Thoracic Surgery in the Elderly
Amanda Marsch
Joseph B. Zwischenberger
During the last several decades, the fastest-growing segment of our population is made up of people >65 years of age. The U.S. Census Bureau estimates that the group aged ≥65 will increase from 35 million in 2000 to >86 million by 2050.91 By 2030, it is estimated that 20% of the population will be >65 years of age. Interestingly, once age 75 is reached, men, on average, live another 10.8 years and women an additional 12.8 years.2 Today 15% of lung cancer patients are >75 years old. Because an individual who is alive at age 75 is expected to live, on average, 12 additional years, cancer management in the octogenarian should focus on quality of life as well as survival.12 Advanced age alone is no longer a contraindication to operation, even for higher-risk procedures in thoracic and vascular surgery.8,68,72
Just as children are not considered little adults, elderly patients should not be considered simply older people. A surgeon must understand the normal physiologic changes associated with aging to accurately construct a risk:benefit analysis specifically tailored to each patient. The focus should be on the patient’s current physiologic state, his or her life expectancy and quality of life, and pain control issues. The surgeon should anticipate end-of-life issues and the potential need for rehabilitation or nursing home placement in the early postoperative period.
Cardiovascular Physiology
Eighty percent of patients aged >80 years have identifiable cardiovascular disease; however, most show no obvious sign of impaired hemodynamic performance until their physiologic reserve is tested. Surgery may uncover their limited reserve by increasing myocardial oxygen demand or by anesthetic-induced vasodilatation.
The physiologic effects of aging result from an accumulation of processes that occur at the cellular, organ, and systems level as well as environmental factors, including infection, trauma, nutrition, and behavioral adaptation.23 The impact on the cardiovascular system at a cellular and tissue level includes changes in the walls of blood vessels that lead to stiffening of the vascular wall and increased peripheral vascular resistance.45 Increased peripheral vascular resistance causes hypertension, which in turn leads to accelerated myocyte turnover via apoptosis, hypertrophy of the remaining myocytes, and subsequent ventricular hypertrophy. Thickening of the ventricular wall results in prolonged myocardial contraction and delayed relaxation. Compared with that of 20-year-olds, the early diastolic filling of 80-year-old patients is reduced by one-third to one-half.46,81 Consequently, the left atrium enlarges to augment late diastolic filling.33 The nonstressed heart in normal sinus rhythm can compensate for some diastolic dysfunction, but tachycardia or hypertension may additionally reduce diastolic filling beyond the ability of the heart to compensate. The development of atrial fibrillation further diminishes cardiac output.
Congestive heart failure (CHF) is the leading cause of postoperative morbidity and mortality. Preoperative recognition of impaired cardiac function is essential for the perioperative fluid management that is required in order to minimize adverse outcomes. Changes at both the systemic and organ levels result in a decline in functional reserve. Even without identifiable cardiovascular disease, aging causes a decrease in cardiac output of 1% per year beginning at age 30.67 Cardiac output remains the key determinant of oxygen delivery. These pathophysiologic changes underscore the importance of maintaining the heart and vascular system in a nonstressed, normotensive sinus rhythm during surgical procedures.
Pulmonary Physiology
Pulmonary complications account for most of the morbidity encountered after thoracic surgery. Atelectasis, pneumonia, air leakage, and prolonged mechanical ventilation account for a morbidity rate of 7% to 33% after thoracic procedures in the elderly.51,74 Pulmonary changes associated with aging are evident by a loss of elastic recoil of the lung as well as atrophy of the chest wall muscle, resulting in decreased tidal volume.97 Impaired elasticity also causes ventilation/perfusion mismatch, leading to decreased oxygen transfer.28 As lung parenchyma is destroyed or thickened by aging, oxygenation is further impaired by decreased surface area for gas exchange.4 Residual volume can double between the ages of 20 and 65. Vital capacity (VC) decreases with age, resulting in an increase in dead space ventilation.66 Loss of parenchymal elasticity, joint stiffening, weakening of inspiratory muscles, and early small airway collapse also change gas flow characteristics. The forced expiratory volume in 1 second (FEV1) progressively declines with aging, resulting in an FEV1:VC ratio <70% by age 70. The sum of the respiratory changes associated with aging ultimately limits the maximal breathing capacity by age 70 to 50% of that at age 30.89
Chronic obstructive pulmonary disease (COPD) is the primary diagnosis in 18% of all hospital admissions of patients aged >65 years.56 Although the age-adjusted death rate for stroke and
coronary artery disease has declined in the last 30 years, the death rate for COPD has increased by 70%.63 With early diagnosis and aggressive preoperative pulmonary treatment, complication rates in the elderly with COPD can be minimized.16
coronary artery disease has declined in the last 30 years, the death rate for COPD has increased by 70%.63 With early diagnosis and aggressive preoperative pulmonary treatment, complication rates in the elderly with COPD can be minimized.16
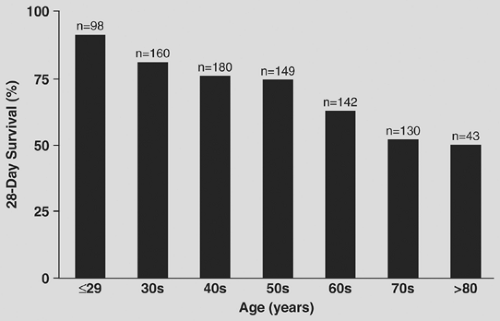
Prevalence of adult respiratory distress syndrome (ARDS) among hospitalized patients has been estimated to be as high as 40% in high-risk patients.41 The relationship between age and outcomes in ARDS shows a progressive decline in survival for each increasing age group at 28 days of hospitalization (Fig. 27-1). ARDS mortality rates in patients younger than 60 are between 12% to 45%, although rates in patients older than 60 are 64% to 72%.34,83,85
Renal Physiology
Age-related changes in the renal system are characterized by a progressive reduction in renal mass secondary to glomerulosclerosis and leading to decreased creatinine clearance in most aged patients.47,89 Glomerulosclerosis results in a decline in renal plasma flow and in glomerular filtration rate.32 Additionally, the age-related decline in cardiac output also impacts both renal plasma flow and glomerular filtration rate negatively. Patients with impaired glomerular filtration rate are more susceptible to volume overload in the perioperative period and accumulation of metabolic substances and drugs that must be excreted by the kidneys.64 Slowed drug elimination can lead to prolonged sedative effects of anesthetic and narcotic medication and a propensity for drug-induced acute renal failure after the administration of nonsteroidal anti-inflammatory medications, diuretics, and antibiotics.89 Impaired renal sodium conservation can lead to electrolyte imbalances that potentially affect cardiac conduction and lead to arrhythmia.1 The plasma level of creatinine may measure low in elderly patients because of reductions in skeletal muscle mass. Calculated creatinine clearance remains the most sensitive marker of renal function in the elderly.1
Preoperative Assessment
Coexisting disease has more impact on morbidity and mortality than age alone in the geriatric population.25 Likewise, age alone is not an independent risk factor for thoracic operation.68 A barrage of laboratory tests is generally not indicated and has been shown to be of no benefit in the elderly.27 A workup should begin with basic laboratory screening based on an individual’s comorbidities. Symptoms of ongoing infection should prompt an inquiry to identify the source and clear the infection before any elective procedure. Recent weight loss is important, and the nutritional state of the patient should be evaluated and corrected if possible. The National Veteran’s Affairs Surgical Risk Study has identified the American Society of Anesthesiologists (ASA) classification as the most important independent risk factor predicting postoperative mortality in both men and women.31,38 The second greatest indicator for mortality shared between both sexes is the preoperative serum albumin level. Age as an independent variable ranked fourth for predicting mortality in females and fifth in males.31,38
Cardiac Evaluation
Cardiac assessment usually begins with an electrocardiogram (ECG); however, 75% of patients >70 years of age have some abnormality on ECG, which has not been shown to predict outcome.50 Arrhythmias have been shown to impact postoperative cardiac morbidity adversely in elderly patients.51 Atrial fibrillation is the most common arrhythmia; it is estimated to be present in 10% of patients >80 years old and accounts for 75,000 thromboembolic events per year. New-onset atrial fibrillation requires rate control and attempts to restore normal rhythm. However, in asymptomatic patients, there is no survival benefit to converting chronic atrial fibrillation to sinus rhythm preoperatively. Rate control and anticoagulation are still the mainstays of treatment in chronic atrial fibrillation.
Cardiac complications in the elderly occur in 10.3% to 12.5% of patients with preexisting heart disease.48,74 Preexisting CHF can lead to a two- to fourfold increase in postoperative cardiovascular complications, including myocardial infarction (MI), supraventricular tachycardia, hypo- or hypertension, and cardiac arrest.48,94 Estimation of cardiac reserve can be difficult because most elderly patients with cardiac dysfunction are compensated and will show signs of disease only when stressed. Physical
reserve of elderly patients is difficult to estimate under circumstances of a sedentary lifestyle or general debility. Provocative testing with either a thallium scan or dobutamine stress test is helpful, and many recommend that it should be routine in identifying elderly patients with reversible ischemic heart disease.
reserve of elderly patients is difficult to estimate under circumstances of a sedentary lifestyle or general debility. Provocative testing with either a thallium scan or dobutamine stress test is helpful, and many recommend that it should be routine in identifying elderly patients with reversible ischemic heart disease.
Patients with coronary artery disease are at particular risk for perioperative myocardial ischemia. Tachycardia and hypertension during the operation can increase cardiac work and decrease coronary blood flow, leading to ischemia.94 Implementation of beta-adrenergic blocking agents should begin before a planned procedure and continue throughout the perioperative period. Intraoperative IV nitroglycerin dilates the coronary circulation and reduces cardiac stress to prevent myocardial ischemia. Patients with known CHF should have their fluid balance and hypertension well controlled before any elective procedure.
Pulmonary Evaluation
Pulmonary complications account for the highest morbidity after thoracic procedures in all age groups. Especially at risk are patients with a history of smoking, reactive airway disease, and recent pneumonia. Smoking cessation ≥2 months prior to surgery can reduce the risk of perioperative pulmonary complications to levels similar to that of nonsmokers; however, cessation ≤4 weeks presurgery can increase the risk of these complications!7 Smoking cessation should therefore be recommended only if both adequate time is available and patient compliance is evident. Predicting pulmonary recovery relies on pulmonary function testing with both volume and flow studies and assessment of exercise capacity and reserve. Among the various pulmonary function tests, the FEV1 has shown good correlation with predicting morbidity in thoracic surgery patients. An FEV1 >1.5 L predicted good outcomes in patients >70 years of age.35 Haraguchi and colleagues37 showed a predicted postoperative FEV1 <55% was the strongest independent predictor of pulmonary complications after pulmonary resection. Consequently, using this predictor as an exclusion criterion, they decreased their pulmonary morbidity rate from 33% to 9.8% and mortality rate from 10% to 0% for elderly patients undergoing resection for lung cancer.37
Exercise tolerance has also proved excellent in predicting morbidity in elderly patients. Simply having the patient walk flights of stairs can give a valuable functional assessment in the clinic. Brunelli and colleagues12 studied 109 patients >70 years old undergoing lobectomy for cancer. Patients who could climb more than four flights of stairs had a <20% cardiopulmonary complication rate, although those who could not climb at least three flights of stairs had a 57% complication rate.12 Achieving an exercise capacity of only 2 minutes with a heart rate of 99 beats per minute can lower an elderly patient’s complication rate from 42% to 9% and mortality rate from 7% to 1%.35 The data in these studies challenge the adage “three flights for a pneumonectomy, two for a lobectomy, and one for a thoracotomy.”
Many groups have studied the effects of preoperative pulmonary rehabilitation on patients undergoing surgery for lung volume reduction. A structured pulmonary rehabilitation program includes patient education, exercise training, psychosocial support, and nutritional intervention.99 The National Emphysema Treatment Trial, sponsored by the National Institutes of Health, reported the effects of lung volume reduction surgery versus medical treatment in patients with severe emphysema. All patients completed a preoperative pulmonary rehabilitation program. Significant improvements in exercise capacity, dyspnea, and health-related quality of life were observed postrehabilitation. In fact, 10% of the subjects in this trial improved sufficiently during the rehabilitation program and decided to forgo the risks of surgery.19
Intraoperative Approaches to Minimize Morbidity
Anesthesia
Physiologic changes seen in the elderly and their effects on drug bioavailability and side-effect profiles can define the type and dose of agent used for anesthesia. For instance, a decrease in total body water seen with aging leads to higher peak drug concentrations after bolus or rapid infusion.71 The progressive decrease in cardiac output observed in the elderly has many anesthesia considerations. The lower tissue perfusion can lengthen the time required to transport drugs to tissues and delay the time to peak effect. A relative reduction in perfusion to organs such as the liver and kidneys can prolong a drug’s duration of action by slowing metabolism and excretion.79 Most anesthetic drugs have some degree of cardiac depressant activity; therefore the dose delivered must be reduced in the elderly. In a patient with CHF, using drugs such as midazolam or opioids, which have minimal effects on cardiac contractility and heart rate, can reduce the likelihood of hypotension or arrhythmia at induction.5,88 For patients with minimal cardiac functional reserve, tachycardia has deleterious effects. Avoiding drugs like pancuronium, which induce tachycardia, can help avoid cardiac ischemia.94 Epidural anesthesia decreases perioperative cardiac stress and decreases tachycardia-induced cardiac ischemia.44,53
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree