INDICATIONS/CONTRAINDICATIONS
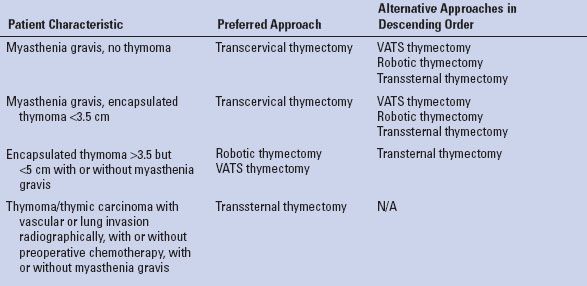
Controversy surrounds the selection of the surgical approach to thymectomy. Clearly, the emergence and refinement of minimally invasive procedures has challenged the routine application of transsternal thymectomy. Patients with nonthymomatous myasthenia gravis likely benefit from a minimally invasive approach as long as the resection is complete. Similarly, patients with small, well-encapsulated thymomas are likely good candidates for minimally invasive approaches. In our current practice patients with large (>5 cm), well-encapsulated thymomas, patients with clearly invasive lesions who are pretreated with chemotherapy, and all patients with thymic carcinoma undergo a transsternal thymectomy. Figure 28.1 shows the pre- and post-treatment images of a patient who is offered a transsternal resection. This approach allows for easy resection of concomitant involved structures such as lung, chest wall as well as major vascular structures requiring resection and possible reconstruction. Table 28.1 summarizes our current approach to thymectomy based on the clinical situation.
There are no major contraindications to transsternal thymectomy. In patients with prior cardiac surgery it is important to know the route of any coronary grafts and their proximity to the inner table of the sternum and the thymoma. These patients should be approached in the same way one would approach a redo sternotomy for cardiac surgery. The graft location should be mapped out preoperatively with either coronary catheterization or CT angiogram. I prefer CT angiogram. The sternum must be opened carefully to avoid damage to any underlying patent grafts. Cardiopulmonary bypass should be available and a plan must be in place should replacement of coronary graft be required either due to injury opening the sternum or due to tumor involvement.
Patients with pectus excavatum can present a challenge. In my experience I have performed transsternal thymectomy with no attempt to repair the pectus resulting in satisfactory outcomes. The lack of working domain makes minimally invasive approaches difficult in these cases although some have reported sternal lift type procedures, which may be applicable and may allow for adequate working domain.
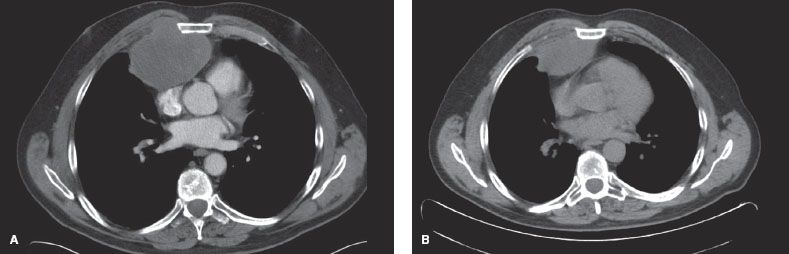
Figure 28.1 CT scan of the chest showing a patient with a thymic carcinoma. A: Shows the initial presenting scan and (B) shows the postchemotherapy scan. The patient subsequently underwent complete resection including partial resection of the sternum and right anterior chest wall. He was reconstructed with a combination of mesh and methylmethacrylate, which was covered with a pedicled muscle flap.
 PREOPERATIVE PLANNING
PREOPERATIVE PLANNING
All patients should have a CT scan with intravenous contrast. With large, poorly encapsulated lesions suggestive of invasive thymoma or thymic carcinoma the patient undergoes a preoperative biopsy either by CT-guided needle biopsy or by anterior mediastinotomy (Chamberlain procedure) followed by preoperative chemotherapy. Following chemotherapy treatment patients undergo repeat enhanced CT scan prior to definitive resection for planning purposes. In these situations attention is focused on the possible need for vascular reconstruction.
If not already performed we also obtain acetylcholinesterase antibodies in all patients undergoing thymectomy. These tests can be helpful in uncovering patients with impeding myasthenia gravis despite noticeable symptoms. As part of the preoperative discussion we always inform patients that a percentage of patients with thymoma and no symptoms of myasthenia gravis may develop the disease later in life.
TABLE 28.1 Current Surgical Approach to Thymoma Based on Clinical Scenario
Clinically, many large thymomas are “phrenotropic.” Although most, none myasthenic patients can tolerate a neuropraxia or paralysis of a single phrenic nerve, this can have catastrophic effects in the myasthenic patient. The possibility of phrenic nerve injury should be discussed with all patients undergoing thymectomy by any approach.
Patients undergo preoperative pulmonary function testing. In myasthenia patients these serve as a base line; following the force vital capacity postoperatively to ensure adequate muscle strength for unassisted respiration.
As mentioned above, patients with prior coronary artery bypass surgery undergo graft mapping to determine the location and patency of each graft. Completely occluded grafts, which are involved with an invasive thymoma or thymic carcinoma, can be sacrificed. Patient grafts coursing through or inseparable from the thymoma must be bypassed.
 SURGERY
SURGERY
The patient is brought to the operating room receives routine prophylactic antibiotics and preinduction subcutaneous heparin for DVT prophylaxis. For myasthenic patients the anesthesia team, surgical team, and nursing team review the list of contraindicated drugs in the preoperative meeting to assure they are not administered during or after the case. General anesthesia is administered and the patient is intubated with a left-sided double-lumen endotracheal tube. The tube is positioned for isolated lung ventilation with the help of a pediatric bronchoscope to allow for lung isolation if required during the resection.
Positioning
The patient is placed in a supine position with the arms tucked at the sides. A roll is placed length wise under the shoulder blades to extent the neck and drop the shoulders. For particularly large difficult lesions and for those patients with prior sternotomy the groins are prepped into the field and additional arterial or venous access should be acquired. When the lesion appears to involve the superior vena cava, caval atrial junction, or the innominate vein I always place intravenous access above and below the diaphragm, so that intravenous medication can be administered during times of intermittent caval clamping. For complex caval reconstruction, which requires more than a side-biting caval clamp with partial occlusion or a short complete clamping caval–atrial bypass, should be considered to avoid cerebral congestion due to venous outflow occlusion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


