INDICATIONS/CONTRAINDICATIONS
Thoracic outlet syndrome (TOS) is a spectrum of disorders resulting from compression of the neurovascular structures within the thoracic outlet. The three subtypes of TOS are identified based on the structures affected: The brachial plexus which is compressed in the most common subtype, neurogenic TOS; the subclavian vein which may be thrombosed in the second most common subtype, venous TOS; and the subclavian artery which may become stenotic or aneurysmal in arterial TOS. Transaxillary approach to first rib resection and anterior scalenectomy is indicated in all three subtypes of TOS unless the subclavian artery needs to be resected and replaced.
The initial treatment of neurogenic TOS is nonoperative with physical therapy, avoidance of inciting activities, and image-guided neuromuscular blockade of the anterior scalene muscle with lidocaine of Botulinum toxin A (Botox). Ample time is allowed for work with physical therapists, at least several months. If no improvement occurs with physical therapy, if the anterior scalene block is positive (the patient obtains temporary symptomatic relief with local anesthetic injection), and if symptoms are truly significant, then an operation is offered.
Transaxillary first rib resection and scalenectomy is indicated for both venous and arterial TOSs as symptoms will recur without this definitive operation even if thrombus is removed via thrombolysis or thrombectomy. Reoperation for residual symptoms after prior supraclavicular first rib resection is also best performed with a transaxillary approach as this avoids scar tissue from the prior operation.
Another indication for this operation is the symptomatic presence of a cervical rib. Cervical ribs, defined as anomalous ribs originating from the seventh cervical vertebrae, are frequently fused to the first rib and may cause symptomatic arterial compression, thrombosis, aneurysm formation, and embolization. Those patients with symptomatic cervical ribs who do not require vascular reconstruction should undergo transaxillary first rib resection, anterior scalenectomy, and cervical rib resection. Patients with this syndrome who require arterial bypass are best served by a supraclavicular approach that allows arterial reconstruction at the time of rib resection.
A contraindication to the transaxillary approach is first rib resection in patients with arterial TOS in whom replacement of the subclavian artery is planned due to aneurysmal changes. These patients are best served with a supraclavicular approach (with sometimes an infraclavicular counterincision) which allows direct arterial reconstruction. Also, preoperative first rib resection in a patient who has had a transaxillary approach should be done using the supraclavicular technique.
 PREOPERATIVE PLANNING
PREOPERATIVE PLANNING
Preoperative planning and evaluation vary depending on the type of TOS with which the patient presents.
Patients with suspected neurogenic TOS often present with vague symptoms of arm pain, weakness, or paresthesias. These nonspecific symptoms may result from many other conditions, and thus it is imperative to determine whether such patient have TOS and may benefit from first rib resection. A reliable approach to confirming the diagnosis is neuromuscular blockade of the anterior scalene muscle. The diagnosis is confirmed if an injection of lidocaine into the anterior scalene under ultrasound or computed tomography (CT) guidance produces relief. Nonoperative management should then be attempted, with physical therapy and careful attention to activities that incite symptoms. Botulinum toxin A may also be injected into the anterior scalene muscle for longer duration of relief. If nonoperative management is unsuccessful, first rib resection and anterior scalenectomy is indicated.
Venous TOS typically presents with arm swelling and subclavian vein thrombosis in the setting of exercise or overuse. Thrombosis may be acute or chronic. This disease entity is also known as effort-induced thrombosis of the subclavian vein or Pagett–Schroetter syndrome. Historically, these patients underwent thrombolysis and percutaneous venoplasty. Recent data indicate that preoperative thrombolysis and percutaneous venoplasty are of no benefit for patients with TOS manifested by subacute or chronic venous thrombosis. Preoperatively, these patients should undergo laboratory evaluation for the presence of hypercoagulable disorders such as Factor V Leiden mutation, protein C or S deficiency, antithrombin III deficiency, prothrombin gene mutations, homocysteinemia, activated protein C (APC) resistance, antiphospholipid antibodies, and lupus anticoagulant. Patients with venous TOS should also be anticoagulated, preferably with therapeutic dosing of Lovenox of 1 mg/kg twice a day, which is continued until the operation.
Arterial TOS is characterized by chronic thrombosis manifesting as arm claudication, or in the acute form by potentially limb-threatening hand and digit ischemia due to thromboembolism from the subclavian artery secondary to compression. These patients often have a bony abnormality such as a cervical rib. Poststenotic dilatation and aneurysm formation may occur in the subclavian artery in the chronic form of the syndrome. Preoperative planning may include urgent thrombolysis or thrombectomy in the presence of clinically significant distal ischemia. Hypercoagulability studies are conducted as for venous TOS. A plain chest radiograph should be obtained to evaluate for the presence of a cervical rib and other bony abnormalities. A duplex ultrasound should also be performed to evaluate for arterial stenosis and dilatation, as well as to measure arterial velocities. An arteriogram may be helpful in delineating thrombosis or aneurysm formation. It is imperative to determine whether the patient requires arterial reconstruction in addition to first rib resection and scalenectomy, as the transaxillary approach should be reserved for patients not undergoing arterial bypass. The supraclavicular approach is best for patients who require replacement of the subclavian artery.
 SURGERY
SURGERY
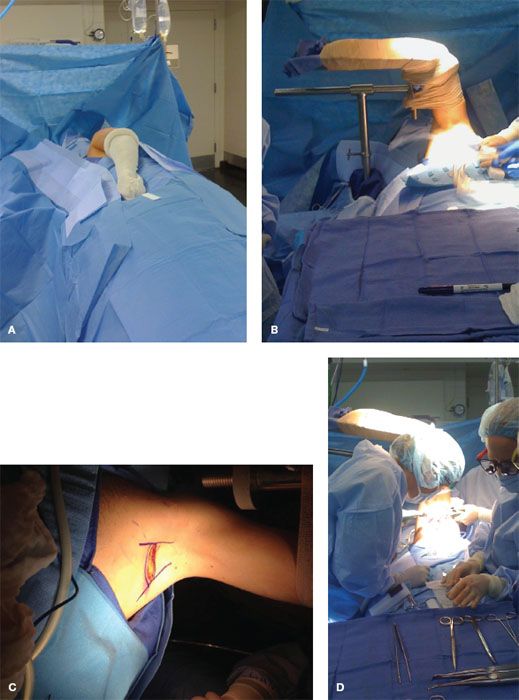
The operation of first rib resection and anterior scalenectomy is performed under general endotracheal anesthesia. Short acting paralytics are used at the start of the operation, so that their effects wear off and do not interfere with nerve identification during the operation.