube Sizes According to Age | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||
Two recent meta-analyses demonstrate the superiority of percutaneous tracheostomy. Delaney and associates16 reviewed 17 randomized controlled trials involving 1,212 critically ill patients. Despite the fact that most investigators used a multiple dilator technique, percutaneous tracheostomy was equivalent to open tracheostomy for bleeding, major periprocedural and long-term complications. Furthermore, subgroup analysis suggested that percutaneous tracheostomy resulted in a lower incidence of bleeding when the open tracheostomy was performed in the operating room. Higgins and Punthakee25 reviewed 15 randomized controlled trials and 1,000 patients not limited to the ICU. In a more detailed analysis, they discovered that there were significantly fewer complications in the percutaneous group with respect to wound infection and unfavorable scarring. Although trends favored percutaneous tracheostomy, there was no statistically significant difference for complications of false passage, minor hemorrhage, major hemorrhage, subglottic stenosis, death, and overall complications. They did note a higher complication rate: in one study in particular, there was a higher rate of difficulty due to early tube complications. Most of these studies used kits with percutaneous tracheostomy tubes that did not have an inner cannula, leading to more mucous plugging. This was corrected when manufacturers redesigned the system to allow the use of standard tracheostomy tubes with inner cannulas.
Description of Operative Techniques
Standard Open Tracheostomy
There is nothing standard about the standard open tracheostomy. Although Jackson30 tried to standardize the procedure, nearly every hospital has an established, unique approach employing some permutation of the varieties of techniques. Moreover, hospital operating rooms have tracheostomy trays that vary from institution to institution with a myriad of tools, some basic, some from antiquity, and some with purposes long forgotten. Open tracheostomies are done under local anesthesia with or without sedation or general anesthesia with or without neuromuscular paralysis. The skin incision is either vertical or horizontal. The trachea is either dissected out or barely visualized. Traction sutures are placed laterally or not at all. The tracheal incision is performed vertically or horizontally or a trap door superiorly or inferiorly is made; or the trachea is trephined. After placement, the tracheostomy tube is sewn to the skin or the wound and twill tape or Velcro straps are used for security.
Only a few important milestones and tips can be offered with a procedure steeped in such local traditions. Planned tracheostomies should never be hurried operations. The patient deserves to be comfortable, without pain, whatever anesthetic technique is used. Vertical incisions are helpful if the tracheal anatomy cannot be defined prior to incision, but this results in a problematic scar. Traction sutures are of benefit only in the very early postoperative period; they assist in replacement of the tube if it becomes dislodged; however, adequate visualization of the trachea is essential to a satisfactory result. Any incision that deviates from Jackson’s original vertical incision results in loss of tracheal wall and possible stenosis. The tracheostomy tube should be inserted with the curve 90 degrees laterally to the trachea and then rotated back to midline to assure easy placement. Each method of securing the tube is as good as any other.
Cricothyroidotomy
The technique of cricothyroidotomy is reserved for emergent situations when the patient has upper airway obstruction or the patient cannot be intubated through the pharynx. The main reason is that the cricoid membrane is a constant and easily palpable landmark making for a high probability of success. However, there is a much higher incidence of subglottic complications including vocal cord dysfunction. Sise and colleagues48 described the approach with particular attention to the membrane incision. They made a cruciate incision in the membrane and placed the tube while holding the space open.
Technique of Percutaneous Tracheostomy
Ciaglia and associates11 reported the technique of percutaneous dilational tracheostomy. After a number of iterations, the system is mature. The contents of the most popular kit, the Ciaglia Blue Rhino (Cook Medical, Inc., Bloomington, IN) are shown in Table 78-2. The kit is complete with the exception of scissors to cut the tape on the endotracheal tube and the Velcro tracheostomy tape.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree