Chapter 31 Thoracic Outlet Syndrome and Vascular Disease of the Upper Extremity
Thoracic Outlet Syndrome
History
TOS is still a controversial subject in regard to its diagnosis, conservative management, and surgical treatment. The concept of the disease and the anatomic structures focused on have changed over the centuries. In 1821, Cooper noted that subclavian artery thrombosis was due to compression by a cervical rib.1 This compression became known as cervical rib syndrome. From 1920 to 1931, the scalene muscles, first rib, and congenital ligaments became the focus to explain neurovascular compression in the thoracic outlet region.2–4 Next, the term scalenus anticus syndrome became popular, and an association with trauma was described.5,6 The costoclavicular syndrome, compression between the clavicle and first rib, was described in 1943.7 Peet and colleagues introduced the term thoracic outlet syndrome in 1956,8 and Rob and Standeven proposed the term thoracic outlet compression syndrome in 1958.9 More recent studies have emphasized histologic abnormalities indicating scalene muscle fibrosis in TOS patients.10,11
Over the years, various surgical approaches have been proposed. Coote performed a cervical rib resection in 1861.12 Murphy performed a first rib resection in 1908.13 Because of the high nerve complication rate associated with this procedure, the first scalenectomy was performed by Adson and Coffey in 1927,14 but it was realized that division of the muscle alone eventually led to reattachment of the muscle fibers and scarring, causing recurrent symptoms. Clagett reintroduced the first rib resection with a posterior approach in 1962.15 In 1966, Roos described the transaxillary approach for first rib resection,16 which is less invasive and more cosmetic and has become one of the standard approaches. In the late 1960s, an approach using an infraclavicular incision alone was described17; however, this approach produced a large, cosmetically unpleasant scar and, more importantly, provided only limited exposure posteriorly. Sanders and coworkers18 reintroduced scalenectomy for the treatment of recurrent TOS after first rib resection and posttraumatic TOS in 1979. For the purpose of total decompression, Atasoy introduced a combined approach, a transaxillary first rib resection and transcervical anterior and middle scalenectomy, in 1996.19
Incidence and Demographics
The incidence of TOS is reported to be approximately 0.3% to 2% in the general population.19,20 The most common age range is 25 to 40 years. Patients in their teens as well as octogenarians have also been diagnosed with TOS, although rarely. Women are more commonly affected than men, with a female-to-male ratio of 4 : 1.
Anatomy
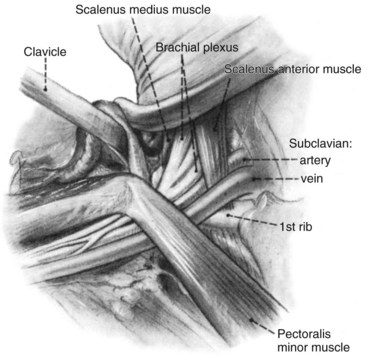
A knowledge of the complex anatomy of the thoracic outlet is crucial to understanding the pathogenesis of TOS and making the diagnosis. The thoracic outlet is defined as the musculoskeletal structures surrounding three important structures: subclavian artery, subclavian vein, and brachial plexus. This triangle is formed by the anterior scalene muscle, middle scalene muscle, and first rib (Figure 31-1). The subclavian artery arises from the upper mediastinum, passes behind the anterior scalene muscle, and arches over the first rib; it therefore courses through the scalene triangle, which is bordered by the anterior and middle scalene muscles and has the first rib as its floor. The nerve roots (C5 to T1) of the brachial plexus, after exiting the intervertebral foramina, unite to form the upper (C5 and C6), middle (C7), and lower (C8 and T1) trunks of the brachial plexus. They lie posterior, lateral, and superior to the subclavian artery and travel through the scalene triangle with the artery, with the lower trunk having a close relationship with the artery. The subclavian vein follows a similar course but, in contrast to the subclavian artery and brachial plexus, does not traverse the scalene triangle. It courses anterior to the insertion of the anterior scalene muscle on the first rib, outside the scalene triangle, and runs inferior and lateral to the subclavius tendon and costocoracoid ligament. All three structures then follow a similar course, passing under the clavicle and subclavius muscle and beneath the pectoralis minor near its insertion into the coracoid process and giving off several branches before entering the upper arm. Throughout their course, the neuromuscular structures are confined by various myofascial coverings.
In addition to the brachial plexus, two nerves in this area are surgically important. The phrenic nerve, a motor nerve to the diaphragm, arises primarily from C4 and usually receives branches from C3 and C5. The nerve travels on the anterior surface of the anterior scalene muscle, crossing lateral to medial. Because of this anatomic relationship, the nerve is vulnerable to injury during scalenectomy. Thirteen percent of the population has a double phrenic nerve.21 The long thoracic nerve arises primarily from C6 and usually receives branches from C5 and C7. It courses through or just posterior to the middle scalene muscle and then descends over the first rib to reach the serratus anterior muscle. Injury to the nerve results in winging of the scapula. Another surgically important structure is the thoracic duct, which empties into the left subclavian vein and is susceptible to operative injury resulting in troublesome lymphatic leakage.
Cause
Osseous Changes
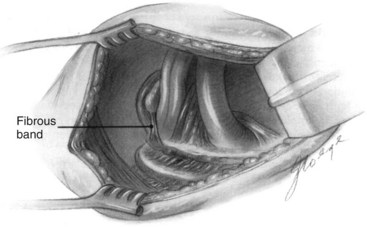
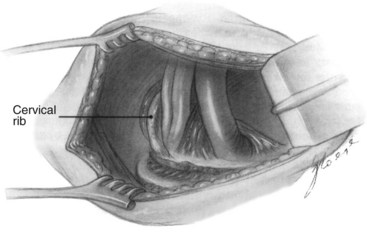
Cervical ribs, present since birth, are regarded as predisposing factors. They have an incidence of 0.5% to 1.5% in the general population22–24; approximately 50% are bilateral,25,26 and there is a female-to-male ratio of 2 : 1. Most are asymptomatic,27 but they are found with increasing prevalence in patients with TOS, reportedly occurring in 4% to 11% of patients who undergo TOS decompression surgery.23,28,29 The size of the cervical rib may vary. The ribs often have rudimentary or incomplete ossification, with a fibrous band extending from the tip and inserting on the first rib (Figure 31-2). Complete cervical ribs often insert on the first rib and occasionally are accompanied by an area of hyperostosis or even a fairly well-developed joint structure (Figure 31-3). The brachial plexus is stretched over the cervical rib or accompanying fibrous bands, which produces compression, usually in the lower trunk.30 Other osseous factors predisposing a patient to symptomatic TOS include a long transverse process of C7, first rib fracture, bifid first rib, and malunion of the clavicle. Poor posture with anterior displacement31 and saggy or droopy shoulders are also included in this category. It should be noted that the presence of a radiographically observed anatomic anomaly is not always necessary for the diagnosis.
Soft Tissue Abnormalities
Congenital fibromuscular bands and ligaments are observed in a majority of patients with neurogenic TOS.30 Some authors report anomalous bands or ligaments found at the time of surgery in more than 80% of their patients.32,33 These bands and ligaments have been present since birth and are categorized into nine different types.30,34
Scalene muscles are the most important structures that cause upper extremity symptoms. Congenital or acquired scalene muscle changes may be observed. One anatomic variation is the smallest scalene muscle (scalenus minimus) originating from the transverse process of the C7 vertebra, interdigitating between the subclavian artery and the brachial plexus, inserting in conjunction with the anterior scalene muscle on the first rib, and producing further compression (Figure 31-4). The role of the smallest scalene muscle has previously been underappreciated, but our review of 185 patients undergoing TOS surgery revealed that it was a prevalent (68.1%) and clinically significant marker for contralateral TOS surgery (unpublished data).
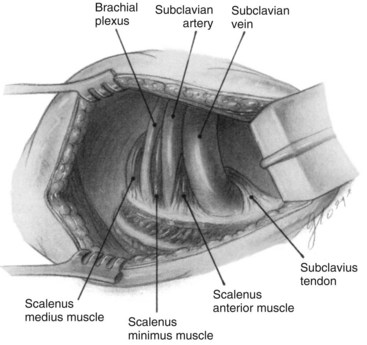
FIGURE 31-4 Appearance of the scalenus minimus abnormality from the transaxillary surgical approach.
(From Makhoul RG, Machleder HI: Developmental anomalies at the thoracic outlet: an analysis of 200 consecutive cases. J Vasc Surg 16:534–545, 1992.)
Another variation is a narrow scalene triangle, which could have a significant role in the development of TOS symptoms.35 The anatomic relationship between the scalene angle and the brachial plexus—the nerve roots emerging from the apex of the scalene triangle (a higher anatomic region)—might also contribute to symptoms.35 A hypertrophied subclavius muscle may be a factor in TOS as well.
Trauma
In addition to anatomic predispositions, trauma has been implicated as a precipitating factor for symptomatic TOS. Typical major trauma includes whiplash injuries of the neck36 and blows to the shoulders resulting in acute hyperextension injury, often occurring during motor vehicle accidents. Some reports note that approximately 80% of TOS patients have symptoms precipitated by trauma to the neck and shoulder girdle area.37,38 Stress injury, caused by repetitive motion or specific occupational activities over a prolonged period (e.g., continual abduction of the arms or excessive computer use), can also lead to TOS. Even upper extremity injury can cause TOS. Trauma causes spasm, inflammation, edema, and swelling, followed by scarring and fibrosis; this leads to increased muscle thickness, narrow interscalene spaces, and eventually compression of the neurovascular structures during contraction. The onset of symptoms may be delayed by days to weeks or even months.35 Significant histologic muscle fiber changes have been demonstrated in the scalene muscles of patients with neurogenic TOS.10,11
Pathology
Studies focusing on the histochemical and morphometric analysis of the anterior scalene muscle have opened a new area of investigation into the causes of neurovascular compression at the thoracic outlet.10,11 This research has been particularly useful in demonstrating the changes that occur in posttraumatic neurogenic TOS and often appear in the absence of obvious structural abnormalities.
Clinical Presentation
Neurologic Symptoms
Neurologic symptoms caused by thoracic outlet compression of the brachial plexus predominate in 94% to 97% patients.37,39 The symptoms of neurogenic TOS are basically the same as those of nerve compression in other regions of the body: pain, paresthesia, tingling sensation, and weakness for peripheral nerves; and Raynaud’s syndrome, temperature change, and color change for autonomic nerves. Typically, two patterns of brachial plexus compression have emerged. Lower plexus (C8 and T1) involvement is regarded as more common than upper plexus (C5 and C6) involvement; however, the picture is often mixed.40
Lower brachial plexus thoracic outlet compression usually causes sensory disturbance to the ulnar nerve distribution. Patients complain of pain and paresthesias in the medial (ulnar) aspect of the arm from the axilla, through the brachial area and the forearm, down to the hand (the fourth and fifth fingers). Ulnar-innervated muscles include the hypothenar, interosseous, and deep flexors of the ring and little finger. Pain in the anterior or posterior shoulder region and the side or back of the neck radiating into the occipital or mastoid area of the skull is also characteristic.41
Patients with upper plexus TOS usually exhibit symptoms in the forearm and upper arm, rather than the hand. Upper plexus TOS also produces pain in the side of the neck that radiates upward to the ear and may include the mandible, face, temple, and occipital regions, with hemicranial headaches.40 The pain radiates posteriorly to the rhomboid area, anteriorly across the clavicle into the upper pectoral region, laterally through the trapezius and deltoid muscle areas, and down the outer arm.41 Compression of the upper trunk may cause evidence of C5 to C7 nerve root involvement or sensory disturbance to the median nerve distribution.42
Brachial plexus compression can cause subjective coldness of the hand, even pallor, which may be mistakenly interpreted as arterial insufficiency or complex regional pain syndrome type I (reflex sympathetic dystrophy). In more advanced cases, weakness of the hand and loss of dexterity of the fingers frequently develop.22 The lateral thenar muscles are most severely affected. In late cases there is muscle atrophy, impaired use of the arm without paralysis, or even a “claw” hand.
Venous Symptoms
Venous TOS is less common than neurogenic TOS and accounts for 2% to 3% of cases.21,39 Venous obstruction produces swelling, edema, cyanosis, and discomfort of the arm that is aggravated with exercise. Patients may have a sudden onset of symptoms because of subclavian vein thrombosis. The natural clinical course is protracted, with continued disability. Collateral venous circulation develops over time and may be evident as distended superficial veins of the shoulder and chest. Vigorous activity is often difficult in the presence of chronic subclavian vein occlusion.
Arterial Symptoms
Arterial involvement is the least common form of presentation, constituting 1% to 2% of cases.21,39 These patients exhibit signs of ischemia: pain, pallor, pulselessness, and coolness of the affected side. They often experience fatigue of the arm with exercise and ischemic claudication, particularly with the arm elevated. Ischemic ulcers on the hand or gangrenous fingertips may occur because of thrombosis or embolization; this indicates severe narrowing or aneurysm of the subclavian artery. Retrograde embolization to the brain circulation can occur. In the authors’ series, 1.5% of all surgical TOS patients (43% of arterial TOS patients) exhibited vertebrobasilar stroke (unpublished data).
Physical Examination
Inspection and Palpation
The initial examination of the upper extremity should begin with inspection and palpation for discoloration, such as blanching, cyanosis, or gangrene; muscle atrophy; abnormal fingernail and hair growth; and temperature, moisture, and pulse. A note should be made of abnormal distension of veins, which could be collateral vessels, particularly around the shoulder. The symmetry and positional change of the vessels should be noted.43 Muscle atrophy, particularly in the hypothenar, is not common, but not rare, in TOS. The hands should be examined at the same time and compared with each other.
Auscultation
Auscultation should begin in the supraclavicular fossa bilaterally. It should then be performed with the stethoscope just beneath the middle third of the clavicle beginning with the arm in the neutral position and then gradually bringing it up into the abducted and externally rotated position. This is done while palpating the radial pulse. If obliteration of the radial pulse occurs, the stethoscope should be moved laterally in the infraclavicular area, then medially in the supraclavicular area, to detect bruits and a site of compressive occlusion. Because blood flow may be totally obliterated at the thoracic outlet, the maneuver should be performed slowly so as not to overlook bruits.43
Muscle Strength Test
Because muscle weakness can be one of the objective findings of TOS, the strength of all muscle groups of the arm should be tested. Patients may have weakness of the shoulder girdle muscles (deltoid), biceps, and triceps in cases of upper plexus compression (C5 to C7) and weakness of the intrinsic muscles of the hands in lower plexus compression (C8 to T1). Note that most TOS patients (85% to 90%) have combined symptoms of upper and lower plexus compression.40 The patient is asked to make a ring with the thumb (the thenar muscle innervated by the median nerve) and the little finger (the hypothenar muscle innervated by the ulnar nerve) against resistance. The interosseous muscles are tested using the interdigital card test and spreading the fingers apart against resistance. Grip strength should be measured with dynamometry.
Provocative Clinical Tests
Positional and pressure maneuvers that increase pressure on the nerve may be used to elicit symptoms and make a clinical diagnosis. The patient should complain of reproduction of symptoms in the correct nerve distribution. However, these results should be interpreted carefully. Obliteration of a peripheral pulse or even the production of symptoms during the examination does not necessarily mean pathology; this may occur in normal individuals. These tests should be used to supplement other physical, radiographic, or historical findings that point to the diagnosis. These provocative tests (pressure, position, and Tinel) should also be performed at the common distal sites of nerve compression in the upper extremity to determine any concomitant sites of nerve compression that may be present and contributing to the patient’s symptoms.23
Adson Test.
The Adson test is performed by holding the patient’s arm down while the head is turned toward the affected side with slight cervical extension.14 The radial pulse is evaluated when the patient inspires deeply. This maneuver may narrow the scalene triangle, compressing the subclavian artery and brachial plexus. It should be considered positive when the radial pulse is obliterated or diminished or symptoms are reproduced.
Abduction and External Rotation Test and Wright’s Hyperabduction Test.
The abduction and external rotation test requires abducting the arms to 90 degrees in external rotation, which rotates the clavicle and subclavius muscle posteriorly and inferiorly. Wright’s hyperabduction test is performed with the shoulders hyperabducted to 180 degrees and rotated externally while turning the head away from the affected side.44 Symptoms caused by a narrow interscalene space are aggravated by abduction of the extremity because the nerves are pushed up against the tight, narrow area, increasing pressure on them. Deep inspiration with breath holding may accentuate an ambiguous response. The patient is checked for any change in pulse and any symptoms in the arm. The test should be considered positive when the radial pulse is obliterated or diminished or if symptoms, such as weakness, tiredness, and numbness in the arm and paresthesia in the fingers, are reproduced. The duration of these provocative tests should not exceed 2 minutes and preferably should last only 1 minute. Care must be taken to avoid misdiagnosing an ulnar nerve neuropathy at the elbow.
Elevated Arm Stress Test.
The elevated arm stress test (or Roos test) requires the shoulders to be abducted and externally rotated 90 degrees and the elbows flexed 90 degrees with rapid opening and closing of the hands.30 This test is performed for up to 3 minutes, as long as the patient has no complaint. Reproduction of symptoms, such as fatigue, cramping, pain, or paresthesia, within 3 minutes is considered a positive test.
Laboratory Tests
Electrophysiologic Tests
Because the majority of symptoms of TOS are caused by neural compression, a variety of electrophysiologic tests have been proposed for the objective diagnosis of TOS. However, because compression is positional and intermittent, and electrophysiologic change may occur in late cases,41 these tests have a low level of sensitivity for TOS diagnosis.19 A positive electrophysiologic study confirms the clinical diagnosis of TOS, but a negative finding does not exclude its presence. These tests may also be useful in the differential diagnosis of more peripheral nerve lesions, such as median nerve compression at the carpal tunnel or ulnar nerve compression at the cubital tunnel or Guyon canal.
Nerve Conduction Velocity.
The typical findings of nerve conduction studies in patients with TOS are as follows: normal sensory and low-amplitude motor responses in the median nerve region; low-amplitude sensory and relatively low- or normal-amplitude responses in the ulnar nerve region.19,45
F-Wave Responses.
When a peripheral nerve is stimulated percutaneously and the centrally propagated (antidromic) impulse reaches the motor neuron in the spinal cord, some of the impulses will be reflected back down the axon in an orthodromic direction. This “reflected” potential is called an F wave.46 In some settings, quantitative measurements can enhance the sensitivity of this electrophysiologic response.47
Somatosensory Evoked Potentials.
Progress has been made in facilitating the objective evaluation of neurogenic TOS by recording somatosensory evoked potentials across the brachial plexus and in the supraclavicular fossa and cervical spinal cord.48,49 The most characteristic abnormality found in patients with neurogenic TOS is a reduction in the amplitude of the ulnar nerve response at the N9 electrode, or Erb’s point, or the brachial plexus recording electrode, whereas the median somatosensory evoked potential is normal. This dampening of the N9 amplitude can be accentuated, or the potential completely ablated, by placing the arm in the abducted and externally rotated position, which is the most symptomatic position for patients with TOS.
Anatomic Studies
Plain Radiography.
Plain radiographs of the cervical spine and shoulder should be obtained in all patients being evaluated for TOS to identify bony or other abnormalities that might be the cause of compression, including cervical disk disease, an abnormal first rib, a cervical rib, elongated C7 transverse processes, or shoulder pathology. Cervical ribs and long transverse processes at C7 may be the origin of radiolucent congenital bands to the first thoracic rib.22,41 Patients with a low-lying shoulder girdle have a narrow costoclavicular space. A chest radiograph should be obtained to rule out the presence of Pancoast tumor at the apex of the lung.
Computed Tomography and Magnetic Resonance Imaging.
Computed tomography (CT) scanning is not conclusively diagnostic in TOS patients. Brantigan and Roos claimed that a high-speed multidetector CT study with contrast is a promising technique because spatial resolution is much better than with magnetic resonance imaging (MRI), and the study is faster.41 Individual muscles can be visualized and peeled back using computer techniques.
MRI has also been proposed for the diagnosis of TOS because of its better visualization of soft tissues; fibrous bands and brachial plexus deviation have been shown.50 Using special sequences, Collins and others51 have performed detailed studies of the thoracic outlet with a high degree of accuracy in diagnosing TOS compression. These tests are helpful to confirm compression, but it should be noted that such compression may not necessarily be the cause of the patient’s symptoms. MRI is also useful to rule out other causes, such as tumor. Impaired venous flow at the thoracic outlet can be demonstrated by MRI without contrast medium.
Arteriography.
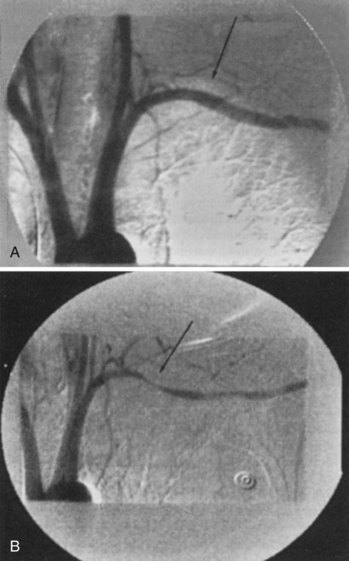
In patients with arterial thoracic outlet compression, arteriography and venography in the upper extremities should be performed in the neutral position, with the arm at the patient’s side, and in the stress position, with the upper arm at right angles to the chest. The use of digital intravenous angiography, which allows the patient to be radiographed in the sitting position, demonstrates a much higher yield of arterial compression lesions, correlating much more closely with the clinical findings (Figure 31-5). We often perform the positional exposures with the patient’s hand behind the head. If this is not done, many of the compressive abnormalities at the thoracic outlet are missed.
Venography.
Venography is indicated if venous involvement is suspected. Venograms with the patient’s arm in various positions can show intermittent occlusion or complete occlusion with collateralization (Figure 31-6). Magnetic resonance angiography is also being used for that purpose.41 Early venography combined with catheter-directed thrombolysis is indicated in a patient with acute occlusion of the axillosubclavian vein, an acutely swollen upper extremity, or when the possibility of Paget-Schroetter syndrome exists.
Provocative Tests (Scalene Muscle Block)
A newer test with high sensitivity and specificity for the diagnosis of neurogenic TOS is the electromyogram-guided selective scalene block. The method and results have been reported by Jordan and Machleder.52 Anesthetic blocks of the anterior scalene muscle have been used as a method of diagnosing and confirming TOS and for predicting which patients may benefit from surgical decompression.28 When a local anesthetic agent is injected into the anterior scalene muscle and paralyzes it temporarily, the patient’s symptoms caused by compression are relieved for a few hours to a few days. However, the standard technique of using surface landmarks often results in inadvertent somatic and sympathetic block because there is no reliable way to verify needle tip localization.19
Jordan and Machleder47,52 reported that electrophysiologic guidance facilitates accurate needle tip placement in the performance of anterior scalene muscle blocks. A Teflon-coated, 25-gauge hypodermic needle, bared at the tip, is advanced through the sternocleidomastoid muscle. Electromyographic activity is monitored as the needle is advanced through the tissue layers; the anterior scalene muscle can be activated with lateral neck bending against resistance and with deep inspiration. In most patients, a twitch of the scalene muscles is visible with electrical stimulation. The patient is asked whether pain is produced and whether insertion at this depth produces pain that is similar in quality and location to the usual pain experienced. After an injection of 2 mL of 2% lidocaine into the anterior scalene muscle, the arm is placed into a stress position and exercised for 1 minute; the patient is then asked to rate the pain. Attempts to activate the anterior scalene muscle are performed again with lateral neck movement and with deep inspiration, but only distant motor action potentials can be identified. Electrical stimulation can no longer produce a visible twitch of the scalene muscles. A positive test occurs if the patient has greater than 50% improvement in the elevated arm stress pain score after anesthetic injection of the anterior scalene muscle compared with a baseline examination. The results of these blocks correlate with surgical outcomes; a positive result predicts a good outcome to surgical decompression. Note that the absence of pain relief does not exclude the presence of TOS, as long as the patient has symptoms and clinical findings.
Differential Diagnosis
Failure to make the correct diagnosis or to appreciate the presence of other problems is a major concern in the treatment of patients with TOS.53 It is not uncommon for TOS to coexist with other conditions; in particular, lung tumors, cardiac disease, and psychiatric disorders should be considered, as well as cervical spine, neurologic, and musculoskeletal disorders.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree