CHAPTER 7 Thoracic Trauma
The earliest recorded reference to thoracic trauma is found in the Edwin Smith Surgical Papyrus written around 3000 BC.1 In this report of 58 cases, three were related to the chest: a penetrating injury to the cervical esophagus, a stab wound to the sternum, and blunt trauma resulting in rib fractures. During the Trojan war, Homer reported on many thoracic injuries in his Iliad, perhaps the most famous of which was that of King Agamemnon, who slayed Odius during the Battle of Troy with a well-placed spear through his chest.2 At the start of the common era, there are descriptions of fatal thoracic injuries suffered by the ancient Olympians in their often more violent version of the familiar games, as well as those suffered by the Gladiators and depicted by Galen.3,4 Many of these injuries were the focus of art in the ancient world (Fig. 7-1).5 More recent was the assassination attempt of President Ronald Reagan by John Hinkley in 1981; a bullet struck the president in his left chest, causing a nonfatal hemothorax (Fig. 7-2).6,7 In the most recent conflicts in Afghanistan and the Middle East, Operation Enduring Freedom and Operation Iraqi Freedom, respectively, thoracic trauma was responsible for one quarter of on-battlefield deaths and represented up to 20% of all battlefield injuries.8–10
Through the eras of Hippocrates and Galen, open packing and local treatment with common ingredients (red meat, honey, lint) was the mainstay of treatment, until the 13th century when wound débridement and closure was advocated. However, wound closure became a topic of great debate, although it was somewhat clarified by Paré in 1514. He advocated immediate closure of wounds without blood (or with only a small amount) in the chest; enlarging of small wounds if better drainage of blood were required; and delaying wound closure until blood drainage had ceased (usually 2 to 4 days).11 During the next century, various cannulas were developed to irrigate infected wounds and empyemas, which eventually evolved into the closed drainage systems used during World War II.
Mortality from chest wounds progressively decreased from a wartime high of 80% to 90% during the Civil War, as reported by Billings,12 to 4% to 7% in recent civilian experience. Nevertheless, thoracic trauma accounts for 25% of all trauma deaths, representing approximately 160,000 deaths annually.13 Over 70% of thoracic injuries result from blunt trauma, and most occur in automobile accidents. One in four patients with cardiothoracic trauma regardless of etiology requires hospital admission.
THE PRIMARY SURVEY
The standard resuscitation of the trauma patient has been outlined by the American College of Surgeons in the Advanced Trauma Life Support (ATLS) guidelines.14 When the patient arrives in the trauma bay, a primary survey is rapidly performed. The ABC algorithm is followed so that potentially life-threatening injuries can be recognized before they become lethal: the airway is controlled, then breathing is assessed and assisted with mechanical ventilation if necessary, and third, circulation is supported by establishing reliable, large-bore venous access and initiating fluid resuscitation. Finally, the patient’s neurologic disabilities are assessed, and the entire body is exposed to identify any significant deformities or penetrating injuries that might otherwise have been overlooked. The goal of the primary survey is to identify immediate, life-threatening injuries that could account for ventilation or hemodynamic instabilities that, if left uncorrected, could cause the acute demise of the patient.15
Injuries to the thoracic cavity or its contents comprise the majority of this group, and they generally require urgent intervention as a life-saving measure (Table 7-1). These problems should always be kept in mind during the resuscitation of every trauma patient. The mechanism of injury should also influence the index of suspicion for these injuries, as some are more likely to be sequelae of blunt trauma (aortic rupture, diaphragmatic hernia, cardiac tamponade), penetrating trauma (cardiac tamponade, massive intrathoracic hemorrhage), or common to both (pneumothorax).
Table 7–1 Potentially Acutely Lethal Injuries of the Chest and Their Management
| Injury | Management |
|---|---|
| Tension pneumothorax | Tube thoracostomy |
| Massive intrathoracic hemorrhage | Tube thoracostomy, operative repair |
| Cardiac tamponade | Pericardiocentesis, operative repair |
| Deceleration aortic injury | Operative repair |
| Massive flail chest with pulmonary contusion | Intubation, pain control, fluid restriction |
| Upper or lower airway obstruction | Intubation, airway, bronchoscopy |
| Tracheobronchial rupture | Bronchoscopy, operative repair |
| Diaphragmatic rupture with visceral herniation | Operative repair |
| Esophageal perforation | Operative repair |
DIAGNOSTIC TESTS
Approximately a third of all deaths from thoracic trauma occur immediately on or shortly after the patient’s arrival at a treatment facility. Diagnostic and emergency management modalities are essential to fully evaluate these injuries and direct care toward the proper therapeutic interventions.16
Chest Radiography
CT of the chest has been shown to be more sensitive than plain radiography in detecting thoracic injuries such as pulmonary contusions, hemothorax, and pneumothorax.17,18 Up to 75% of trauma patients with a normal physical examination and chest radiograph will have an occult injury diagnosed on chest CT, and 5% of these patients will need intervention for their injuries.19,20 Even when evidence of thoracic trauma is seen on physical examination and plain radiography, the addition of chest CT leads to altered management and therapeutic decisions in up to a third of all patients with thoracic injuries.18,19 In addition, chest CT can be used to exclude diagnoses made by the less sensitive chest radiograph, which can happen in up to 15% of patients.19
Ultrasonography
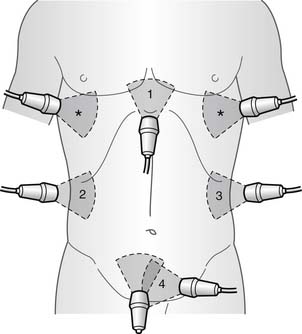
Ultrasonography has now become fairly routine in the early evaluation of the abdomen and pericardium.21 The focused assessment for the sonographic evaluation of the trauma patient, or FAST examination, four standard viewing ports are used to quickly access for abnormal fluid collection: right upper quadrant, left upper quadrant, pelvis, and subxiphoid. In addition, the extended (E)-FAST, which uses an extension of the right and left upper quadrant views to include the right and left hemithoraces (right and left longitudinal thoracic views), respectively, can aid in the diagnosis of hemothorax or pneumothorax (Fig. 7-3).22,23 Although not as precise as an ultrasound performed by a board-certified radiologist or cardiologist, this examination is able to detect fluid collections that might influence the need for urgent operative intervention. Of the four views, the subxiphoid view is the most accurate in the hands of surgeons for detecting abnormalities in the trauma setting.21 It is safe, expeditious, repeatable, and effective even in the hands of surgeons from different specialties24 and can be useful to identify injuries to the heart, and fluid in the pericardium.
Echocardiography
A major shift in the diagnosis of aortic and great vessel injuries has occurred in recent times.25 In the 1990s and before, these injuries were diagnosed almost exclusively by aortic angiography or transesophageal echocardiography (TEE). Since the late 1990s, CT angiography (CTA) has become the most prevalent diagnostic modality in this patient population, with only a small percentage of patients undergoing conventional angiography or TEE. In two large trauma-center reviews, CTA was found to be 90% to 95% sensitive and to have a 99% to 100% negative predictive value, making it very useful as a screening modality.26,27 Meta-analyses of smaller case series from the literature since the late 1980s appear to support these conclusions, with sensitivity and negative predictive values approaching 100%.26
Cited reasons for the shift in diagnostic modalities include technical improvements in the quality of CT angiograms with the addition of multirow detector CT techniques to the standard helical CT, the relative ease of performing the test, reliable interpretations of rapidly obtained results, cheaper cost to perform the test, ability to perform real-time three-dimensional (3D) reconstructions, and the ubiquitous nature of CT machines in emergency departments across the nation. CT angiography can be performed at the same time as the common whole-body CT scan that many trauma patients undergo as part of their routine workup. Furthermore, the level of detail achieved with CT aortography far exceeds that from conventional aortography, allowing the radiologist and the surgeon to identify even the most subtle of aortic injuries that may have been missed on conventional aortography. Large case series have identified CT aortography as an appropriate modality for screening, diagnosing, and planning operative repair of aortic injuries.27
Angiography
Conventional angiography was once the gold standard in the diagnosis of aortic transection or injuries to the great vessels (Fig. 7-4).28 In aortic transection, the classic aortographic image displays a pseudoaneurysm near the site of the isthmus. Partial or complete interruption of the aortic contour may be seen when the aortic wall has retracted, or if debris of the wall prolapses into the lumen. Occasionally, a ductus diverticulum, a normal finding at the site of the uninterrupted intimal surface, is seen at the site of the ligamentum arteriosum.29
The present role of conventional arteriography is unclear, as many centers now use highly detailed 3D aortic reconstructions alone for diagnosis and operative planning (Fig. 7-5). Others obtain a conventional aortogram if the results of the CT angiogram are equivocal or if the study was technically inadequate. Still others routinely obtain conventional arteriograms to confirm the presence of an aortic injury prior to surgical intervention.30 When performed, a retrograde femoral arteriogram is the preferred study. Generally agreed on indications for aortography in these patients, by either conventional methods or CT angiography, are listed in Box 7-1.
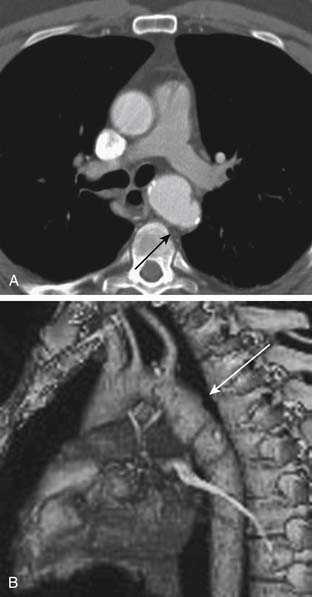
(From Steenburg SD, Ravenel JG, Ikonomidis JS, Schonholz C, Reeves S. Radiology 2008;248[3]:748-62.)
Box 7–1 Indications for Angiographic Studies for Potential Thoracic Injuries
In fact, use of conventional aortography to further evaluate patients whose CT angiogram has been read as indeterminate is unlikely to aid in a diagnosis of any aortic or other great vessel injuries and thus may no longer be part of the evaluation of these patients.31 Thus, some have argued that the role of conventional angiography is limited to those centers that do not have adequate multidetector CT scanners with software for 3D reconstruction and an available radiologist for interpretation, for cases where artifact from air or metallic objects precludes adequate imaging, or for cases where angiography is used to direct therapy (e.g., embolization of smaller arteries).16
The presence of a mediastinal hematoma is often the first manifestation of an aortic injury seen on CTA.32 It is important, however, to note the exact location of this hematoma, as hematoma outside of the aortic walls with preservation of the fat plane around the aorta does not represent an aortic injury but rather, usually, damage to surrounding periaortic mediastinal vasculature. If the hematoma extends from a point adjacent to the aortic wall, a true aortic injury can be suspected, and careful examination of the remainder of the thoracic CTA is important. Rarely is active extravasation of contrast material into the mediastinum or thorax seen, as this type of injury is almost always uniformly fatal.
EMERGENCY DEPARTMENT THORACOTOMY
The indications for emergency department (ED) thoracotomy have been widely debated.33 ED thoracotomy clearly plays a role in the case of penetrating thoracic trauma, particularly for trauma patients with cardiac tamponade from penetrating chest injuries.34 There is a very limited role for patients with blunt traumatic injuries, the only accepted indication being the patient who arrives with vital signs and suffers a traumatic arrest in the trauma bay.
Thoracotomy allows relief of cardiac tamponade, the ability to perform open cardiac massage, and control of ongoing intrathoracic hemorrhage. In addition, by applying a crossclamp to the thoracic aorta, one can limit intra-abdominal bleeding and improve cerebral and coronary perfusion in the setting of exsanguinating hemorrhage. Patients with penetrating cardiac stab wounds and other penetrating cardiac injuries are the most likely to survive resuscitation with ED thoracotomy. The likelihood of patient survival depends on patient downtime, the patient’s age and comorbidities, and signs of life on arrival to the ED. General guidelines have been recommended for ED thoracotomies by the American College of Surgeons’ Committee on Trauma in the setting of thoracic trauma (Box 7-2).35
Box 7–2 Indications and Contraindications for Emergency Room Thoracotomy
Accepted Indications
Relative Indications
Although these general guidelines have been debated, most agree that the best results occur in patients with penetrating cardiac trauma and in whom there is a good likelihood for cerebral activity. Even with an experienced team and established protocols, results are still poor. The length of time cardiopulmonary resuscitation (CPR) was performed before the patient reached the hospital has become one of the determinants for whether to perform ED thoracotomy. In one report, there were no survivors from ED thoracotomy when prehospital CPR had been in progress in an intubated patient for more than 10 minutes, or more than 5 minutes in an unintubated patient.36 Another marker of relatively poor outcome is refractory metabolic acidosis monitored during the initial resuscitation efforts, with a pH of less than 6.8 or severe base deficits restraining the use of ED thoracotomy.
Even with these extraordinary efforts on the part of the ED trauma team, the results from ED thoracotomy are dismal, with overall survival rates of 1.8% to 27.5%.33 Although the survival rates of patients who undergo ED thoracotomy varies substantially between case series, mechanism of injury is the most important factor affecting mortality, and patients suffering penetrating injuries are more likely to benefit from this procedure, with mean survival rates of 13% (range, 2.7% to 38.9%) compared with a mean of 1% (range, 0% to 12%) for patients who presented with blunt injuries. Even among those who survive their injuries after ED thoracotomy, up to half will have some neurologic deficit, although some authors have reported that over 90% of patients regain neurologic function in their series.
BLUNT TRAUMA
Blunt trauma to the chest in the United States is far more common than penetrating injury. A 2002 report by the National Safety Council reported that of all blunt trauma deaths, 25% resulted from thoracic trauma. The high-speed deceleration and crush injuries involved in automobile accidents have become increasingly prevalent since the 1950s and account for the majority of blunt thoracic trauma. Falls, sports mishaps, assaults, and blast injuries follow. The damage from a powerful blast can be particularly severe, as the blast pressure wave imparts a large amount of kinetic energy to a small area. Blast kinetic energy especially affects gas-containing organs, such as the lung, resulting in pulmonary hemorrhage, hypoxia, and shock. In addition, because of the mechanisms that provide the amount of energy needed to produce significant blunt thoracic trauma, many of these patients will have associated head, abdominal, or extremity injuries along with those of the thorax (as presented here).37 Nevertheless, even in this multiply injured population, the thoracic injuries are responsible for the majority of mortality.38
Chest Wall
Optimal mechanical properties of the chest wall are important determinants for effective functioning of the entire respiratory system. Blunt trauma to the chest wall can disrupt respiratory mechanics and lead to poor pulmonary toilet and significant morbidity. Chest wall trauma alone occurs in only 16% of cases39 and is more often a marker of more ominous visceral injury in the thoracic cage or below the diaphragm. Because the chest wall provides a protective bony skeleton (ribs, sternum, clavicles, and scapulas) around the vital organs of the chest, the impact of fracturing each of these bones will be considered.
Rib Fractures
Fracture of the ribs is the most common blunt thoracic injury, occurring in an estimated 300,000 people in the United States during 2000, or 39% of patients admitted to major trauma centers.40,41 Rib fractures are an important indicator of trauma severity. The greater the number of ribs fractured, the higher is the patient’s morbidity and mortality, even from nonpulmonary causes, especially if six or more ribs are broken.42,43 The number of ribs fractured has been significantly correlated with the presence of hemothorax or pneumothorax, with 81% of patients having either condition if two or more ribs were fractured.44 Fractures of the fourth through the ninth rib are associated with injuries to the lung, bronchus, pleura, and heart, whereas fractures below the ninth rib are indicative of spleen, hepatic, or renal injuries.
The main symptoms include pain, exquisite tenderness, and possibly crepitus. In the initial examination, an upright chest radiograph is performed as a routine part of the trauma series. In the event that special documentation of a crime, such as child abuse, is needed, rib detail films are obtained. Chest radiograph alone fails to diagnose rib fractures in over half of trauma patients with fractures, and the addition of CT to the trauma evaluation improves the sensitivity of the diagnosis of rib fractures.45 Careless dismissal of a simple rib fracture and underestimating its pathophysiologic potential, especially in the elderly patient, is a common management pitfall. After adjusting for severity of injury, comorbidity, and the presence of multiple rib fractures, elderly patients (≥65 years old) with simple rib fractures still were five times more likely to die than those younger than 65.46 The first rib fracture has particular significance because of the great force required for it to occur and the likelihood that intrathoracic visceral injury has also taken place. The two most common sites of first rib fractures are at the subclavian sulcus and in the neck of the first rib posteriorly. Subclavian artery or aortic arch angiography (conventional or CTA) is indicated, or both can be done, if the first rib fracture is displaced posteriorly, if the subclavian groove is fractured anteriorly, or if there is widened mediastinum on chest radiograph, an upper extremity pulse deficit, a concomitant brachial plexus injury, or an expanding hematoma.47
Although binders, cumbersome rib belts, and taping were advocated in the past, the modern approach to treatment emphasizes relief of pain, prevention of atelectasis, and optimization of pulmonary toilet. The importance of adequate analgesia to proper pulmonary toilet is evident by studies showing decreased mortality among patients with rib fractures who received epidural anesthesia.43 A prospective case series at a level 1 trauma center found that patients with isolated, simple rib fractures suffered an average of more than 50 days of disability and lost work or usual activity because of pain.40 Interventions favored for short-term pain relief include epidural analgesia, intercostal rib blocks, intrapleural instillation of anesthesia, and intravenous opiates as well as oral nonsteroidal anti-inflammatory drugs (NSAIDs).40,48–50 Chronic pain control is invariably required, usually with oral narcotics, NSAIDs, and transdermal patches. Patients must be reminded to practice adequate pulmonary toilet after discharge by using an incentive spirometer, deep breathing, coughing, and ambulation. Patients should be counseled that their pain will probably continue for weeks, and that sustained need for oral analgesics during this time is not uncommon. In addition to chronic pain, other long-term sequelae include chest wall deformities, persistent dyspnea, and neurologic deficits. A relatively uncommon but potential long-term complication of severe blunt trauma is a thoracic lung hernia. Because these entities pose a constant threat of incarceration, pneumothorax, or strangulation, they should be repaired.51
Flail Chest
During the primary survey of a patient who has suffered blunt trauma, careful observation for the presence of a flail chest is imperative because of the associated pathophysiologic derangements that accompany this finding.52 This injury usually occurs with the fracture of four or more ribs at two sites, either unilateral or bilateral, promoting enough instability that the thoracic cage exhibits paradoxical motion locally. This impairs respiratory mechanics and results in hypoventilation, poor pulmonary drainage, and atelectasis. Patients with flail chest are distinct from those with multiple rib fractures as they are at a higher risk of respiratory compromise and often require early intubation.53 Endotracheal intubation is required in more than two thirds of patients with flail chest and is indicated for a respiratory rate of more than 40 breaths per minute, or a PO2 of less than 60 mm Hg despite 60% face mask oxygen. Relative indications for intubation include shallow respirations, depressed consciousness, preexisting chronic lung disease, or the presence of associated injuries. In the presence of multiple injuries, intubation of the patient with a flail chest is almost unavoidable, and early controlled intervention often obviates sudden respiratory decompensation and its subsequent morbidity.53
A flail chest is invariably caused when the thoracic cage absorbs high kinetic energy, and thus it is an important marker for significant intrathoracic injury in the patient with blunt trauma. It is highly associated with pulmonary contusion, which occurs in about 45% of these patients.54 Pneumothorax or hemothorax is a common acute sequela, and acute respiratory distress syndrome (ARDS) occurs in as many as a third of these patients and results in mortality rates as high as 33%.54
Conservative therapy with emphasis on pain relief with thoracic epidural analgesia is the mainstay of therapy in most centers. In a minority of cases, however, patients require chest wall stabilization (Fig. 7-6).55,56 These commonly are intubated patients with no possibility of being weaned from the ventilator because of a large unstable flail segment of chest wall.
Sternal Fractures
Isolated fractures of the sternum are seen with increasing frequency in motor vehicle accidents, particularly since the passing of the mandatory seatbelt legislation, because of the rapid deceleration that occurs from this mechanism of injury, especially in vehicles with absent or malfunctioning airbags.57 Point tenderness, edema, and obvious deformity are occasionally detected on physical examination, but a lateral chest radiograph is diagnostic in the majority of patients.
Morbidity and mortality from isolated sternal fractures is low, and surgical repair is uncommon (<2%). Some have suggested that patients with isolated sternal fractures, a normal echocardiogram, and no elevation of cardiac enzymes in the early hours of injury will have a benign course. They advocate discharging these patients home within 24 hours of arrival in the ED.58 Still others support selective repair for those with severe deformities or associated chest wall fractures, as this procedure can be performed with low mortality and morbidity and with good outcomes.59 Surgical management options include metal plates with or without autologous bone grafts.60,61 Although an isolated sternal fracture carries a favorable prognosis, other life-threatening concomitant injuries occur in up to a third of patients, necessitating careful evaluation and clinical vigilance.
Clavicular Fractures
Because the clavicles are thin and exposed, the mid-clavicular shaft, in particular, is often fractured, and this occurs in three of four patients with clavicular fractures.62 One of four patients fractures the acromial part of their clavicle. Right and left clavicles tend to be fractured with equal frequencies. Clinical examination reveals tenderness, deformity, crepitus, and occasionally upper extremity neurovascular injury. Routine chest radiographs often demonstrate the diagnosis. Conservative treatment for pain control using closed reduction and figure-eight slings heals 95% of patients. Surgical techniques include placement of steel reconstruction plates and cannulated bone screws. Late sequelae of clavicular fractures include painful nonunions, altered shoulder mechanics, neurogenic thoracic outlet syndrome, vascular abnormalities, and brachial plexus injuries. Contributing factors to nonunion include severe initial trauma, open fracture, marked initial displacement and shortening, soft tissue interposition, primary open reduction and internal fixation, refracture, multiple trauma, and inadequate initial mobilization.63
Scapular Fracture
Because the scapula is thick and well protected, scapular fractures are relatively rare and usually occur only after high-kinetic-energy impacts. In fact, many patients with scapular fractures have other serious injuries to other anatomic sites because of the severe mechanism of energy needed to produce this injury.64 Still, scapular fractures should always be in the differential diagnosis in any patient who complains of shoulder pain or violent muscular contractions about the shoulder after blunt trauma. Most fractures occur in the neck and body, with glenoid, acromion, and coracoid process injuries being less frequent. As is the case with other thoracic cage trauma caused by severe blunt trauma, associated pulmonary contusions and rib fractures are common. Diagnosis is often difficult on physical examination, occasionally identified by localized tenderness, swelling, and hematoma formation over the fracture site. Scapular fractures are often overlooked on supine chest radiographs, and the three-view trauma series of the shoulder is often necessary to reveal the fracture. Chest CT scans are not recommended.
Traumatic Asphyxia
Traumatic asphyxia is an uncommon clinical syndrome usually occurring after a severe crushing or compression-related injury to the chest. Symptoms and associated physical findings include subconjunctival hemorrhage, cervicofacial cyanosis resulting in a purple-blue discoloration of the neck and face, facial edema, vascular engorgement of the head, mucosal petechiae, and multiple ecchymotic hemorrhages of the face, neck, and upper chest. Cerebral hypoxia resulting from hypoventilation is an ever-present danger that results in varying degrees of cerebral dysfunction. Sore throat, hoarseness, dizziness, numbness, and headaches are common. Pitting lower extremity edema, hemoptysis, hemotympanum, hematuria, rectal bleeding, and transient visual loss may also be evident.65 The diagnosis is made primarily from the history and physical examination. Chest radiographs are usually normal.
Pulmonary Contusion
The lung parenchyma fills a large portion of the chest cavity and lies very close to the bony thorax, making it vulnerable to contusion. In fact, pulmonary contusion is the most common injury in blunt chest trauma.52 The mechanism of injury usually involves a sudden deceleration injury such as in a motor vehicle accident with the chest hitting the steering wheel, or in a blast injury or a fall from a great height. Although pulmonary contusions are generally associated with concomitant thoracic cage damage and other visceral injuries, they can be isolated and without evidence of rib fracture. Wagner and colleagues have suggested that the pathophysiology of a pulmonary contusion is based on hemorrhage into adjacent alveolar spaces rather than injury to the alveolar capillary wall itself.66
As mentioned, patients with pulmonary contusions are at a high risk of respiratory insufficiency and secondary pneumonia because of the parenchymal damage and large systemic inflammatory response that accompanies this injury. The formation of a pulmonary contusion along with an injury severity score of greater than 65 has been identified as the risk factor that has the greatest contribution to the development of ARDS.67 The mortality rate from an isolated pulmonary contusion is low, but when combined with other severe injuries, it rises to as high as 50%.68 Clinical factors predisposing to mortality after a pulmonary contusion include patient age, resuscitation volume, and severity of the pulmonary parenchymal injury as measured by the ratio of PaO2 to fraction of inspired oxygen (FiO2) at 24 and 48 hours after the injury.69
Laryngeal Injuries
The larynx enjoys a position of relative protection in the neck, shielded laterally by the sternocleidomastoid, posteriorly by the cervical spine, and from the front and above by the mandible. Blunt trauma to the larynx is therefore rare, but its mortality rate reaches as high as 40%, with most patients dying from the injury at the trauma scene.70 Death is caused primarily by asphyxia from laryngospasm, hemorrhage from an associated major vascular laceration, or laryngeal concussion. Laryngeal trauma is suspected after motor vehicle accidents, hanging attempts, sporting blows such as in karate or soccer, and severe falls.
Tracheobronchial Injuries
Tracheobronchial injuries are uncommon, but they occur usually after high-energy impact and are associated with trauma to other vital organs.71 According to an extensive review of all published tracheobronchial injuries since 1873, 59% of these injuries were found to be caused by motor vehicle accidents, 76% occurred within 2 cm of the main carina, and 43% were located within 2 cm of the right main bronchus.72 Three potential mechanisms of blunt tracheobronchial disruption have been identified. The first and most common is a forceful anteroposterior compression of the thoracic cage, the so-called dashboard injury, where an unrestrained automobile occupant hyperextends the neck, striking it on the dashboard or steering wheel and producing a crushing injury of the cervical trachea. The second mechanism is a consequence of high airway pressures, and the third is a rapid deceleration. The typical clinical features include respiratory distress, dyspnea, and air leak. Hoarseness or dysphonia is also common, occurring in up to 45% in some series. Persistence of an undiagnosed air leak is life-threatening and may lead to hypoventilation and, ultimately, respiratory insufficiency. On physical examination, the most common diagnostic signs are subcutaneous emphysema (35% to 85%), pneumothorax (20% to 50%), and hemoptysis (14% to 25%).
The definitive diagnostic study of choice is a flexible bronchoscopy. A careful bronchoscopic examination includes an inspection of the tracheobronchial tree, documenting the site and extent of injury, including a withdrawal of the endotracheal tube in an intubated patient to diagnose proximal tracheal tears. A high level of suspicion is imperative for diagnosis, becausee occasionally patients with tracheobronchial injuries present with normal clinical appearance and negative endoscopic findings. In fact, often the diagnosis of tracheobronchial injury is delayed, and the repair is performed months and even years after the initial injury.72 In that study, no statistically significant association was found between delay in treatment and successful repair of the injury, with 90% of patients undergoing successful surgical reconstruction more than 1 year after initial injury.
Great Vessels
The thoracic great vessels consist of the aorta and its major intrathoracic branches, the pulmonary arteries and veins, the venae cavae, and the azygous vein. By far the most lethal injury to any of these is descending aortic injury, which accounts for as many as 40% of fatalities after blunt thoracic trauma, with the majority of deaths at the trauma scene.73 Most of these deaths result from free intrapleural aortic rupture before surgical repair. The site of injury is usually the medial descending aorta at the ligamentum arteriosum, where shear forces caused by rapid deceleration result in a tear at this point of fixation of the vasculature. Again, a high index of suspicion in a patient who has suffered a high-speed collision is critical, because about half of the patients with contained aortic rupture have no external signs of trauma.74
A plain chest film has a 95% negative predictive value for identifying blunt traumatic aortic lesions, so it is an adequate diagnostic screening study.75 The classic signs on plain chest radiograph (Fig. 7-7) as described by Kirsch and Sloan include a widened mediastinum (>10 cm), loss of aortic knob contour, shift of the endotracheal tube and the trachea to the right, elevation of the left main-stem bronchus, depression of the right main-stem bronchus, shift of the nasogastric tube to the left, apical capping, first rib fracture, acute left-sided hemothorax, and a retrocardiac density. Of these, the finding that most reliably correlates with an aortic tear is loss of aortic knob contour. Spiral-CT scanning with angiography, which has 96.2% sensitivity and 99.8% specificity for blunt traumatic aortic abnormalities, as well as wide availability, has become the preferred confirmatory study in the algorithm of blunt aortic injury for hemodynamically stable trauma patients. Conventional biplane contrast aortography should be considered despite previous negative studies if the clinical suspicion remains high, as it is suggested that 2% of patients with great vessel injuries have this scenario.76 Those patients with an obviously widened mediastinum on radiograph, along with hypotension and hemothorax, are at high risk for imminent rupture of a contained aortic injury and may be taken to the operating room without delaying for further confirmatory studies.77
Once a contained, aortic rupture is diagnosed, urgent management is required. Specifically, invasive monitoring and careful blood pressure and heart rate control with intravenous beta-blockade followed by nitroprusside are indicated as a first step. A thorough neurologic examination to document any preoperative deficits is vital. If other life-threatening injuries, such as intra-abdominal bleeding, are detected in the primary or secondary survey, these are repaired first before the thoracic aortic injuries are addressed. If there is little time for preoperative studies, a TEE can even be performed during laparotomy to identify signs of blunt traumatic aortic injury. Since the mid 1990s, the four most dramatic changes in management of these patients have been nonoperative management, delay to definitive treatment, use of endovascular stenting for repair, and the increasing use of left heart bypass via centrifugal pumps in the operating room.76
A subset of patients with contained aortic rupture, including those with severe central nervous system injury, extensive burns, hemodynamic instability from other traumatic injuries, respiratory failure, or small intimal defects, are appropriately managed either nonoperatively or with a delayed operation.78 Mean arterial pressure should be maintained near 60 to 70 mm Hg in a manner similar to that used for patients who have suffered an acute dissection of the descending thoracic aorta.76 Although the length of time necessary for rigorous antihypertensive therapy is unknown, reports in a small series of patients followed serially by TEE have shown that complete resolution of small (<20 mm) injuries occurs in about 9 days (range, 3 to 19 days).79
Since 1991 when the first endovascular stenting of the aorta was performed for an abdominal aortic aneurysm, interest in stent grafting as an alternative to traditional aortic surgery has surged. Preliminary experience is now accumulating from percutaneous positioning of endovascular stent grafts under angiographic guidance for blunt traumatic aortic lesions.80–83 An analysis of the available data has demonstrated this to be an safe and effective procedure.83 This procedure has excellent technical success rates, averaging 96.3%, with endo-leak rates of 5.1%, while maintaining low rates of complication, including overall and graft-related mortalities of 7.7% and 2%, respectively, and a 1.1% rate of paraplegia. Similar analyses of open repairs have demonstrated worse outcomes, with mean mortality of 14.7% and a 3.3% rate of paraplegia. In addition, length of hospital stay, transfusion requirement, and need for additional surgical procedures have been shown to be lower among patients who undergo percutaneous stenting compared with open repair of traumatic aortic injuries.84 As the technology progresses and the grafts and their delivery systems become easier to employ, long-term studies, including randomized, prospective trials evaluating the durability and efficacy of this approach, will be warranted.
The open surgical approach is via a fourth interspace left posterolateral thoracotomy. Proximal and distal control is obtained with care taken to avoid injury of the recurrent laryngeal and vagus nerves as well as the thoracic duct. There has been considerable controversy for more than 2 decades between proponents of the use of “clamp and sew” techniques versus unloading the heart proximally and shunting the blood distally. Traditional arguments against the use of left heart bypass via passive shunts included the need to heparinize a trauma patient with associated injuries and the lack of data showing decreased neurologic injury with passive shunting. Convincing evidence is accumulating, however, demonstrating the benefits of left atrial to femoral shunting via a centrifugal pump. Many of these systems do not require heparin, and there is growing evidence of low rates of paraplegia and mortality.85–87 Although prolonged clamp times and the increasing complexity of the repair are associated with rising paraplegia rates, another important predictor of paraplegia has been the occurrence of upper body hypotension during surgery. Left atrial to femoral shunting during and immediately after clamping of the aorta allows strict control of upper body blood pressure. In fact, a review of a 30-year experience of blunt traumatic aortic rupture noted the gradual evolution in clinical surgical technique from clamp-and-sew, to passive shunt, to heparin-less partial bypass.87
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree