Coronary artery spasm is a rare but potentially fatal disease. Herein, we report a case of recurrent ST-segment myocardial infarctions and ventricular fibrillation complicating severe multivessel coronary artery spasm successfully treated with bilateral thoracic surgical sympathectomy.
Coronary artery spasm (CAS) is an uncommon but potentially fatal disease. Enhanced sympathetic tone has been linked to refractory spasm, and sympathectomy has been used to treat and prevent refractory CAS. We report a case of a young woman with angina pectoris, multivessel refractory CAS, recurrent acute myocardial infarction, unexplained postural tachycardia, and ventricular fibrillation, which was successfully treated with video-assisted thoracoscopic surgery (VATS) for sympathectomy.
Case Presentation
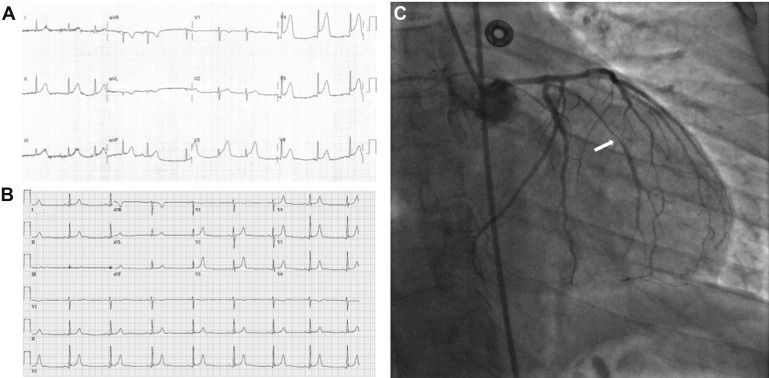
A 39-year-old white woman with no significant medical history presented to the emergency department with angina pectoris. She awoke in the middle of the night with substernal chest pain radiating to her left arm. The prehospital electrocardiogram showed ST-segment elevations in V3-V5 ( Figure 1 ). On arrival to the emergency department, the angina had subsided, her vital signs and examination were normal, and a repeat electrocardiogram showed no ST-segment deviations ( Figure 1 ). Troponin I levels were <0.03 pg/ml and 2.06 pg/ml on arrival and 3 hours later, respectively. She was admitted and treated for acute coronary syndrome and underwent coronary angiography showing 99% occlusion of the first obtuse marginal coronary artery, with evidence of intracoronary thrombus ( Figure 1 ), diffuse narrowing of the left anterior descending and left circumflex arteries, and no significant narrowing in the right coronary artery ( Figure 2 ). Two Integrity stents (2.75 × 26 mm and a 2.75 × 8 mm; Medtronic, Minneapolis, Minnesota) were implanted in the first obtuse marginal coronary artery with good angiographic results and Thrombolysis In Myocardial Infarction 3 flow.
The following day, she had recurrent chest pain with no dynamic changes on electrocardiogram. Given concerns for vasoconstriction, metoprolol was discontinued and diltiazem was started. Subsequently, she had recurrent symptoms with dynamic ST depression and further increase in troponin I. Intravenous nitroglycerin was started, and a repeat coronary angiogram showed patent coronary stents but documented further diffuse narrowing on all 3 coronary arteries consistent with diffuse epicardial coronary vasoconstriction refractory to intravenous and intracoronary nitroglycerin.
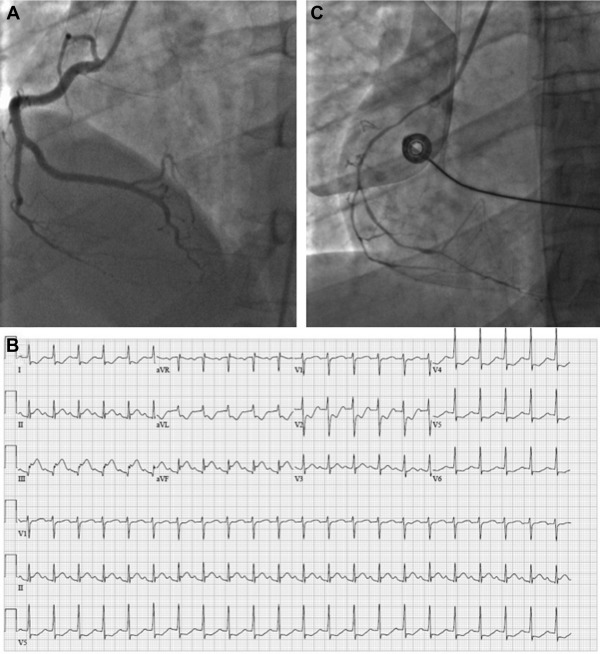
On day 3, a percutaneous ultrasound-guided left stellate ganglion blockade was performed with lidocaine 1%, 10 ml, and angina temporarily subsided. On day 4, she had significant increase in heart rate with orthostasis, from 85/min to 165/min with no changes in blood pressure, associated with angina and ST-segment depression in V4-V6, consistent with postural orthostatic tachycardia syndrome. Vasodilators were reduced, and intravenous fluids, fludrocortisone, and low-dose propranolol were added with a significant improvement of orthostatic tachycardia and reduction in the episodes of tachycardia-induced angina and ST-segment depression. On day 6, propranolol dose was further increased, and diltiazem was suspended. Approximately 12 hours later, she had recurrent severe angina pectoris while in bed, without tachycardia. Electrocardiogram showed ST-segment elevations in inferior leads ( Figure 2 ), refractory to high-dose intravenous nitroglycerin. Course was complicated by cardiac arrest due to ventricular fibrillation, requiring multiple electric shocks. A repeat coronary angiogram again demonstrated diffuse luminal narrowing of coronary arteries, with more severe obstruction of the right coronary artery ( Figure 2 ); first obtuse marginal coronary artery stents were patent. Vasodilators were started. On day 8, she underwent VATS sympathectomy. She had no recurrent angina or arrhythmias recurrences, and with resolution of postural orthostatic hypotension. She was discharged on aspirin, ticagrelor, atorvastatin, diltiazem, fludrocortisone (2-week course with taper) and a LifeVest wearable defibrillator (ZOLL, Pittsburgh, Pennsylvania) for 4 weeks. At 3- and 6-month follow–up, she had no recurrent clinical events.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


