Chapter 27 Endoscopic Harvesting of the Saphenous Vein
Open vein harvest for coronary artery bypass grafting and infrainguinal bypass procedures is associated with increased patient morbidity and postoperative wound complications.1 In the limb salvage population, patients exhibit severe peripheral arterial occlusive disease, marginal distal perfusion, poor nutrition, and infected wounds. These factors make it difficult to heal lower-extremity skin incisions required to harvest long, continuous segments of saphenous vein required for optimal bypass patency. Over the past decade, endoscopic harvest of the saphenous vein and the radial artery has been increasingly used by cardiac surgeons for coronary artery bypass grafting and has become the standard of care within this specialty.
More recently, these techniques have been used increasingly for minimally invasive harvest of autogenous conduits in conjunction with peripheral vascular surgery. Because longer, continuous segments of conduit are required for infrainguinal revascularization, especially infrapopliteal bypass, certain technical modifications have been required to facilitate use for lower extremity limb salvage procedures.2
Results
Endoscopic Vein Harvesting: Coronary Artery Bypass Grafting
Several prospective, randomized trials have compared endoscopic vein harvest (EVH) with traditional open saphenous harvest during coronary artery bypass grafting and have demonstrated superior outcomes for EVH. Advantages include lower wound complication rates, decreased postoperative pain, increased patient satisfaction, improved cosmesis, and equivalent graft patency rates.3–8 Griffith and colleagues9 performed a histologic analysis of veins harvested by open techniques and EVH. There was no difference in endothelial, smooth muscle, and elastic lamina continuity between the two groups. Medial and adventitial connective tissue uniformity was also not significantly altered.
Despite multiple supportive studies validating EVH for coronary artery bypass grafting (CABG), a recent study by Lopes and colleagues10 questioned the superiority of this technique. They reviewed the outcomes of 1753 patients who underwent EVH for CABG and compared them to 1247 patients in the open harvest group. They demonstrated a higher rate of vein-graft failure at 12 to 18 months in the EVH group compared with the open cohort (46.7% vs. 38%, respectively). At 3 years, endoscopic vein harvest was also associated with higher rates of death, myocardial infarction, and repeated revascularization. Critics of this study highlighted the elevated vein-graft failure and death rates in both open and EVH groups compared with similar published series. Additional criticisms included an overall lower use of internal mammary artery conduits, which are associated with superior patency compared with vein grafts, and that 20% of the procedures in this patient cohort were performed off-pump.
A recent study performed by the Northern New England Cardiovascular Disease Study Group demonstrated a decreased risk of leg wound infections with EVH, but an increased adjusted risk of bleeding requiring a return to the operating room.11 Endoscopic harvest was also associated with a significant reduction in long-term mortality in these patients. The results also demonstrated that between 2001 and 2004, the use of EVH increased from 34% to 75% in patients requiring CABG.
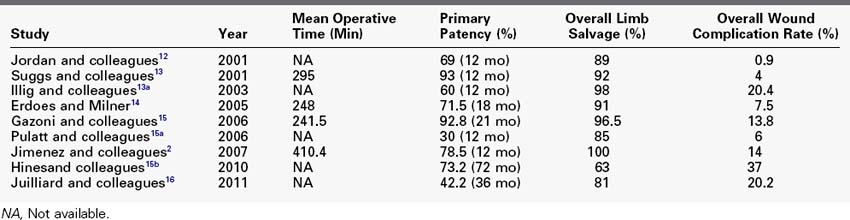
Endoscopic Vein Harvesting: Infrainguinal Revascularization
Several studies have demonstrated similar favorable results for EVH during distal arterial bypass for limb salvage, although no randomized controlled trials have been conducted (Table 27-1).12–15 Jordan and colleagues12 performed 164 saphenous vein EVHs for lower extremity arterial reconstructive procedures over a 6-year period.12 A review of patency rates using Kaplan-Meier analysis at 1, 3, and 5 years demonstrated vein graft patencies of 85%, 74%, and 68%, respectively. Fourteen patients (8.5%) developed wound infections during the 30-day postoperative period, and two patients developed harvest site hematomas. None of these wound complications led to either graft failure or limb loss. The limb salvage rate was 89%.
A review by Erdoes and Milner14 examined the outcomes following EVH for infrainguinal arterial bypass in 214 limbs over a 6-year period. The indication for bypass was limb salvage in 88.3%, claudication in 9.3%, and trauma and aneurysm in 2.4%. Assisted primary patency at 18 months was 77.2% by Kaplan-Meier analysis. Wound complication rates were 7.5%, with 2.5% of patients requiring readmission to the hospital. Only one patient early in the series required conversion to an open harvest.
