Chapter 125
Thoracic Outlet Syndrome
General Considerations
Ying Wei Lum, Julie A. Freischlag
Based on a chapter in the seventh edition by Richard J. Sanders
Thoracic outlet syndrome (TOS) is a constellation of upper extremity symptoms and signs resulting from compression of the neurovascular bundle in thoracic outlet area. The three components of the bundle in the thoracic outlet area are the brachial plexus, subclavian vein, and subclavian artery. Thus there are three types of TOS, depending on which structure is compressed: neurogenic (nTOS), venous (vTOS), and arterial (aTOS). Their distinct symptoms and signs are described in Table 125-1.
Table 125-1
Comparison of the Three Types of Thoracic Outlet Syndrome

EMG, electromyography; MAC, medial antebrachial cutaneous nerve; MRI, magnetic resonance imaging; NCV, nerve conduction velocity; PTA, percutaneous transluminal angioplasty; RSI, repetitive strain injury; Rx, treatment.
Most patients with TOS are 20 to 50 years of age. Fewer than 5% are teenagers, whereas 10% are older than 50 years. Seldom is any form of TOS seen in patients older than 65. Seventy percent are female. There is no explanation for the female preponderance, but perhaps it is related to the observation that 70% of cervical ribs also occur in females.
TOS is uncommon, but its true incidence is unknown because many people with upper extremity pain and paresthesia have TOS that had escaped diagnosis by health care providers who may have failed to recognize it. nTOS is by far the most common form, accounting for more than 95% of all TOS patients. vTOS occurs in 2% to 3%, whereas aTOS is the least common, being seen in less than 1% of patients. The incidence of each type may vary depending on geography and the referral base.
History
Some of the controversies concerning TOS arise from the rich history of differing theories and concepts about the pathophysiology of this syndrome. Although cervical ribs were first described by Galen and Versalius centuries ago, it was not until 1742 that the French anatomist Francois Hunauld made the first scientific description of supernumerary ribs in humans including the cervical rib.1 Although the thoracic outlet was subsequently implicated in several descriptions of upper extremity ischemia by Sir Astley Cooper, Henry Mayo, and John Hilton, another century would go by before the first successful surgical resection of a cervical rib for relief of aTOS was described in 1861 by R.H. Coote.2 In 1860, W.H. Willshire noted the relationship between a cervical rib and paresthesias of the upper extremity.3 Similarly, the first description for vTOS was independently described during this same era by Sir James Paget and Leopold von Schroetter.4,5 Halsted is finally credited with explaining the association of cervical ribs and subclavian artery aneurysms that subsequently thrombose.6 The term cervical rib syndrome was suggested by J.B. Murphy in 1916.7
Meanwhile, neurovascular compression in the absence of a cervical rib was first suggested by F. Bramwell in 1903 and followed by the first resection of a first rib by T. Murphy in 1910.8,9 Traction for noncervical rib explanations for neurologic symptoms continued with descriptions of congenital ligaments and soft tissue bands,10 anterior scalene muscle,11,12 and middle scalene muscle13 as potential causes. It was around this time that the term scalene anticus syndrome was coined by Ochsner, who also called it Naffziger’s syndrome, thus attributing it to the surgeon who originated it.14 Finally in the 1950s, Peet et al and Rob and Standeven independently suggested the name thoracic outlet syndrome to bring together in a single term all the previous terms for syndromes marked by the constellation of clinical findings around the thoracic outlet.15,16
The later part of the 20th century was significant for developments in the surgical approach for thoracic outlet decompression. The supraclavicular exposure had been the primary approach up until this time. However, several surgeons began describing different approaches, including the posterior approach to the first rib by Clagett in 1962,17 the transaxillary approach by Roos in 1966,18 and the infraclavicular approach by Gol et al in 1968.19 Controversies regarding surgical technique concerning rib resection alone, scalenectomy alone, or rib resection in conjunction with scalenectomy continue to exist today.20,21
Anatomy
Three Spaces
Three anatomic spaces pertain to the thoracic outlet area: the scalene triangle, the costoclavicular space, and the pectoralis minor (PM) space (Fig. 125-1A). The scalene triangle (Fig. 125-1B) is the most common site of brachial plexus compression. When present, cervical ribs (Fig. 125-2) and anomalous first ribs (Fig. 125-3) also compress the plexus in this location. The costoclavicular space, between the first rib and clavicle (Fig. 125-1C) and traversed by all three structures (subclavian artery, subclavian vein, and brachial plexus), is the most common site of subclavian vein compression. The PM space is actually outside the thoracic outlet area, but compression of the upper extremity neurovascular bundle can occur in this space between the PM muscle and ribs of the chest wall. Although this might better be termed axillary compression syndrome, it is appropriate to consider the PM space as an extension of the thoracic outlet area because compression here is common and the axillary and the thoracic outlet neurovascular bundles contain the same elements (Fig. 125-4). It is this PM space that should be evaluated more carefully, particularly in patients with recurrent or persistent symptoms after initial operation for nTOS.
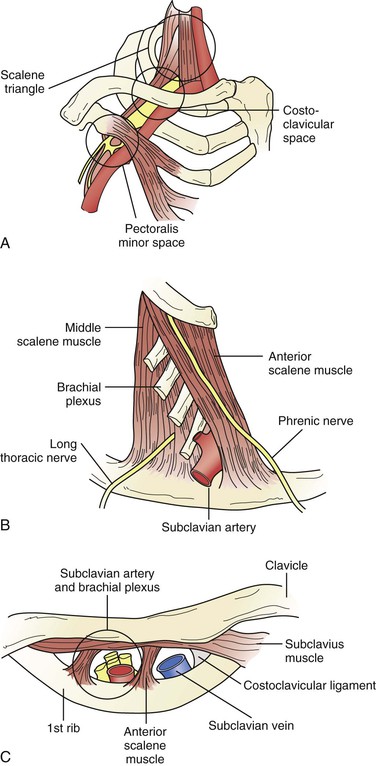
Figure 125-1 A, Anatomy of the thoracic outlet area with the three major spaces. B, Scalene triangle with the phrenic and long thoracic nerves located in the most common positions. C, Costoclavicular space revealing the subclavian vein being separated by the anterior scalene muscle from the subclavian artery and brachial plexus. (From Sanders RJ, et al: Thoracic outlet syndrome: a common sequela of neck injuries, Philadelphia, Pa, 1991, JB Lippincott.)
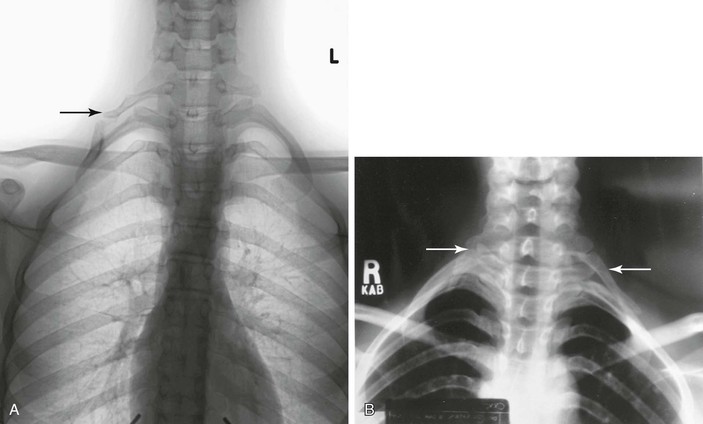
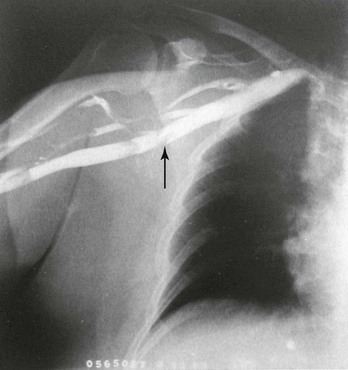
Figure 125-2 A, Right complete cervical rib (arrow) with a true joint between the cervical rib and a small process arising from the top of the first rib. B, Bilateral cervical ribs, incomplete on the right (arrow) and complete on the left (arrow). (B, from Sanders RJ, et al: Thoracic outlet syndrome: a common sequela of neck injuries, Philadelphia, Pa, 1991, JB Lippincott, p 43.)

Figure 125-3 Anomalous right first rib. That this is an anomalous first rib and not a cervical rib is demonstrated by comparing the normal first rib on the patient’s left with the abnormal rib on the patient’s right. Note the symmetry of the two second ribs. An anomalous right first rib and normal left first rib arise from the symmetric transverse processes of T1.
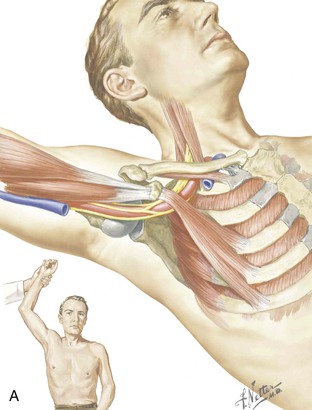
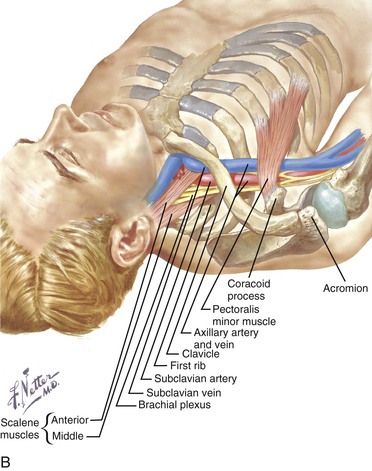
Figure 125-4 A and B, Two views of the thoracic outlet area demonstrating the pectoralis minor space in the foreground. The axillary artery and vein are continuations of the subclavian artery and vein. At the axillary level the brachial plexus has already formed its cords, so it is the branches that are seen under the pectoralis minor. (From Lord JW, Jr, et al: Thoracic outlet syndromes. Ciba Symp 23:1-13, 1971.)
Nerves
In addition to the brachial plexus, the phrenic and long thoracic nerves are seen during supraclavicular dissections. Very close to the area, but rarely seen, are the dorsal scapular nerve and cervical sympathetic chain.
Brachial Plexus
The brachial plexus arises from nerve roots C5 to T1. In the scalene triangle area, the five nerve roots become three trunks. The anterior and posterior divisions and cords of the plexus are usually formed proximal to the PM space, so it is the branches of the plexus that lie under the PM muscle, along with the axillary artery and vein.
Phrenic Nerve
Arising primarily from C4, the phrenic nerve usually receives branches from C3 and C5. It is single in 87% and double or triple in 13% of individuals. A double phrenic nerve usually results from the C5 branch to the phrenic nerve’s failing to fuse with the C4 branch in the neck. It may fuse below the clavicle or in the mediastinum. The phrenic descends 84% of the time from the lateral to the medial side of the anterior scalene muscle. In the other 16% the phrenic nerve remains on the lateral side.22 Each phrenic nerve accounts for 20% of the breathing capacity. In neck dissections, a helpful landmark is that the nerve lies just below the transverse cervical artery.
Long Thoracic Nerve
The long thoracic nerve arises primarily from C6 and usually receives contributions from C5 and C7. The C5 and C6 branches run through the muscle belly of the middle scalene muscle, where they can usually be observed to join. The C7 branch arises from the posterior aspect of the nerve root and often descends below the middle scalene before joining the other two branches.
Dorsal Scapular Nerve
The dorsal scapular nerve, the first branch of C5, courses through the cephalic portion of the middle scalene muscle and then descends lateral to the muscle. However, it may course very close to the area of dissection in supraclavicular approaches to thoracic outlet decompression.
Cervical Sympathetic Chain
Though not usually in the operative field of supraclavicular procedures, the cervical sympathetic chain lies over the transverse processes of the cervical vertebrae and is therefore very close to the origin of the anterior and middle scalene muscles. As a result, when cautery is used to excise the scalene muscles at their transverse process origins, the current may reach and damage the cervical sympathetic chain. This is the probable explanation for the occasional case of Horner’s syndrome observed after supraclavicular scalenectomy. Since we have stopped excising scalene muscles all the way to bone, we no longer are seeing Horner’s syndrome. Use of bipolar cautery can reduce the incidence of this complication but does not totally eliminate it.
Scalene Muscle Variations and Anomalies
A significant number of anatomic variations in scalene muscles have been observed both in the normal population and in patients with nTOS. They are too common to be called anomalies. These variations might be regarded as factors predisposing to TOS but are not regarded as causes.
Splitting of the Anterior Scalene around C5 and C6.
Such splitting was noted in 45% of cadavers and in only 21% of nTOS patients.22
Scalene Minimus Muscle.
This muscle arises from the transverse processes of the lower cervical vertebrae, runs in front of C8 and T1 and behind the subclavian artery, and inserts on the first rib or Sibson’s fascia. Its incidence is 25% to 55%.23
Interdigitating Muscle Fibers.
Such fibers commonly run between the anterior and middle scalene muscles. They were noted in 75% of nTOS patients and in only 40% of cadavers.
Scalene Triangle Width.
The width of the scalene triangle varies from very narrow to quite wide, with the distance between the two scalene muscles at their insertion on the first rib ranging from 0.3 to 2.0 cm. The nerve roots emerge lower in a wide triangle than in a narrow triangle (Fig. 125-5). Observations during surgery have revealed that most nTOS patients have the narrower type of triangle.22

Figure 125-5 Scalene triangle variations. A, The usual relationships found in cadavers. The triangle is wider and the nerves emerge lower in the triangle than in most patients with neurogenic thoracic outlet syndrome. There is minimal contact between nerve and muscle. B, A narrow triangle in which the nerves emerge high and are touching the muscles as they emerge. Contact between nerve and muscle is stronger than in A. (From Sanders RJ, et al: The surgical anatomy of the scalene triangle. Contemp Surg 35:11-16, 1989.)
Congenital Bands and Ligaments.
These structures are frequently observed in the normal population, with an incidence as high as 63%.24 Although bands have been observed in almost every area of the scalene triangle and have been nicely classified,25 their role is as a predisposing factor rather than a direct cause (Table 125-2).
Table 125-2
Classification of Congenital Bands and Ligaments within the Scalene Triangle25
| Type | Description |
| 1 | Extends from the anterior tip of an incomplete cervical rib to the middle of the first thoracic rib; inserts just posterior to the scalene tubercle on the upper rib surface |
| 2 | Arises from an elongated C7 transverse process in the absence of a cervical rib and attaches to the first rib just behind the scalene tubercle; associated with extension of the transverse process of C7 beyond the transverse process of T1 on anteroposterior spine radiographs |
| 3 | Both originates and inserts on the first rib; starts posteriorly near the neck of the rib and inserts anteriorly just behind the scalene tubercle |
| 4 | Originates from a transverse process along with the middle scalene muscle and runs on the anterior edge of the middle scalene muscle to insert on the first rib; the lower nerve roots of the brachial plexus lie against this band |
| 5 | Scalene minimus muscle arises with the lower fibers of the anterior scalene muscle, runs parallel to this muscle but passes deep to it to cross behind the subclavian artery and in front of or between the nerve roots, and inserts on the first rib; any fibers passing anterior to or between the plexus but posterior to the artery |
| 6 | Scalene minimus muscle inserting onto Sibson’s fascia over the cupula of the pleura instead of onto the first rib; labeled separately to distinguish its point of insertion |
| 7 | Fibrous cord running on the anterior surface of the anterior scalene muscle down to the first rib and attaching to the costochondral junction or sternum; lies immediately behind the subclavian vein, where it may be a cause of partial venous obstruction |
| 8 | Arises from the middle scalene muscle and runs under the subclavian artery and vein to attach to the costochondral junction |
| 9 | Web of muscle and fascia filling the inside posterior curve of the first rib and compressing the origin of the T1 nerve root |
Relationship of the Subclavian Vein to the Phrenic Nerve.
The phrenic nerve usually runs posterior to the subclavian vein. However, in 5% to 7% of individuals the phrenic nerve runs anterior to the vein and in this position can be a rare cause of subclavian vein obstruction (Fig. 125-6).26 A case of this is seen in Figure 125-7. This patient was treated by dividing the subclavian vein, letting the nerve fall behind the vein, and anastomosing the vein anterior to the nerve.
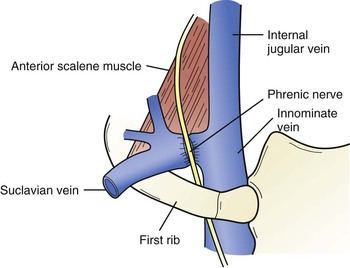
Figure 125-6 Prevenous phrenic nerve lying anterior to the subclavian vein and compressing it. This occurs in 5% to 7% of cases. (From Sanders RJ, et al: Thoracic outlet syndrome: a common sequela of neck injuries, Philadelphia, Pa, 1991, JB Lippincott, p 241.)
Relationship of the Subclavian Vein and Costoclavicular Ligament.
The subclavian vein lies on top of the first rib just before it is joined by the jugular vein. It is touched medially by the costoclavicular ligament and superiorly by the subclavius tendon. A variation in the position of the vein is its position a little more medially on the first rib so that it is partially compressed by the costoclavicular ligament. Variations in the thickness of the subclavius tendon can also result in compression of the vein from above. These variations in position between the three structures predispose to the development of subclavian vein obstruction. Obstruction is then caused by excessive overhead use of the upper extremity, which results in the vein’s being repeatedly pushed against the ligament or tendon (or both) and the first rib (Fig. 125-8).
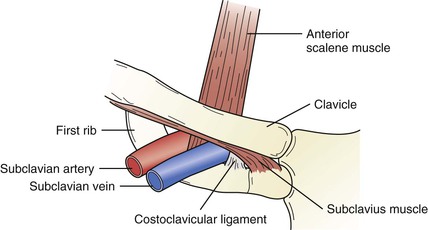
Figure 125-8 Anatomy of the subclavian vein and ligaments. The subclavian vein is in close contact with the costoclavicular ligament, subclavius tendon, and anterior scalene muscle because it lies on the first rib. (From Sanders RJ, et al: Thoracic outlet syndrome: a common sequela of neck injuries, Philadelphia, Pa, 1991, JB Lippincott, p 236.)
Cervical Ribs and Anomalous First Ribs
Incidence
Anomalous or rudimentary first ribs are often overlooked on routine chest radiographs. The first report was a 1939 study of 5000 chest radiographs. This study found the incidence of anomalous first ribs and cervical ribs to be 0.76% and 0.74%, respectively. Anomalous ribs occurred equally in women and men. In contrast, the female-male ratio of cervical ribs was found to be 7 : 3.27 No one has yet provided an explanation for this difference.
Both ribs are narrower and lie higher than a normal first rib. The only difference between the two is that a cervical rib arises from the transverse process of C7, whereas an anomalous first rib arises from the transverse process of T1 (see Fig. 125-4). It is more than of academic interest to note the distinction between anomalous and cervical ribs. It is common to excise the first rib with the cervical rib. However, if the rib is an anomalous first rib, the second rib below it should not usually be removed. There is one exception: if the anomalous first rib is so fused to the second rib that the second rib is significantly thinned and deformed when removing the anomalous first rib, excision of the second rib is justified.
Complete versus Incomplete Cervical Ribs
About 30% of cervical ribs are complete ribs fused to the first rib by a true joint or a fibrous attachment. The other 70% are incomplete cervical ribs with no direct attachment to the first rib. However, most of these incomplete ribs have a tight fascial band extending from the tip of the cervical rib to the first rib.25 The cervical rib and attached band lie within the middle scalene muscle, thereby narrowing the space within the scalene triangle through which the nerve roots of the plexus must pass. Thus an incomplete cervical rib with its band can act like a complete rib.
Significance
Cervical and anomalous first ribs can push against the subclavian artery and cause stenosis with or without poststenotic aneurysm formation, or more often, they will push against the lower trunk of the brachial plexus and cause a neuropathy. However, most cervical and anomalous first ribs remain asymptomatic throughout life. When symptoms do develop, they are usually neurogenic. In a recent review of 47 nTOS operations involving abnormal ribs, 15% were anomalous first ribs and 85% were cervical ribs. Spontaneous onset of symptoms occurred in 50% of patients with complete cervical ribs versus only 20% with incomplete ribs. Neck trauma preceded the onset of symptoms in the other 80% with incomplete ribs and in the 50% with complete ribs.28
Association with Arterial and Neurogenic Thoracic Outlet Syndrome
Cervical ribs or anomalous first ribs are almost always seen in patients with aTOS. On the other hand, symptomatic cervical ribs are more likely to produce symptoms of nTOS than aTOS. Over a 28-year period during which more than 1000 nTOS operations were performed, there were 39 cervical ribs and 7 anomalous first ribs, for an incidence of about 4%. Among the same group of 1000-plus TOS patients, there were only nine with aTOS—five with complete cervical ribs and four with anomalous first ribs—for an incidence of less than 1%.28
Objective Findings
Ulnar neuropathy on electrodiagnostic studies and hand atrophy occur in only a small minority of patients with cervical ribs and nTOS symptoms. Both were present in only 3 of 39 patients (8%) in one study28 and were noted in 8 of 45 patients (18%) in another.29 Improvement in symptoms and signs after surgery is the same in patients with cervical ribs as in those without. In the few patients with cervical ribs and hand atrophy, the neurologic deficit persisted after surgery in more than half.29
Pathogenesis
Etiology
The most common cause of nTOS is neck trauma that involves a hyperextension neck injury. Whiplash in a motor vehicle accident is the most common injury. Other frequent causes are repetitive stress injuries in the workplace and falls on slippery floors or icy walkways.
vTOS is most often the result of developmental anomalies of the costoclavicular space and repetitive arm activities such as throwing, swimming, or working with the arms overhead for long periods.
aTOS is usually associated with a cervical or anomalous first rib or, rarely, an anomalous insertion of the anterior scalene muscle. Symptoms and signs are the result of arterial emboli arising from subclavian artery aneurysms or stenosis that resulted from the abnormal rib.
Predisposing Factors
These syndromes result from a combination of developmental anomalies in the thoracic outlet and physical activities and life events that predispose individuals to become symptomatic. In nTOS, predisposing factors include scalene muscle anomalies, narrow scalene triangles, congenital ligaments or bands, roots of the plexus arising high near the apex of the scalene triangle, and cervical ribs. A common initiating event is neck trauma, which causes symptoms in patients with developmental anomalies of the thoracic outlet. All patients with cervical ribs are predisposed to the development of some form of TOS, most commonly nTOS. In such patients, neck trauma may precipitate symptoms, but in some patients with no history of trauma, the rib and arm activities of daily living can cause nTOS.
In vTOS, the predisposition is the relationship of the subclavian vein to the subclavius tendon and costoclavicular ligament and dimensions of the costoclavicular space. In most patients with vTOS, the subclavian vein lies tightly against the costoclavicular ligament, and the subclavius tendon is compressing the top of the vein within a narrowed costoclavicular space. With the vein in this compressed position, repetitive arm movements can easily traumatize the vein and produce fibrosis, stenosis, and eventually thrombosis.
In aTOS, symptoms may be caused by a cervical or anomalous first rib, developmental anomalies of the anterior scalene muscle, and activities of daily living.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree