INDICATIONS/CONTRAINDICATIONS
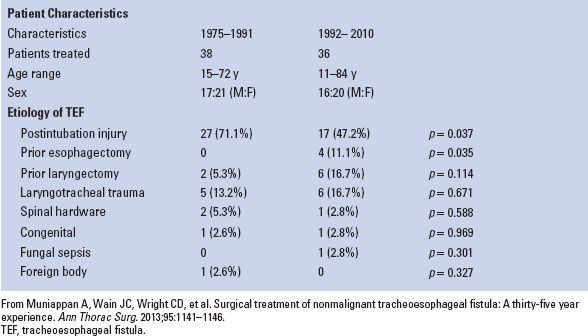
Acquired nonmalignant tracheoesophageal fistula (TEF) most commonly arises as a complication of endotracheal intubation. Pressure exerted by the endotracheal tube cuff on the tracheal wall leads to circumferential necrosis and potential for fistulization. The presence of a nasoenteric feeding tube greatly increases this risk. High-volume, low-pressure endotracheal tube cuffs and avoidance of prolonged nasoenteric tube placement have reduced but not eliminated this complication. Nonmalignant TEF may also occur secondary to blunt or penetrating trauma, in the setting of mediastinal inflammatory or granulomatous disease, or as a late complication following esophagectomy or laryngectomy (Table 38.1).
The presentation of TEF ranges considerably. Some patients may develop overwhelming pulmonary sepsis and inability to wean from the ventilator; others may present with chronic cough and aspiration years after intubation. In all cases the presence of TEF mandates surgical repair. Once formed there is little hope of the fistula closing with conservative measures alone, and the natural history of the condition is one of the intractable pulmonary complications and death. Continued mechanical ventilation is considered a relative contraindication to repair because positive pressure ventilation postoperatively is a risk factor for failure of the tracheal repair. However, in some patients the fistula represents the major impediment to ventilator weaning, and so, repair must be considered under suboptimal conditions.
Several approaches to repair of nonmalignant TEF have been described. The most conservative approach is a two-stage repair involving tracheal resection and reconstruction along with esophageal diversion, followed by interval esophageal reconstruction. Hermes Grillo demonstrated that similar results could be achieved with a single-stage tracheal resection and reconstruction and primary esophageal repair with muscle flap interposition. We believe this approach remains the gold standard for management of nonmalignant TEF. Others have proposed primary repair of both trachea and esophagus. This may be adequate for small fistulae but leads to unacceptably high rates of recurrence when the fistula is large. The increasing popularity of tracheal and esophageal stents in the field of thoracic surgery has led some to propose their use in the management of nonmalignant TEF. We feel that luminal stents are inadequate in that they do not address the underlying fistula and have potential for considerable harm by recreating the conditions under which the fistula formed leading to potential extension of the defect, and by making definitive repair more difficult. However, for malignant TEF—which usually occurs in the setting of aggressive cancer with a poor prognosis—luminal stents should be employed to achieve the goal of palliation.
TABLE 38.1 Patient Characteristics and Etiology of TEF
 PREOPERATIVE PLANNING
PREOPERATIVE PLANNING
Preparation for operative repair of nonmalignant TEF focuses on two things: Control of pulmonary sepsis by preventing further aspiration, and optimizing nutritional status. In the patient with a tracheostomy in place the former can be accomplished by placing a long tracheostomy tube with the cuff inflated distal to the fistula. Placement of a gastrostomy tube for drainage and a jejunostomy tube for feeding ensures that the patient will receive enteral nutrition with minimal aspiration risk. This approach excludes the fistula while improving the patient’s overall clinical condition. Every attempt should be made to wean a patient from the ventilator before undertaking operative repair.
All patients undergoing repair of a TEF should undergo preoperative bronchoscopy and esophagoscopy. Understanding the anatomy and precise location of the fistula as well as the condition of the uninvolved trachea and esophagus is a crucial part of operative planning. Active tracheal inflammation is often the cause to delay elective tracheal resection and reconstruction for management of tracheal stenosis; however, in the case of TEF it is unlikely that tracheal inflammation will subside completely and delaying repair for this reason would be inappropriate.
 SURGERY
SURGERY
Repair of a nonmalignant TEF is a complex operation that should only be performed by an experienced thoracic surgeon at a high-volume center. Issues to emphasize include: Involvement of an experienced anesthesia team, complete resection of all involved trachea, two-layered longitudinal repair of the esophageal defect, and interposition of a suitable muscle flap between the repaired esophagus and the tracheal anastomosis.
Anesthesia
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


