INDICATIONS/CONTRAINDICATIONS
Tracheal stenosis or obstruction most commonly develops in the setting of postintubation injury (stomal or cuff injury), primary and secondary tumors of the airway, and trauma, in order of decreasing frequency. Patients are symptomatic when the cross-sectional area is reduced by more than 50% or the diameter of the tracheal lumen is less than 5 to 6 mm. Tracheal resection and reconstruction (TRR) may be appropriate for definitive correction of all of these conditions. Tracheal resection is distinguished from laryngotracheal resection in that the lesions are confined to the trachea and do not involve the cricoid or subglottic airway.
TRR is generally not appropriate for patients requiring mechanical ventilatory support, as positive airway pressures predispose to anastomotic complications. TRR is also inadvisable in patients requiring a high dose of corticosteroid, which can impair healing. Extended lesions of the trachea that involve more than half its length may not be resectable as anastomotic tension may be too great. Advanced age, obesity, short stature, kyphosis, and prior tracheal or mediastinal surgery must also be factored when selecting patients for TRR. When TRR is undertaken for an airway neoplasm, it is important to rule out distant metastasis or invasion of a mediastinal structure that cannot be resected.
 PREOPERATIVE PLANNING
PREOPERATIVE PLANNING
Plain chest radiography may identify an abnormal tracheal air column and establish the level of the tracheal pathology. Computed tomography (CT) is much more sensitive and provides more accurate localization and measurement of tracheal disease. Inspiratory and expiratory CT imaging can visualize dynamic obstruction, for instance when tracheomalacia is responsible for inspiratory collapse of the trachea. CT is vital for evaluation of neoplastic disease, as it determines whether or not there is invasion of adjacent mediastinal structures or if there is evidence of distant metastatic disease.
Bronchoscopy is much more specific and sensitive than imaging in the evaluation of tracheal disorders. Tracheal narrowing may be over- or underestimated on imaging studies. Bronchoscopy is used to measure the extent of the lesion and determine whether a lesion is resectable. Rigid bronchoscopy is the most versatile technique as it is not only diagnostic but also therapeutic when used to dilate critical airway stenoses. Rigid bronchoscopy and core-out of tracheal neoplasms restores the airway and provides tissue for histologic diagnosis. There is virtually no indication for emergent TRR, and bronchoscopic management is sufficient to assess and stabilize the patient’s airway.
When a patient’s condition requires prolonged mechanical ventilation, a tracheostomy may be necessary. The stoma is carefully located in the diseased segment of the trachea so as to not extend the amount of diseased trachea that would eventually require resection. It is important to wean patients from mechanical ventilation before undertaking TRR. Similarly, patients requiring high-dose corticosteroid therapy are weaned completely or to a very low dose prior to TRR.
 SURGERY
SURGERY
Anesthesia
Induction of anesthesia is performed with the surgeon present. A laryngeal mask airway may be sufficient for ventilation and permits flexible bronchoscopy. A rigid bronchoscope must be available if anesthetic induction leads to complete airway obstruction. Jackson bougie dilators and small ventilating rigid bronchoscopes (3 to 5 mm size) are effective at dilating very tight strictures. Once dilation is completed, the anesthesiologist may intubate with a size 5 to 6 orotracheal tube. A pediatric flexible bronchoscope may facilitate navigation of the tube through the stenosis.
Positioning
Patients are positioned supine with a bag inflated under their shoulders to extend the neck; a gel pad supports the occiput (Fig. 35.1). The arms are left at the sides, and the knees and hips are slightly flexed so as to prevent blood pooling in the lower extremities. The patient is prepped from the chin to just beneath the xiphoid.
Technique
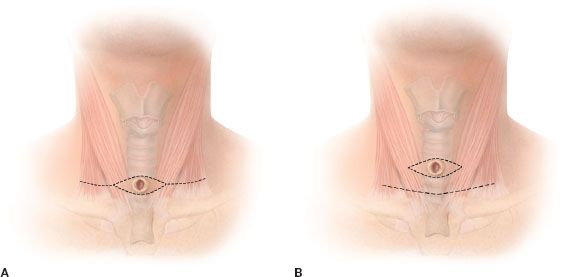
A low cervical collar incision is made and subplatysmal flaps are raised (Fig. 35.2). The superior flap should be at least to the level of the cricoid cartilage and the inferior flap is made down to the sternal notch. Gelpi retractors are used to distract the flaps and maintain exposure (Fig. 35.3). On occasion, a cervicomediastinal approach is necessary if the lesion is in the lower half of the trachea (Fig. 35.4). In this case, a T-shaped incision, including the low-collar component and an extension in the midline down to the sternal angle is made. The sternum is divided in the midline down to the angle and a pediatric chest spreader distracts the manubrium. Total sternotomy does not enhance exposure. A right thoracotomy is generally only necessary for the most distal tracheal resections, which approach the carina. The collar incision may have to circumscribe a tracheal stoma, when one exists (Fig. 35.2).
The midline anatomy is established by dissecting down to the anterior surface of the trachea. The sternohyoid and sternothyroid strap muscles are mobilized and retracted with a Weitlaner retractor. The thyroid isthmus is divided if it has not been previously. Anterior dissection right on the airway is performed to isolate the tracheal pathology. As the tracheal vasculature is segmental and enters laterally, circumferential dissection must be restricted to the lesion that is to be resected. As the surface appearance of the trachea does not always reveal the location of the endoluminal pathology, bronchoscopic transillumination at the stenosis or tumor allows marking sutures to be placed on the surface, to guide further dissection and plan airway division. The endotracheal tube may need to be pulled back to visualize the endoluminal disease.

Figure 35.1 Patient positioning. A bag is inflated beneath the shoulders, extending the neck. The arms are by the side. The table is adjusted to flex the patient at the hips and knees.