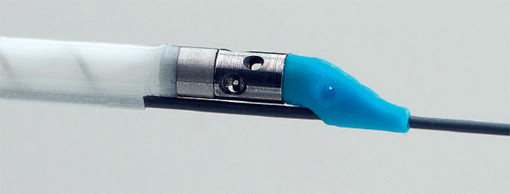
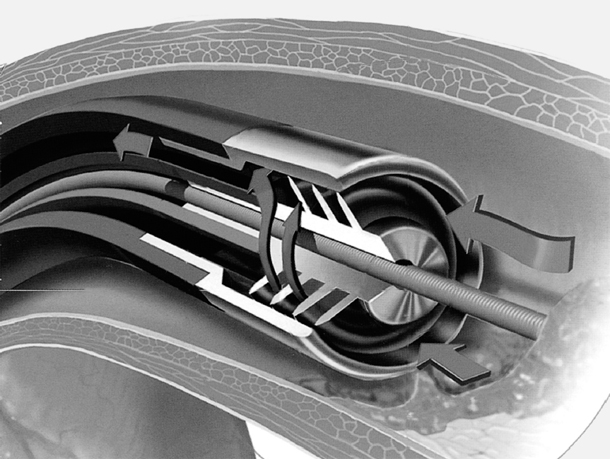
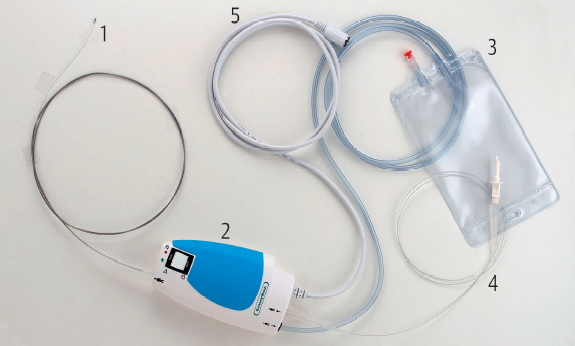
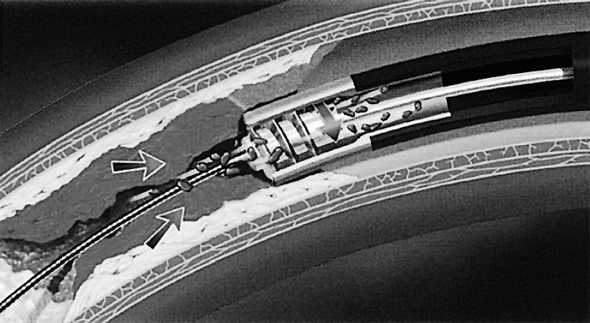
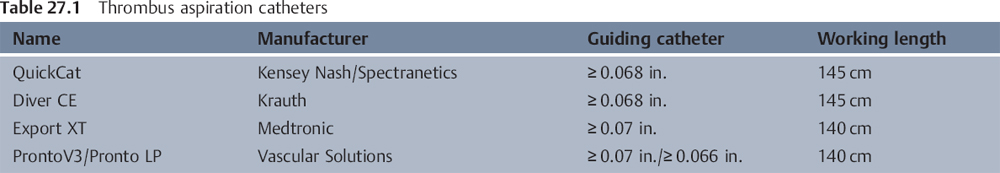
27 Thrombectomy and Protection Systems The use of percutaneous coronary intervention (PCI) to treat stenoses with demonstrable thrombi or high plaque burden, especially in the case of diffusely affected coronary vein grafts, involves a high risk of peripheral vessel occlusions. Peripheral embolizations can cause reduced perfusion (“no reflow”) and myocardial infarctions. In addition, primary PCI for an acute coronary syndrome often results in myocardial hypoperfusion due to embolization of plaques and thrombi. Even the use of GP IIb/IIIa inhibitors does not always lead to unimpaired perfusion (TIMI flow < 3) or prevent distal embolization with vessel occlusions on the microvascular level. Aspiration and thrombectomy catheters represent a therapeutic approach to address this issue. Aspiration catheters basically consist of a catheter with a terminal opening and distal side holes (Fig. 27.1). All aspiration catheters are 6F-compatible with an external diameter of 0.066 to 0.07 in. Larger catheters impede the pressure measurement via the guiding catheter. The systems usually have an internal diameter of 1.0 to 1.1 mm. All catheters are advanced as monorail systems via a 0.014-in. wire. Aspiration is done with a syringe that is connected to the end of the catheter and used to generate suction. The most frequently used catheters are summarized in Table 27.1. Aspiration catheters are efficacious in removing fresh thrombi and atheromatous material, for example, in acute coronary syndrome with symptoms of no more than 12 hours, or in the context of a fresh periprocedural atheroma activation. Older thrombi—especially in acute coronary syndromes more than 24 hours after symptom onset or thrombi in chronically degenerated vein grafts—cannot be removed effectively with this technique. Here mechanical systems are clearly better. The catheter consists of the following components: 1. Aspiration catheter with a diameter of 0.066 to 0.07 in. 2. 30-mL aspiration syringe that can be locked 3. Extension with stopcock 4. Sieve to filter the aspirated blood 5. Guiding catheter, at least 6F (internal diameter ≥ 0.07 in.) 6. Guidewire, 0.014 in. The ThromCat system (Spectranetics, Colorado Springs, CO, USA) is single-use and consists of a catheter, a control and drive unit, a collection bag, an infusion system, and a power cord with connection to a power supply (Fig. 27.3). Its function is based on the principle of the Archimedes’ screw (Fig. 27.4). The system contains two helices: one infusion helix and one extraction helix. The control unit drives the helices, so that the infusion helix pumps saline from the saline bag into the catheter and the extraction helix generates a vacuum of −700 mm Hg. The helix rotates at 95,000 rpm. The vacuum aspirates the thrombus into the openings of the catheter, macerates it inside the catheter, and transports it to the collection bag. The catheter has a profile of 5.5F and a working length of 150 cm. The infusion rate is 15 mL/min and ~45 mL/min is extracted. The system has a flexible, atraumatic tip. The helix is completely encapsulated, thus there is no direct contact with the vessel wall. Fig. 27.3 Individual components of the ThromCat system. 1 Catheter 2 Drive unit 3 Collection bag for the aspirate 4 Connection for flush 5 Electrical connection This method is indicated for the percutaneous transluminal removal of thrombi from native coronary arteries and infrainguinal arteries with a diameter of 2.5 to 7.0 mm. The technique can be used for both fresh and older thrombi. The method is not indicated for The system consists of the individual components mentioned above (Fig. 27.3) plus: 1. Guiding catheter: size 7F (≥ 0.078 in.) or sheath: size 6F (≥ 0.078 in.) 2. Standard guidewire: 0.014 in. 3. Y-connector to be connected to the guiding catheter The disadvantages of the technique are the equipment required and the associated costs. An advantage is the potential to completely remove older thrombi. Personal view In our view the technique is very easy, efficacious, and safe. The X-Sizer system (EndiCOR Medical Inc., San Clemente, CA, USA) consists of a helical rotating cutting system housed in the distal tip of a flexible double-lumen catheter. This system also works according to the principle of the Archimedes’ screw. The double-lumen catheter is connected to a hand-held, battery-powered control module that rotates the cutter at 2,100 rpm. The generated vacuum entraps the thrombus, the Archimedes’ screw draws in material and shears it, and then the material is removed by the vacuum lumen into the connected collection bottle (Figs. 27.5, 27.6, 27.7). The system is available in two sizes: 1.5 mm and 2.0 mm cutting diameter. The procedure can be performed with 7F to 8F standard guiding catheters and 300 cm long 0.014-in. standard guidewires. There is no specific atraumatic, flexible tip at the catheter end (Fig. 27.7). Fig. 27.6 Mechanism of action of the X-Sizer system according to the principle of the Archimedes’ screw. The most important indications for thrombectomy with the X-Sizer system are Use of the X-Sizer system is not indicated for The system (Fig. 27.5) consists of a pre-assembled system in two sizes (diameters of 1.5 mm [4.5F] and 2.0 mm [5.5F]) with a drive unit and two vacuum collection bottles. The AngioJet thrombectomy catheter (MEDRAD, Inc., Warrendale, PA, USA; Fig. 27.8) was developed to remove thrombi safely from the coronary arteries without embolization. From the catheter tip, six high-velocity saline jets are directed into a specially designed catheter, so that a vacuum is generated according to the Bernoulli principle. The thrombotic material is broken up and removed through the catheter. To achieve this effect, a pressure of 6,000 atm (608 MPa) is applied to the catheter, which due to the decrease in pressure within the catheter is reduced to 170 atm (17 MPa) at the catheter tip. The six saline jets at the catheter tip can achieve speeds of up to 500 km/h (300 miles per hour) (Fig. 27.9). Before the procedure, the catheter is connected to a specific console and filled. The heparinized saline introduced into the catheter is directed on its return into a special collection container for later examination. Thus, in addition to thrombectomy, an effective thrombolysis is also done. Due to the size of the catheter only vessels with a diameter of > 2 mm can be treated. The intervention can be performed with 6F standard guiding catheters and 190 cm long 0.014-in. standard guidewires. The most important indications for thrombolysis and thrombectomy with the AngioJet system are The use of the AngioJet system is not indicated for
Aspiration Catheter
 Basics
Basics
 Indications and Contraindications
Indications and Contraindications
 Materials
Materials
Preparation of the System
 Flush the lumen, extension, and stopcock of the catheter.
Flush the lumen, extension, and stopcock of the catheter.
Procedure of Aspiration
 Advance the catheter via the wire until at least the end of the catheter and before the atheroma or the thrombus.
Advance the catheter via the wire until at least the end of the catheter and before the atheroma or the thrombus.
 Open the lock so that suction is applied.
Open the lock so that suction is applied.
 Under fluoroscopy and with suction, advance the catheter slowly across the lesion into the periphery and then retract it.
Under fluoroscopy and with suction, advance the catheter slowly across the lesion into the periphery and then retract it.
 If the syringe is full, lock the stopcock, unscrew the syringe, and empty through the filter.
If the syringe is full, lock the stopcock, unscrew the syringe, and empty through the filter.
 Repeat the aspiration procedure.
Repeat the aspiration procedure.
 Concomitant administration of a GP IIb/IIIa inhibitor is usual.
Concomitant administration of a GP IIb/IIIa inhibitor is usual.
 Summary and Evaluation
Summary and Evaluation
Disadvantages:
 It is often not possible to aspirate older thrombi.
It is often not possible to aspirate older thrombi.
 In small vessels the systems are often not efficacious as they become attached to the vessel wall.
In small vessels the systems are often not efficacious as they become attached to the vessel wall.
 If the catheter is advanced too quickly, material can be pushed to the periphery.
If the catheter is advanced too quickly, material can be pushed to the periphery.
 If the internal diameter is too small, it is often not possible to record a pressure curve when the aspiration catheter is in the guiding catheter; therefore, when in doubt use a 7F guiding catheter.
If the internal diameter is too small, it is often not possible to record a pressure curve when the aspiration catheter is in the guiding catheter; therefore, when in doubt use a 7F guiding catheter.
Advantages:
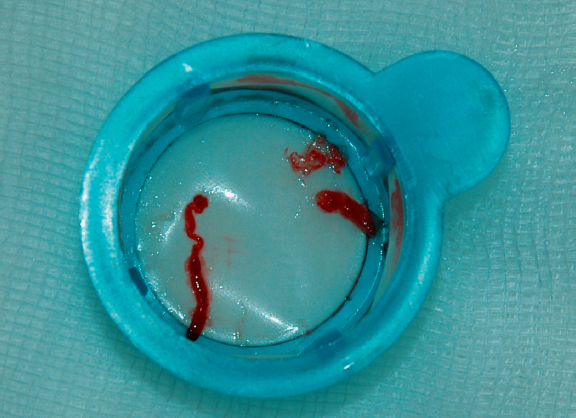
 For fresh thrombi and atheromas this is a very efficacious, fast, and uncomplicated intervention (Fig. 27.2).
For fresh thrombi and atheromas this is a very efficacious, fast, and uncomplicated intervention (Fig. 27.2).
 Clinical studies have shown that aspiration catheters improve the perfusion in acute coronary syndromes.
Clinical studies have shown that aspiration catheters improve the perfusion in acute coronary syndromes.
Mechanical Thrombectomy
 Basics
Basics
 Indications and Contraindications
Indications and Contraindications
 Severe calcifications
Severe calcifications
 Significant residual stenoses
Significant residual stenoses
 Very tortuous vessels
Very tortuous vessels
 Small vessels (< 2.5 mm)
Small vessels (< 2.5 mm)
 Visible dissection
Visible dissection
 Materials
Materials
 Procedure
Procedure
Preparation of the System
 Connect saline to the designated line.
Connect saline to the designated line.
 Connect the power cable.
Connect the power cable.
 Flush the system and remove any air.
Flush the system and remove any air.
 Place the catheter tip in a saline bath and switch on the system at the control unit for an extracorporeal test run.
Place the catheter tip in a saline bath and switch on the system at the control unit for an extracorporeal test run.
Procedure for Thrombectomy
 Use only if the vessel diameter is > 2.5 mm.
Use only if the vessel diameter is > 2.5 mm.
 The guiding catheter is seated. Then, the thrombus is crossed with the guidewire, and the wire tip is positioned as distally as possible.
The guiding catheter is seated. Then, the thrombus is crossed with the guidewire, and the wire tip is positioned as distally as possible.
 The catheter is advanced up to the end of the guiding catheter.
The catheter is advanced up to the end of the guiding catheter.
 After switching on the drive unit and opening the flush solution, the catheter is advanced through the lesion carefully and very slowly (~1 cm/5 seconds).
After switching on the drive unit and opening the flush solution, the catheter is advanced through the lesion carefully and very slowly (~1 cm/5 seconds).
 The procedure is repeated several times.
The procedure is repeated several times.
 The system should be moved within the vessel only with the system running, if possible.
The system should be moved within the vessel only with the system running, if possible.
 Withdraw the catheter into the guiding catheter and angiographically evaluate the procedure’s success.
Withdraw the catheter into the guiding catheter and angiographically evaluate the procedure’s success.
 Summary and Evaluation
Summary and Evaluation
X-Sizer
 Basics
Basics
 Indications and Contraindications
Indications and Contraindications
 Degenerated vein grafts with intervention-induced thrombotic occlusion
Degenerated vein grafts with intervention-induced thrombotic occlusion
 Large intracoronary thrombus burden in the setting of an acute myocardial infarction
Large intracoronary thrombus burden in the setting of an acute myocardial infarction
 Complete, nonacute, thrombotic vessel occlusion
Complete, nonacute, thrombotic vessel occlusion
 Indications for atherectomy
Indications for atherectomy
 Extensive, untreated dissections
Extensive, untreated dissections
 Materials
Materials
 Procedure
Procedure
Preparation of the System
 Removal of the lock wire from the control module
Removal of the lock wire from the control module
 Flushing of the system with heparinized saline
Flushing of the system with heparinized saline
 Connection to the vacuum collecting bottle after occluding the tubing clamp
Connection to the vacuum collecting bottle after occluding the tubing clamp
 The system is held under water and the tubing clamp is opened to test whether the catheter is aspirating; then the tubing is clamped again and kept occluded until the system has been deployed.
The system is held under water and the tubing clamp is opened to test whether the catheter is aspirating; then the tubing is clamped again and kept occluded until the system has been deployed.
Procedure of Thrombectomy
 Premedicate with heparin and a GP IIb/IIIa inhibitor.
Premedicate with heparin and a GP IIb/IIIa inhibitor.
 Place the guiding catheter.
Place the guiding catheter.
 The lesion is crossed with a 300 cm long 0.014-in. guidewire.
The lesion is crossed with a 300 cm long 0.014-in. guidewire.
 Advance the system via the wire to the distal end of the catheter and carefully position it before the lesion or occlusion.
Advance the system via the wire to the distal end of the catheter and carefully position it before the lesion or occlusion.
 Open the clamp that occludes the tubing to the vacuum collection bottle.
Open the clamp that occludes the tubing to the vacuum collection bottle.
 After switching on the drive unit, advance the catheter very slowly (≤ 1 mm/s) across the entire lesion.
After switching on the drive unit, advance the catheter very slowly (≤ 1 mm/s) across the entire lesion.
 Avoid known dissections.
Avoid known dissections.
 Ablated material and blood appear in the vacuum bottle.
Ablated material and blood appear in the vacuum bottle.
 Never stop the cutting process inside the lesion, and never leave the cutter inside the lesion.
Never stop the cutting process inside the lesion, and never leave the cutter inside the lesion.
 Repeat the cutting procedure several times.
Repeat the cutting procedure several times.
 Withdraw the X-Sizer catheter in the guiding catheter and undertake angiographic evaluation of the procedural success.
Withdraw the X-Sizer catheter in the guiding catheter and undertake angiographic evaluation of the procedural success.
 Summary and Evaluation
Summary and Evaluation
Disadvantages:
 A stiff catheter tip with little flexibility
A stiff catheter tip with little flexibility
 Risk of aspiration of dissection tissue
Risk of aspiration of dissection tissue
 High cost
High cost
Advantages:
 Standard guiding catheters and guidewires can be used.
Standard guiding catheters and guidewires can be used.
 The system is technically easier than the AngioJet catheter (see below)—no special drive console, etc. is required.
The system is technically easier than the AngioJet catheter (see below)—no special drive console, etc. is required.
AngioJet
 Basics
Basics
 Indications and Contraindications
Indications and Contraindications
 Coronary thrombi (filling defects) on angiography in unstable angina, acute infarction, or occluded vein graft
Coronary thrombi (filling defects) on angiography in unstable angina, acute infarction, or occluded vein graft
 Thrombotic stent occlusion
Thrombotic stent occlusion
 Atherectomy indications
Atherectomy indications
 Extensive, untreated dissections
Extensive, untreated dissections
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



 Screw on the aspiration syringe with the stopcock in the locked position, apply suction, and lock the syringe.
Screw on the aspiration syringe with the stopcock in the locked position, apply suction, and lock the syringe.