Gazoni and colleagues15 reported results for patients who underwent femoral to below-knee arterial bypass grafting over a 27-month period.15 Fifty-nine patients underwent traditional open saphenectomy, and 29 had EVH. There was a trend toward improved patency rates in the EVH group compared with open harvest, although no statistically significant difference was noted (92.8% vs. 80.6%). No significant differences were found between the two groups in postoperative complications, operative time, length of hospital stay, patency rates, limb salvage, and death. The incidence of wound complications was 3.4% in the EVH group and 15.3% in the open harvest group, although this difference also was not statistically significant. Similarly, Hines and colleagues examined outcomes over a 5-year period for 27 patients who underwent femoral-popliteal bypass with EVH in patients with Trans-Atlantic Inter-Society Consensus (TASC) D disease of the superficial femoral artery.15b Kaplan-Meier primary and primary assisted patency rates were 73.2% and 80.8% at 1 year, respectively, and these rates were maintained for 70 months. Only one patient developed a superficial wound infection.
Following formal systematic training by vascular surgeons and implementation of technical modifications specific to limb salvage procedures at our institution, we noted 30-day primary and primary-assisted patency rates of 85.7% and 92.9%, respectively.2 Kaplan-Meier primary assisted patency was 63.6%. No patients required primary amputation at 19 months. One graft occlusion occurred within 30 days as a result of a tunnel hematoma in a patient who sustained a postoperative myocardial infarction and required therapeutic anticoagulation. One late hematoma was noted, and one patient demonstrated skin necrosis at the level of the ankle requiring prolonged hospitalization. Complete wound healing was achieved in 75% of patients with preoperative tissue loss owing to critical limb ischemia.
Recently, the long-term durability of EVH for lower-extremity bypass has been questioned following a study by Julliard and colleagues.16 Over a period of 8.5 years, 363 patients underwent infrainguinal bypass; 170 patients underwent EVH, and 193 underwent traditional open saphenous vein harvest. No differences in indication for surgery were noted between groups. Primary patency rates were significantly lower in the EVH group compared with the open group at 6, 12, and 36 months. There were no differences in length of stay or wound complication rates. Limb salvage and survival were also identical between groups. The differences were not significant in patients with claudication and in those without diabetes.
Techniques
Endoscopic Harvest of the Greater Saphenous Vein
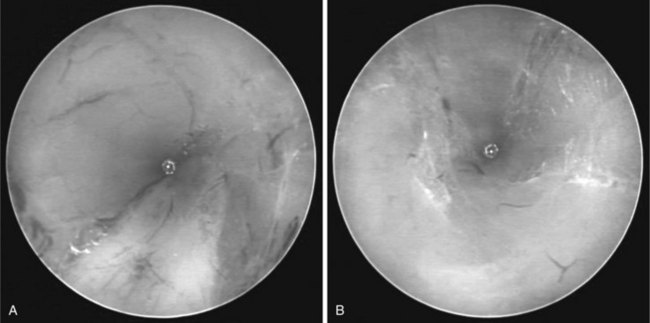
An incision is made three fingerbreadths posterior to the medial femoral or tibial condyles depending on whether harvest will be performed above or below the knee. A longitudinal 2 cm incision is made and the GSV is identified. A Silastic vessel loop is placed around the GSV for mobilization (Figure 27-1). At this time, several more centimeters of vein are bluntly dissected and mobilized from the surrounding subcutaneous tissue to ease placement of the blunt tip trocar (BTT) in the direction of intended vein harvest. The BTT is placed into the subcutaneous space overlying the GSV, and sufficient air is inflated into the port balloon to ensure a good seal with the adjacent skin. Leakage of CO2 outside the harvest tunnel can lead to suboptimal visibility and bleeding during vein mobilization. A CO2 cannula is then attached to a port on the BTT and continued at a flow rate of 3 to 5 L/min up to a maximum pressure of 10 to 15 mm Hg. Carbon dioxide insufflation should not exceed central venous pressure to avoid embolism. Insufflation of the vein harvest tunnel facilitates placement of the 5-mm camera through the main port of the BTT and enhances visualization of the GSV within the subcutaneous space.
A conical tip is placed on the tip of the camera, and the vein is dissected bluntly along its anterior and posterior surfaces (Figure 27-2). Branches are skeletonized from surrounding soft tissue and exposed to maximal length before division with the bipolar dissector. The main goal before division of branches is to suspend the entire length of the vein by its branches in the center of the harvest tunnel and allow maximal CO2 insufflation for good visibility (Figure 27-3). Care must be taken at this time to avoid avulsion of large branches. Generally the disruption of minor venous branches is not problematic, because the insufflation tends to control bleeding from these tributaries without the need for additional cauterization.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree