Thoracic Outlet Syndrome (With Transaxillary, Supraclavicular, Posterior, and VATS Approaches)
Harold C. Urschel Jr.
Thoracic outlet syndrome (TOS) consists of compression of the subclavian vessels and brachial plexus at the superior aperture of the thorax. It was designated previously according to presumed etiologies such as scalenus anticus, costoclavicular, hyperabduction, cervical rib, and first rib syndromes. The various syndromes are similar and the specific compression mechanism is often difficult to identify; however, the first rib seems to be a common denominator against which most compressive factors operate.
The symptoms are neurologic, vascular, or mixed, depending on which component is compressed. Occasionally, the pain is atypical in distribution and severity and is experienced predominantly in the chest wall and parascapular area, simulating angina pectoris.17
Diagnosis of the nerve compression group can be objectively substantiated by determining the nerve conduction velocity. In the vascular compression group, diagnosis is usually established clinically and confirmed with angiography.
The ulnar nerve conduction velocity (UNCV) test, as described by Jebson4 and by Caldwell and associates,3 has widened the clinical recognition of this syndrome and improved diagnosis, selection of treatment, and assessment of therapeutic results.
Physiotherapy to improve posture, strengthen shoulder girdle muscles, and stretch neck muscles is used initially in most neurogenic cases of thoracic outlet syndrome and is often successful in cases of mild compression. Surgical treatment involves extirpation of the first rib, usually through the transaxillary approach except for arterial procedures, which may employ the supraclavicular approach. This is used for cases of severe compression that have not responded to medical therapy.
Anatomic Considerations
The subclavian vessels and brachial plexus traverse the cervicoaxillary canal to reach the upper extremity. The outer border of the first rib divides this canal into a proximal division triangle. This proximal division is composed of the scalene triangle and the space bounded by the clavicle and the first rib (the costoclavicular space). The distal division comprises the axilla. The proximal division is the most critical for neurovascular compression. It is bounded superiorly by the clavicle and the subclavious muscle; inferiorly by the first rib; anteromedially by the border of the sternum, the clavipectoral fascia, and the costoclavicular ligament; and posterolaterally by the scalenus medius muscle and the long thoracic nerve. The scalenus anticus, inserting on the scalene tubercle of the first rib, divides the costoclavicular space into two compartments: an anterior compartment, containing the subclavian vein, and a posterior compartment, containing the subclavian artery and brachial plexus. The axilla, which is the outer division of the cervicoaxillary canal, with its underlying structures—including the pectoralis minor muscle, the coracoid process, and the head of the humerus—is also an area of potential compression.
Compression Factors
Many factors can cause compression of the neurovascular bundle at the thoracic outlet. The basic factor, which was pointed out by Rosati and Lord,9 is deranged anatomy, to which congenital, traumatic, and atherosclerotic factors may contribute (Table 46-1).
Bony abnormalities are present in approximately 30% of patients, either as a cervical rib, a bifid first rib, fusion of first and second ribs, clavicular deformities, or previous thoracoplasty.
Pathologic changes in the configuration of the cervicoaxillary canal alter the normal functional dynamics and serve as the basis of the clinical maneuvers used in the diagnosis of thoracic outlet syndrome.
Diagnosis
The basic diagnostic consideration for thoracic outlet syndrome includes the history and physical examination, radiographs
of the chest and cervical spine, neurologic consultation, electromyography, and UNCV. On occasion, cervical myelography, magnetic resonance imaging (MRI), computed tomography (CT), coronary angiography, venography, or arteriography may be necessary to confirm the diagnosis.
of the chest and cervical spine, neurologic consultation, electromyography, and UNCV. On occasion, cervical myelography, magnetic resonance imaging (MRI), computed tomography (CT), coronary angiography, venography, or arteriography may be necessary to confirm the diagnosis.
Table 46-1 Etiologic Factors in Thoracic Outlet Syndrome | |||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Signs and Symptoms
The symptoms and signs of thoracic outlet syndrome depend on whether the nerves, blood vessels, or both are compressed at the thoracic outlet (Fig. 46-1).
Signs and symptoms of nerve compression occur most frequently; arm pain and paresthesias are present in about 95% of patients and motor weakness in <10%. Pain and paresthesias are segmented in 75% of cases, with 90% occurring in the ulnar nerve distribution. Pain is usually insidious in onset and commonly involves the neck, shoulder, arm, and hand.
Compression Tests
Adson or Scalene Test
The Adson test, or scalene test, described by Adson in 1951,2 tightens the anterior and middle scalene muscles, thus decreasing the interscalene space and magnifying any preexisting compression of the subclavian artery and brachial plexus. The patient is instructed to (a) take and hold a deep breath, (b) extend his or her neck fully, and (c) turn his or her face toward the side. Obliteration or diminution in the radial pulse suggests compression.
Costoclavicular Test: Military Position
In the costoclavicular test, the shoulders are drawn downward and backward; this maneuver narrows the costoclavicular space by approximating the clavicle to the first rib, thus tending to compress the neurovascular bundle. Changes in the radial pulse with production of symptoms indicate compression.
Hyperabduction Test
When the arm is hyperabducted to 180 degrees, the components of the neurovascular bundle are pulled around the pectoralis minor tendon, coracoid process, and head of the humerus. If the radial pulse decreases, compression should be suspected.
Arm Claudication Test
In the arm claudication test, the shoulders are drawn upward and backward. The arms are raised to the horizontal position with the elbows flexed 90 degrees. With exercises of the hands, if compression is present, numbness or pain is experienced in the hands and forearms.
Pseudoangina
In some patients the pain is atypical, involving the anterior chest wall or the parascapular area; it is then termed pseudoangina because it simulates angina pectoris. Urschel and associates17 reported that these patients have normal coronary arteriograms and decreased ulnar nerve conduction velocities, strongly suggesting the diagnosis of thoracic outlet syndrome. The usual shoulder, arm, and hand symptoms that might have provided the clue for the diagnosis of thoracic outlet syndrome are initially either absent or minimal compared to the severity of the chest pain. Without a high index of suspicion, the diagnosis of thoracic outlet syndrome is frequently overlooked, and many of these patients become “cardiac cripples” without an appropriate diagnosis or develop severe psychological depression when told that their coronary arteries are normal and that they have no significant cause for their pain.
To understand the symptomatic overlap between coronary artery disease and this atypical manifestation of the thoracic outlet syndrome (i.e., pseudoangina), it is necessary to review the neuroanatomy, innervation, and pain pathways of the arm, chest wall, and heart.
At least two types of pain pathways are present in the arm. These are the commonly acknowledged C5–T1 cutaneous more superficial fibers and the T2–T5 afferent spinal fibers, which travel with the sympathetic nerves and transmit “deeper” painful stimuli from the ulnar, median, and parascapular distribution, as reported by Kuntz.5 The cell bodies of the two types of afferent neurons are situated in the dorsal root ganglia of the corresponding spinal segments. They synapse in the dorsal gray matter of the spinal cord and the axons of the second-order neurons, cross the midline, and ascend in the spinothalamic tract to the brain.
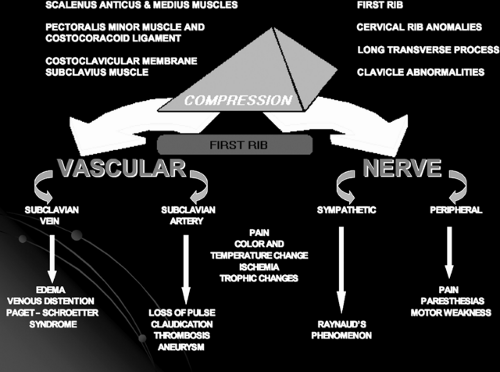 Figure 46-1. Schematic diagram showing the relation of muscle, ligament, and bone abnormalities in the thoracic outlet that may compress neurovascular structures against the first rib. |
Compression of the “superficial” C8–Tl cutaneous afferent fibers elicits stimuli that are transmitted to the brain and recognized as integumentary pain or paresthesias in the ulnar nerve distribution. In contrast, compression of the predominantly “deeper” sensory fibers elicits impulses that are interpreted by the brain as deep pain originating in the arm or referred to the chest wall.
The pseudoangina experienced in thoracic outlet compression shares with angina pectoris the same dermatomal distribution, in that the heart, arm, and chest wall have afferent fibers convergent on T2–T5 spinal cord segments and cell bodies that are located in the corresponding dorsal root ganglia. Referred pain to the chest wall is a component of both pseudoangina and angina pectoris. Because somatic pain is more common than visceral pain, the brain interprets activity arriving in a given pathway as a pain stimulus in a particular somatic area.
Two theories attempt to explain the mechanism of referred pain from the heart or arm stimuli to chest wall. The convergence theory holds that somatic and visceral afferents converge on the same spinothalamic neurons; when the same pathway is stimulated by activity in visceral afferents, the signal reaching the brain is the same and the pain is projected to the somatic area. The facilitation effort theory holds that because of subliminal fringe effects, incoming impulses from visceral structures (e.g., heart) lower the threshold of spinothalamic neurons receiving afferents from somatic areas. Thus, minor activity in the pain pathways from the somatic areas (activity that would normally die out in the spinal cord) passes on to the brain and is interpreted as somatic pain rather than pain in the viscera, where the stimulus was initiated.
Vascular Compression Symptoms
Symptoms of arterial compression (occlusion, aneurysm or emboli) in thoracic outlet syndrome, are much less common than those of neurologic compression, and include coldness, weakness, easy fatigability of the arm and hand, and pain that is usually more diffuse in distribution. Raynaud’s phenomenon is
occasionally noted. Venous compression is recognized by edema, venous distention, and discoloration of the arm and hand. Thrombosis of the subclavian vein (“effort thrombosis” or Paget-Schroetter Syndrome [PSS]) may produce sudden swelling and blueness of the arm and hand. It is associated with subcutaneous venous collateral circulation around the shoulder (Urschel’s sign).
occasionally noted. Venous compression is recognized by edema, venous distention, and discoloration of the arm and hand. Thrombosis of the subclavian vein (“effort thrombosis” or Paget-Schroetter Syndrome [PSS]) may produce sudden swelling and blueness of the arm and hand. It is associated with subcutaneous venous collateral circulation around the shoulder (Urschel’s sign).
Objective physical findings, in contrast, are more common in patients with primarily vascular rather than neural compression. Loss or diminution of radial pulse and reproduction of symptoms can be elicited with Adson’s test, costoclavicular (military) position, and hyperabduction maneuvers in most patients with arterial compression. Raynaud’s phenomenon, temperature changes, and arterial occlusion with claudication may occur. In case of neural compression, the objective neurologic findings, which occur less frequently, consist of hypoesthesia, anesthesia, and occasionally muscular weakness or atrophy.
Nerve Conduction Velocity
Motor conduction velocities of the ulnar, median, radial, and musculocutaneous nerves can be reliably measured, as described by Jebson. Caldwell and associates3 improved and adapted to clinical use the technique of measuring UNCV in evaluating patients with thoracic outlet compression. Conduction velocities over proximal and distal segments of the ulnar and median nerves are determined by recording the action potentials generated in the hypothenar or first dorsal interosseous muscles. The points of stimulation are the supraclavicular fossa, mid-upper arm, area below the elbow, and wrist. The Meditron 201-AD or the TECA B-3 electromyogram including the coaxial cable with three needle or surface electrodes can be used for this examination. The normal UNCV values are 85 m/s across the thoracic outlet, 55 m/s around the elbow, 59 m/s in the forearm, and 2.5 to 3.5 m/s at the wrist. In patients with thoracic outlet syndrome, the average UNCV value is reduced to 53 m/s across the outlet (range of 32–65 m/s) as reported by Urschel and colleagues.12,16
Angiography
Simple clinical observations usually suffice to determine the degree of vascular impairment in the upper extremity, but peripheral ultrasonography, angiography, or MRAs confirm the diagnosis. Bruits in the supra- or infraclavicular spaces suggest stenoses, and absence of pulse denotes total obstruction. In these instances, retrograde or antegrade arteriograms of the subclavian and brachial arterial systems are indicated to demonstrate localized pathologic changes. Using arteriography or phlebography routinely for demonstrating temporary occlusion of the vessels in different arm positions would seem redundant to an adequate clinical examination in most patients and may be associated with some morbidity.
In instances of venous stenosis or obstruction, as in PSS, ultrasonography or phlebography is indicated to discern the extent of thrombosis and to determine the status of collateral venous circulation. After successful thrombolysis, because the stenosis appears localized, attempts have been made to dilate it with a balloon and insert intravascular stents “to keep the stenosis open.” All have occluded in the experience of Urschel20 and in the experience of others.10 Remaining stenosis after successful thrombolysis is related to external compression of the vein by the costoclavicular ligament and scalenus anterior muscle, and should be removed surgically. Dilatations and stents are contraindicated.
Differential Diagnosis
The cardinal rule for the establishment of thoracic outlet diagnosis is the elimination of significant coronary artery disease, as well as pulmonary, esophageal, and chest wall etiologies. It is also necessary to differentiate it neurologically from lesions of the cervical spine, brachial plexus, and peripheral nerves (Table 46-2), as well as from other arterial and venous phenomena (Table 46-3).
Table 46-2 Differential Diagnosis of Nerve Compression | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Table 46-3 Differential Diagnosis of Vascular Compression | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Therapy
Most patients with neurologic TOS receive physiotherapy before operative intervention. Such therapy must not be the same as given to patients with the cervical syndrome, which often exaggerates the symptoms of thoracic outlet compression. Proper physiotherapy for thoracic outlet compression includes heat massages, active neck exercises, scalenus anticus muscle stretching, strengthening of the upper trapezius muscle, and posture instruction. Because sagging of the shoulder girdle, common among middle-aged people, is a main etiologic factor in this syndrome, many patients with less severe disease benefit from strengthening the shoulder girdle and improving posture. More than two-thirds of neurogenic TOS patients seen in consultation required no surgical procedure, but improved significantly with conservative management.
The normal UNCV across the thoracic outlet is 85 m/s. Most patients with an UNCV above 60 m/s improve with conservative management. Most patients with an UNCV below 60 m/s require surgical resection of the first rib and correction of other bony abnormalities.
Physical therapy is not used in patients with PSS or acute arterial insufficiency problems because of the urgency for immediate interventional therapy in both situations. The primary use for physical therapy and conservative management trials is for primary neurologic or recurrent thoracic outlet syndromes. The exception would be a patient who is developing motor deficits and should have prompt first rib removal and neurovascular decompression.
Surgical Approaches for Rib Extirpation and Neurovascular Decompression
Transaxillary
For primary venous or neurologic TOS, resistant to conservative management, the preferred approach is the transaxillary resection of the first or cervical rib with neurovascular decompression as suggested by Roos in 1966.7,8 Because most patients are women, the scar is unobtrusive and difficult to visualize; no major muscles are divided, and the cervical or first rib may be removed directly without retraction of the brachial plexus or blood vessels. The wound, however, is deeper, and more light and magnification are required, and greater experience is necessary, than for the other approaches. The costoclavicular ligament in Paget-Schroetter Syndrome is readily accessible from this approach and difficult to remove from the supraclavicular or posterior approaches.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


