Fig. 8.1
Aortic arch and its branches. IA innominate artery, RScA right subclavian artery, VA vertebral artery, RCCA right common carotid artery, LCCA left common carotid artery, LScA left subclavian artery
The innominate artery is the first and largest arch branch. It arises near midline, anterior to the trachea, and courses gently to the right. Just below the base of the right neck, it bifurcates to form the right subclavian and right common carotid arteries.
The left common carotid artery is typically the second branch from the aortic arch. Arising immediately after the innominate artery, it also originates in front of the trachea and curves gently toward the left side of the neck. Both the innominate and left common carotid arteries start near midline, and then curve gently laterally. The common carotid arteries course to the right and left of midline, where both right and left common carotid arteries approach the carotid bifurcation in a posterior position on either side of the trachea.
The left subclavian artery is the third arch branch, ascending toward the neck but bending laterally to course through the thoracic outlet. In some, the right subclavian artery may originate from the innominate slightly higher in the chest to take a more downward projection to enter the thoracic outlet.
The arch rises in the superior mediastinum fairly high in the chest, but lies protected by the sternum. The truncal branches also arise behind the sternum and sternoclavicular joints at about the level of the third and fourth thoracic vertebrae. This protected position makes a direct transthoracic ultrasonic approach to the arch impossible.
The basic branch anatomy is shared by two thirds (65%) of the population [7], and the remaining one third has a variant anatomy. The most frequent variant lies in a common origin shared by the innominate and left common carotid arteries, the so-called brachiocephalic branch or bovine configuration, which occurs in 27% of the population. Much less frequently, the vertebral artery originates from the aorta between the left common carotid and the left subclavian arteries (2–6% of cases). Rarely (less than 1%), the right subclavian artery originates from the arch distal to the left subclavian, or the right vertebral originates from the right common carotid artery or the arch.
Brachiocephalic Veins
The central veins demonstrate greater symmetry than the supra-aortic arteries (Fig. 8.2). The internal jugular veins of the neck and subclavian veins from the upper extremities are confluent, forming the right and left brachiocephalic veins. The external jugular veins also drain into the subclavian veins bilaterally, near the originations of the brachiocephalic veins. The right and left brachiocephalic veins converge to form the superior vena cava (SVC) at about the level of the aortic arch. The SVC lies to the right of the arch, causing a bit of asymmetry. The right brachiocephalic vein descends directly into the SVC as a short venous segment, but the left brachiocephalic vein is longer and sharply angulated because of the position of the SVC. The left brachiocephalic vein courses obliquely from the left internal jugular (IJ) vein to the right chest, lying anterior to the branch arteries of the arch. Both brachiocephalic veins converge to form the superior vena cava. Approximately 7 cm in length, the SVC is in contact with the pleura of the right lung, the trachea, and aorta. There are no valves in the brachiocephalic trunks or SVC.
Fig. 8.2
Brachiocephalic veins and superior vena cava. RScV right subclavian vein, RIJV right internal jugular vein, RBcV right brachiocephalic vein, LBcV left brachiocephalic vein, LScV left subclavian vein, LIJV left internal jugular vein, SVC superior vena cava
Imaging the Aortic Arch and Brachiocephalic Veins
The arch and branches are a neglected area that is seldom imaged with ultrasound because of dense ultrasound reflections produced by bone and lung air. It is, however, described as part of a standard echocardiographic assessment made through a suprasternal approach [8].
The suprasternal notch is the midline depression that lies at the base of the neck, between the sternum and larynx. Echocardiography uses the notch to visualize the ascending aorta, arch, and descending thoracic aorta as a means for evaluating the aorta for valvular insufficiency, dissection, aneurysm, or coarctation [9]. Though it is described as a standard echo approach, the image is often less than satisfactory and is seldom used in adult echo.
The echocardiographer uses a 2–5 MHz transducer to visualize the ascending aorta, arch, and descending aorta. The transducer produces a small footprint for the more superficial arch branches and is less suited for branch vessel assessment. For the neck, vascular sonographers use high-frequency (5–10 MHz) linear probes to image the extracranial cerebrovascular branches at the carotid bifurcation. The examination approaches the cervical carotid arteries from the lateral neck, alongside the sternocleidomastoid muscle. The scan typically ends centrally at the right common carotid origin and left common carotid artery at the neck base.
As a compromise, the midline, suprasternal approach should be our approach to the supra-aortic vessels, using a low-frequency curvilinear probe rather than the small footprint echo or the high-frequency linear probe. The obvious drawbacks to imaging the arch and its branches from this angle include the following: (1) Interference from the sternum and claviculae which severely limits access. The ultrasound beam is projected downward through a narrow acoustic window which limits the anterior-posterior projection by the sternum and neck. (2) The truncal arteries project directly toward the probe, and veins project directly away from the probe. The resulting B-mode echoes are weakly reflective and poorly illuminate the walls of the central branches. (3) Color Doppler compensates for the weak B-mode image, but the number of large vessel flows and color artifacts picked up from the bright echoreflective surfaces of the mediastinum and pleura produce a confusing image with large swaths of color.
To overcome these problems, recognizing the anatomy of the arch and brachiocephalic veins is important to scanning the central vessels. It is also important to maintain an orientation that is based upon the known ultrasonic anatomy. The examination can be performed by first placing the curvilinear transducer above the sternum and positioning the probe to produce a panoramic view of both common carotid arteries and internal jugular veins at the base of the neck (Fig. 8.3). With this view as the reference point, the scan can be extended centrally by gray scale and color. The right common carotid artery will be seen to rapidly converge with the subclavian artery to become the innominate artery. On the left, the common carotid artery will be seen to simultaneously continue uninterrupted toward the arch. As the probe is projected centrally, both the innominate and left common carotid arteries will approach one another. The larger innominate artery will approach midline from the patient’s right, and the left common carotid artery will course obliquely from the left. From further left, the left subclavian artery will course toward the arch from the clavicle.
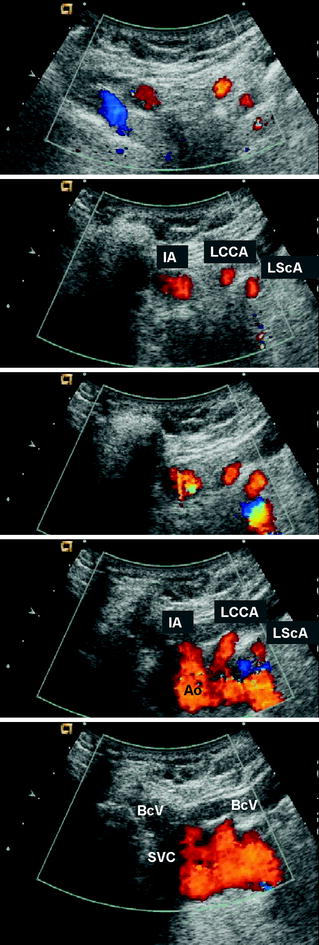
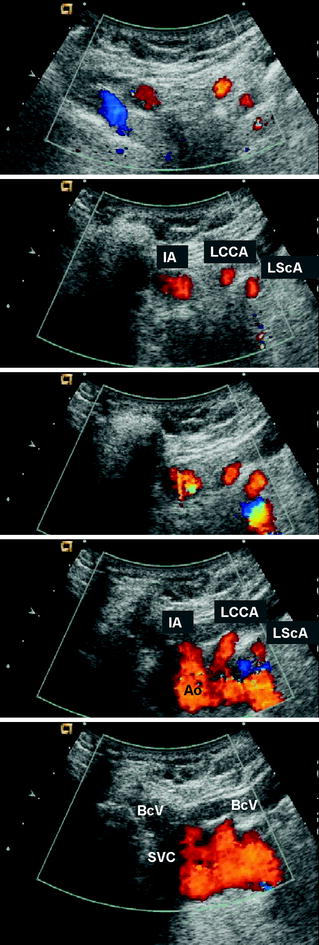
Fig. 8.3
Imaging the aortic arch and its branches. Branches of the arch from the neck base (top) to aorta (bottom) are scanned with a 4-MHz curvilinear probe placed horizontally above the suprasternal notch. The innominate artery (IA), left common carotid artery (LCCA), and left subclavian artery (LScA) are shown in oblique slices. Scanning centrally, the supra-aortic branches enter the aorta (Ao). With greater probe angulation (bottom), the convergence of the right and left brachiocephalic veins (BcV) can be imaged to form the superior vena cava (SVC). The right sternoclavicular joint produces an acoustic shadow alongside the SVC
The arteries and veins of interest lie in front of the trachea. Because the arch projects obliquely from right to left and anterior to posterior, the probe positioned for a transverse view of the innominate and left common carotid arteries will also capture the aorta in near transverse. The aorta will be seen in gray scale as a 2−3-cm pulsatile mass. By color, flow in the aorta will be notably disturbed. Flow in the innominate and left common carotid will be much more uniform and easily traced as tracks of color flow directed toward the probe. Both arteries can be interrogated by spectral Doppler as they approach the aorta.
Once the relative positions of the arteries are identified, the innominate artery (Fig. 8.4) and left common carotid artery (Fig. 8.5) may be imaged individually in the longitudinal view by rotating the ultrasound probe on the neck base to the left of midline.
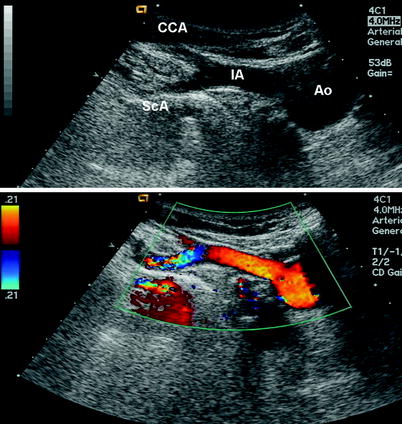
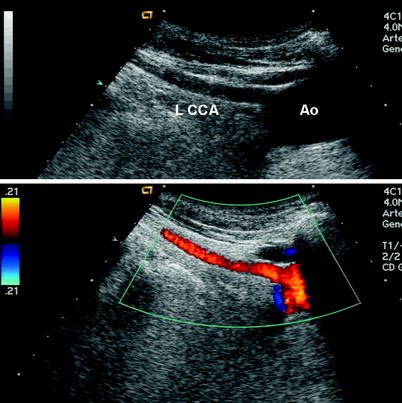
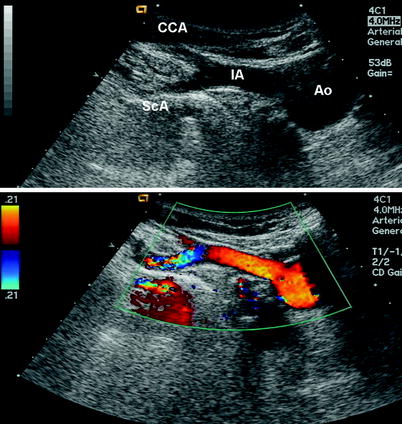
Fig. 8.4
Longitudinal view of the innominate artery from the aorta (Ao) to the innominate artery (IA), right common carotid artery (CCA), and right subclavian artery (ScA), using a 4-MHz curvilinear probe. The probe is placed toward the left of midline. A shadow is cast from the left clavicle at the sternoclavicular joint. A mirror imaging reverberation artifact can be noted below the bright reflector and right subclavian artery
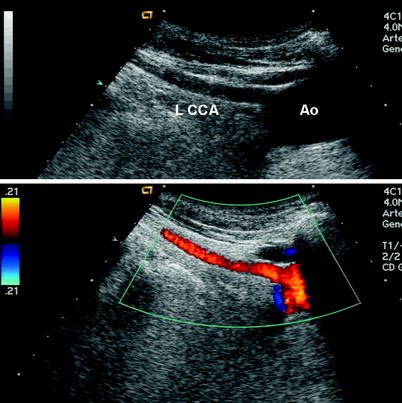
Fig. 8.5
Longitudinal view of left common carotid artery (LCCA) and aorta (Ao) scanned with a 4-MHz curvilinear probe, demonstrating origin of the left common carotid artery, internal jugular vein, and shadowing from the sternoclavicular joint
The left subclavian artery may be the most difficult to follow. To visualize the subclavian, the transducer probe will be positioned above the clavicle, projecting the heel of the probe toward the left posterior aspect of the notch (Fig. 8.6). Ultrasound reflections will capture bright reflections from the pleura and left lung. Artifactual duplication of the left subclavian artery by B-mode and color could then result from mirror imaging reverberation (Fig. 8.6).
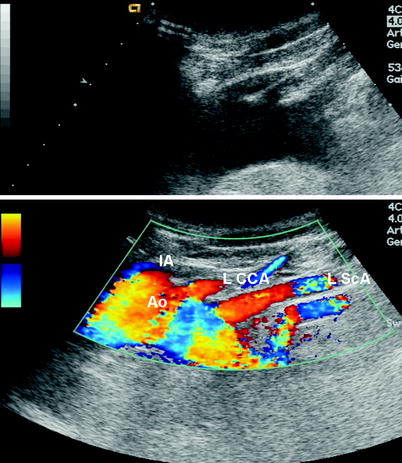
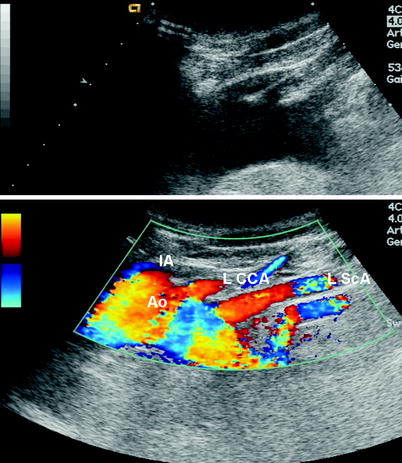
Fig. 8.6
Longitudinal view of left subclavian artery (LScA) and originations of left common carotid artery (LCCA) and innominate artery (IA) from the aorta (Ao). A mirror imaging reverberation artifact can be noted below the bright reflector and left subclavian artery
The subclavian artery should be identified as the color flow pattern that lies superficial to any color artifact. To avoid further confusion, the left subclavian artery could be followed from the axillary artery, below the clavicle, through the thoracic outlet to the subclavian artery.
Difficulties in imaging may be associated with configuration of the arch. The arch has been described in coiled and uncoiled configurations with the supra-aortic trunks originating from different points of the arch [10]. The better configuration positions the innominate on the right edge of the apex, and the left subclavian on the left edge. The take-off points, located on the superior wall of the arch, are optimally positioned for ultrasound imaging and endovascular cannulation. The more difficult imaging configuration occurs when the innominate artery arises from the aorta, before the apex, and its origin lies below the level of the apex. In this “uncoiled” position, the left common carotid and subclavian arteries may be similarly displaced to the right. The deeper take-off of the innominate may prevent adequate ultrasonic visualization as well as increase the difficulty of endovascular cannulation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


