Chapter 48 Thrombolysis for Deep Venous Thrombosis and Pulmonary Embolism
Acute Iliofemoral Venous Thrombosis
Acute obstruction of the single channel outflow from the lower extremity (common femoral, external iliac, and common iliac veins) leads to high compartment and venous pressures. Qvarfordt and colleagues1 reported compartment pressures in patients with iliofemoral DVT who subsequently underwent venous thrombectomy. These patients had high compartment pressures, which is a surrogate for venous pressure upon presentation. Following thrombus removal and restoration of venous outflow, compartment pressures returned to normal.
In a study evaluating venous hypertension by measuring arm-foot pressure differential, Labropoulos and colleagues2 showed that patients with postthrombotic obstruction of the iliofemoral venous system had the highest venous pressures (highest arm-foot pressure differential).
Anticoagulation alone for iliofemoral DVT reduces the risk of pulmonary embolization and reduces the extension of thrombus. Unfortunately, obstruction of the venous outflow channel remains, producing significant venous hypertension. Figure 48-1 is a photograph of a man who had iliofemoral DVT treated with anticoagulation alone 3 months earlier. Despite therapeutic anticoagulation and wearing 30- to 40-mm ankle-gradient compression stockings, he suffered with venous claudication, swelling of the lower extremity, and skin discoloration in the lower leg, with the ascending phlebogram showing extensive deep venous obstruction. Another ascending phlebogram (Figure 48-2) of a patient with severe postthrombotic morbidity and venous ulceration 10 years after anticoagulation alone for iliofemoral DVT shows the extensive amount of venous obstruction. The day following the phlebogram, the patient underwent a classic Linton procedure. The operative photograph of his postthrombotic femoral vein demonstrates the fibrotic obstruction with webbing and synechiae that occur in these patients, causing much more anatomic obstruction to venous return than can be appreciated on the phlebogram.
Natural History Studies
Natural history studies of patients with acute DVT treated with anticoagulation alone have revealed a number of important principles. Meissner and colleagues3 followed patients with acute DVT with sequential venous duplex examinations. Some patients had the good fortune to lyse their thrombus during the first few months of observation, whereas in others the thrombus remained. Their observations demonstrated that when thrombus lysed early (within 60-90 days), patients were likely to retain normal valve function. However, valve reflux occurred in patients whose thrombus did not lyse. In longer term follow-up studies, these authors demonstrated that patients who did not have early lysis had a significantly higher recurrent DVT rate.4
Kahn and colleagues5 performed a prospective analysis of 387 patients with acute DVT. Their intent was to evaluate postthrombotic syndrome following acute DVT. These authors found that patients with iliofemoral DVT had the most severe postthrombotic morbidity (odds ratio [OR], 2.23; p < 0.001). They also found that the patients’ clinical condition at 1 month was the best predictor of long-term outcome (p < 0.001).
A number of authors have followed patients with iliofemoral DVT who were treated with anticoagulation alone.6,7 These patients uniformly suffered with chronic venous disease. Within 5 years, 15% developed venous ulceration and up to 40% had venous claudication. The patients’ quality of life was significantly diminished.
One frequently overlooked observation is that recurrent DVT is more frequent in patients with iliofemoral DVT than in patients with femoropopliteal DVT.8 This is likely due to the large burden of thrombus that remains in the venous system following anticoagulation alone.
Venous Thrombectomy
The purpose of this is not to address operative venous thrombectomy. The principles of restoring patency, normalizing venous pressures, and long-term benefits are well illustrated by the randomized trial performed by Plate and colleagues.9–11 The Scandinavian investigators randomized patients with iliofemoral DVT to venous thrombectomy plus arteriovenous fistula followed by anticoagulation or anticoagulation alone. A careful follow-up at 6 months, 5 years, and 10 years demonstrated significant benefits in patients who underwent venous thrombectomy. Patients randomized to thrombectomy had improved patency, lower venous pressures, less leg swelling, and fewer postthrombotic symptoms compared with anticoagulation alone. These data illustrate the benefit of eliminating obstruction to venous drainage from the leg to the vena cava. The details of contemporary operative venous thrombectomy have been recently reviewed by Comerota and Gale.12
Catheter-Directed Thrombolysis
All drugs currently used for thrombolytic therapy are plasminogen activators. As a result, clot dissolution occurs as a result of plasminogen being activated, resulting in the production of plasmin, which is the active clot dissolving enzyme. Plasminogen circulates as an inactive zymogen. In the systemic circulation, free plasminogen circulates as GLU-plasminogen. When thrombosis occurs, plasminogen binds to fibrin and is altered, forming LYS-plasminogen, which is more susceptible to activation by a plasminogen activator. Alkjaersig and colleagues13 demonstrated that the basic mechanism of clot lysis by plasminogen activators is the activation of fibrin-bound plasminogen within the thrombus to form plasmin, which is the active enzyme that dissolves the clot. If plasmin escapes into the systemic circulation, it is instantaneously neutralized by α-2-antiplasmin or, secondarily, α-2-macroglobulin. Low doses of plasminogen activators are neutralized in the systemic circulation by plasminogen activator inhibitors. Pharmacologic doses of plasminogen activators persist in the circulation because they supersaturate circulating plasminogen activator inhibitors.
Systemic thrombolytic therapy is an inefficient method of treating acute DVT. A relatively small amount of systemically infused plasminogen activator will contact the thrombus to activate fibrin-bound plasminogen. The results of studies evaluating systemic thrombolytic therapy for acute DVT have been disappointing and generally are associated with higher than acceptable bleeding complications and lower than acceptable success rates.14 It is understandable that techniques for delivering the plasminogen activator into the thrombus, thereby maximally activating fibrin-bound plasminogen and minimizing the systemic delivery of the plasminogen activator, will be associated with greater success rates and fewer bleeding complications.
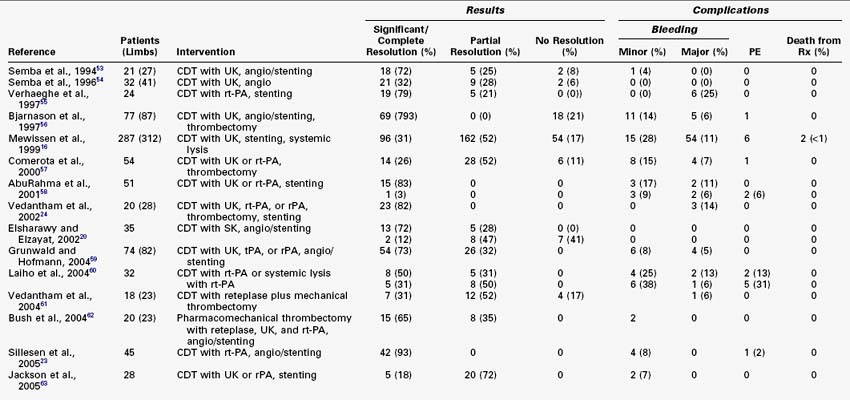
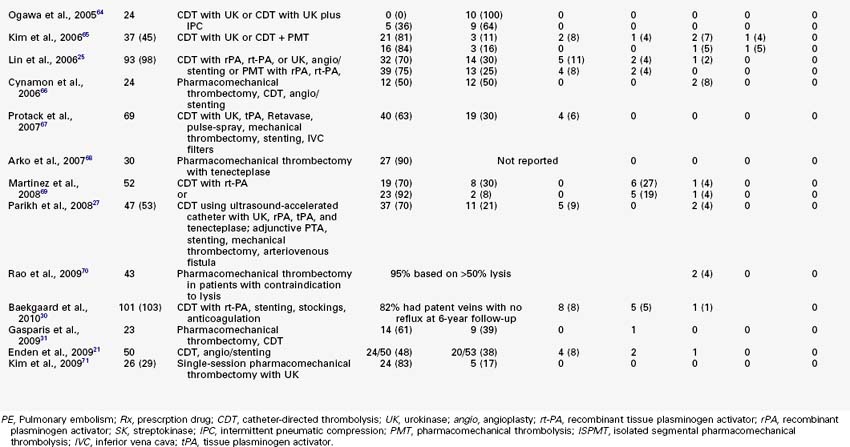
Numerous reports have demonstrated good outcomes of catheter-directed thrombolysis (CDT) for acute DVT. Most of these reports (20 limbs or more) are listed in Table 48-1, which also includes pharmacomechanical techniques used as adjuncts to CDT. In general, when patients with acute DVT are treated with catheter-based techniques, success rates in the range of 75% to 90% can be anticipated. The rate of bleeding complications ranges from 5% to 11%. Fortunately, serious distant bleeding is uncommon and intracranial bleeding is a rarity. Most bleeding complications are localized to the venous access site, and reports surfacing in the past 7 years generally report bleeding complications as 5% or less. Symptomatic pulmonary embolization during infusion is uncommon, and fatal PE is rare.
An interesting report by Chang and coauthors15 documented the benefit of intrathrombus bolus dosing of recombinant tissue plasminogen activator (rt-PA) in a small group of patients (10 lower extremities with acute DVT), which has been recently updated. The pulse-spray technique was used to infuse 50 mg of rt-PA delivered intrathrombus by catheter infusion on a daily basis. Patients underwent the pulse-spray technique, returned to their rooms, and were brought back the following day for complete phlebographic evaluation and additional treatment if necessary. Patients were treated for a maximum of four sessions of pulse-spray thrombolysis. Significant or complete lysis was achieved in 11 of 12 extremities, and 1 had 50% to 70% lysis. Although the average dose of rt-PA was 106 mg, bleeding complications were minor and in no patient did the hematocrit drop more than 2%. This small patient sample draws attention to the importance of high-pressure pulse-spray infusion into the thrombus by demonstrating that lysis will continue long after the treatment session ends if the rt-PA is bound to the plasminogen within the clot. It also raises the question of whether one needs the full 50-mg dose. Patients may have responded equally as well to a smaller dose of rt-PA delivered in a larger volume of solution.
The National Venous Registry16 reported a large cohort of patients treated with lytic therapy for acute DVT. Seventy-one percent of these patients had iliofemoral DVT and 25% had femoropopliteal DVT. It is interesting to note that patients with iliofemoral DVT seem to have had better and more durable results than patients with femoropopliteal DVT.
A quality-of-life (QOL) study was performed to assess whether lytic therapy altered QOL in patients with iliofemoral DVT.17 A cohort-controlled study in the institutions participating in the National Venous Registry was performed. Patients with iliofemoral DVT treated by CDT were compared with a contemporary cohort of patients with the same extent of DVT and from the same institutions who were treated with anticoagulation alone. All patients treated with anticoagulation alone were candidates for lytic therapy; however, the choice of treatment was determined by physician preference. Patients were evaluated with a validated QOL questionnaire that was used to query patients at 16 and 22 months following acute treatment.18 Ninety-eight patients were evaluated; 68 were treated with CDT and 30 were treated with anticoagulation alone. The results demonstrated that CDT was associated with better QOL than anticoagulation alone. QOL was directly related to thrombolytic success. Patients who had a successful lytic outcome reported a better Health Utilities Index, improved physical functioning, less stigma of chronic venous disease, less health distress, and fewer postthrombotic symptoms. Not surprisingly, patients in whom CDT failed had outcomes similar to those treated with anticoagulation alone. A subsequent single-center observational study demonstrated that QOL following CDT for iliofemoral DVT directly correlated with success of clot lysis.19
A small, randomized trial performed by Elsharawy and Elzayat20 compared CDT with anticoagulation alone. CDT resulted in significantly better patency and valve function at 6 months. Enden and colleagues21 reported preliminary results from an ongoing trial of 200 patients randomized to CDT with tPA versus anticoagulation alone with low-molecular-weight heparin followed by warfarin. The preliminary report included approximately half of the projected 200 patients. The primary outcome of this study was patency of the iliofemoral venous segment at 6 months and the incidence of postthrombotic syndrome at 2 years. Preliminary observations indicate significantly better patency in patients randomized to CDT compared to those treated with only anticoagulation. The study has not yet matured to the point of commentary on postthrombotic morbidity.
Patient Evaluation and Technique
Patients with iliofemoral DVT have a large thrombus burden and appear to have a greater stimulus to thrombosis than most other patients with acute infrainguinal DVT. It appears warranted that a search for an underlying etiology should occur. Asymptomatic pulmonary emboli are present in at least 50% of these patients. It would seem appropriate to identify asymptomatic pulmonary emboli early, because up to 25% will subsequently become symptomatic, manifesting as pleuritic chest discomfort once the inflammatory pulmonary process or parenchymal infarct reaches the pleural surface.22 If the PE is not recognized at presentation, clinicians may mistakenly assume that the subsequent pleuritic symptoms are due to a new PE resulting from failure of treatment. A spiral computed tomographic (CT) scan of the chest with contrast evaluates the pulmonary vasculature for PE and other thoracic pathology. The CT scan is then extended to the abdomen and pelvis to identify the proximal extent of thrombus and to evaluate for abdominal or pelvic pathology. This process has been an important addition to the evaluation of these patients, because previously undiagnosed pathologies have been found with surprising frequency. Evaluation of the brain, chest, abdomen, and pelvis is recommended. Renal cell carcinoma, adrenal tumors, retroperitoneal lymphoma, pulmonary adenocarcinoma, hepatic metastases, iliac vein aneurysms, vena caval atresia, and asymptomatic abdominal aortic aneurysms have all been identified. Hematologic evaluations for an underlying thrombophilia are selectively performed, although it may be more useful to obtain a thrombophilia workup in young, female, first-degree relatives of childbearing potential than in the patient being treated.
Pharmacomechanical Thrombolysis
Although good results have been achieved with CDT, treatment times are often unacceptably long; therefore bleeding risk and cost associated with therapy are unacceptably high. A recent report of extensive DVT treated with CDT alone demonstrated a 93% success rate.23 These patients were generally treated within 7 days of symptom onset. It would be expected that lysis could be achieved efficiently in these patients, because they represented a true acute DVT; however, treatment times for CDT alone averaged 71 hours. This duration of acute care is logistically difficult, if not impossible, for many practitioners and many medical centers. The associated cost is high because patients receiving lytic therapy are generally monitored in intensive care units; therefore techniques to speed lytic success will be important for efficient and effective patient care.
Endovascular Mechanical Thrombectomy
Mechanical techniques alone or in combination with thrombolysis have been developed to more rapidly clear the venous system. Vedantham and associates24 evaluated the effectiveness of mechanical thrombectomy alone or in combination with pharmacologic thrombolysis in 28 limbs of patients with acute DVT. They evaluated multiple devices. Venographic scoring was performed at each step of the procedure. Twenty-six percent of the thrombus was removed by mechanical thrombectomy alone, whereas adding a plasminogen activator solution to the mechanical technique (pharmacomechanical) removed 82% of the thrombus. Mechanical thrombectomy (rheolytic technique) alone was highly successful when removing intraprocedural thrombus, which is usually gelatinous and not cross-linked by factor XIII. The average infusion time was approximately 17 hours per limb, and 14% of patients had major bleeding complications.
Rheolytic Thrombectomy
Lin and colleagues25 reported their 8-year experience with pharmacomechanical thrombolysis using a rheolytic thrombectomy catheter. Of their 98 patients, 46 received CDT alone and 52 underwent pharmacomechanical thrombolysis using the AngioJet catheter (Medrad, Minneapolis, Md.). Their observations demonstrated that the pharmacomechanical technique was associated with significantly fewer phlebograms, shorter intensive care unit stays, shorter hospital stays, and fewer blood transfusions. Bleeding complications were not different between the two groups. A smaller patient group treated by rheolytic thrombectomy was reported by Kasirajan and associates,26 who demonstrated that mechanical thrombectomy alone was less effective than the combined pharmacomechanical technique.
Ultrasound-Accelerated Thrombolysis
Parikh and colleagues27 reported an initial clinical experience with ultrasound-accelerated thrombolysis in 53 patients treated for acute DVT with the EKOS EndoWave system (EKOS, Bothell, Wash.). Both upper- and lower-extremity DVT patients were included as well as use of a variety of lytic agents. This makes a comparison with other reports difficult, because axillosubclavian DVT responds more quickly than lower-extremity venous thrombosis.
Isolated Segmental Pharmacomechanical Thrombolysis
Martinez and coworkers28 reviewed 52 consecutive limbs treated for iliofemoral DVT, the first 27 with CDT alone and the following 25 with isolated segmental pharmacomechanical thrombolysis (ISPMT) plus CDT when necessary. Thrombus burden and treatment outcomes were quantified. Ninety-three percent of the patients were treated with rt-PA. Venoplasty and stenting were used to correct underlying stenoses, and all received long-term therapeutic anticoagulation. Sixteen of the 27 limbs treated with CDT required adjunctive mechanical techniques to clear the thrombus, such as the AngioJet, ultrasound-accelerated lysis, or pulse-spray techniques, whereas only 7 of the limbs treated with ISPMT had additional mechanical techniques. A larger percentage of the thrombus was removed with ISPMT than with CDT. Complete lysis (≥90%) was achieved in 11% of the limbs of CDT patients as opposed to 28% of the limbs treated by ISPMT (p = 0.077). Treatment time was shorter (23.4 vs. 55.4 hours; p < 0.001) and the rt-PA dose was lower (33.4 vs. 59.3 mg; p = 0.009) with ISPMT. Hospital and intensive care unit length of stay was no different, which appeared to be a result of underlying patient comorbid conditions. Only 18% of the limbs had complete lysis following the use of the ISPMT catheter alone. Bleeding complications occurred in 5% of patients undergoing CDT alone and 5% of patients treated with ISPMT.