The right atrium (
RA) receives venous blood returning from the upper body (via the superior vena cava,
SVC), the lower body (via the inferior vena cava,
IVC) and also from the myocardium (via the coronary sinus). It can best be seen in:
Right atrial size
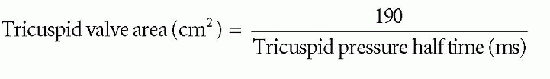
Assessment of
RA size can be challenging in view of the difficulty in imaging it clearly. In an apical 4-chamber view you can simply ‘eyeball’ the relative sizes of the left and right atria. The
RA is normally no larger than the left – if it is larger, it is dilated.
To quantify
RA size, in the modified apical 4-chamber view at end-diastole measure the
RA minor axis from the lateral wall of the
RA to the interatrial septum (perpendicular to the
RA major axis,
Fig. 21.1).
A RA minor axis >4.4 cm or a
RA major axis >5.3 cm is indicative of
RA dilatation. Alternatively, perform planimetry
of the
RA in the modified apical 4-chamber view – a dilated
RA is indicated by an area >18 cm
2. Calculation of
RV volume is
not recommended as there are few data on normal ranges.
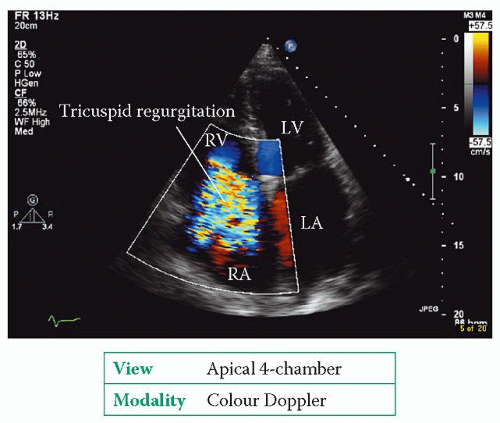
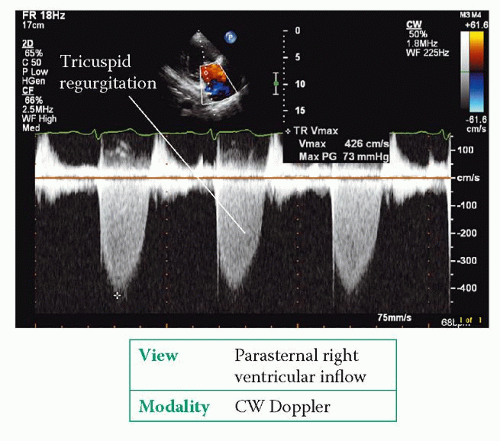
RA dilatation can result from
RA pressure overload (e.g. pulmonary hypertension, restrictive cardiomyopathy, tricuspid stenosis),
RA volume overload (e.g. tricuspid regurgitation,
ASD) and chronic atrial fibrillation (
AF).
Right atrial pressure
There are a number of ways of assessing
RA pressure (
RAP):
1. The
RAP can be gauged by examining the patient’s neck to assess their jugular venous pressure (
JVP) – with the patient reclining supine at 45°, the height of the
JVP above the sternal angle (in cm) is the same as
RAP (in mmHg). However, the height of the
JVP can be tricky to assess, particularly if the
JVP is not clearly visible or if it is very high or low.
2.
A ‘constant’ value of 10 mmHg can be ‘assumed’ as the
RAP. However,
RAP does vary, and so using a ‘constant’ value is rather a blunt instrument and can be potentially misleading.
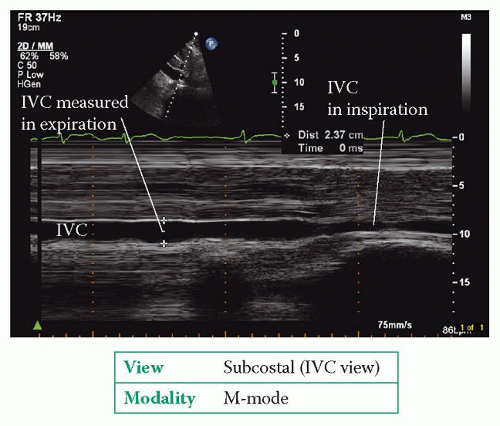
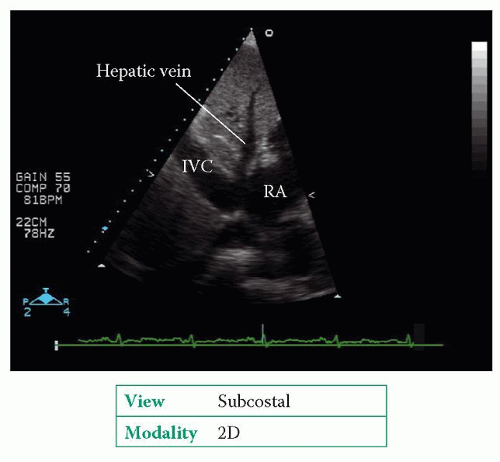
3. The
RAP can be estimated measuring the
IVC diameter in both expiration and inspiration, using the subcostal window (
Fig. 21.2). Normally the
IVC measures 1.5-2.5 cm in diameter and decreases by >50 per cent in inspiration. The data in
Table 21.1 will allow you to place an approximate value on
RAP. For example, if the
IVC measures 2.8 cm in expiration and 1.8 cm in inspiration, a reduction of 36 per cent, the
RAP would be estimated at 15-20 mmHg.
4. The American Society of Echocardiography recommends using absolute values for
RAP rather than ranges, thus:
a. an
IVC measuring ≤2.1 cm which collapses by >50 per cent on inspiration indicates an
RA pressure of 3 mmHg
b. an
IVC measuring >2.1 cm that collapses by <50 per cent on inspiration indicates an
RA pressure of 15 mmHg
c. an intermediate
RA pressure of 8 mmHg may be used in situations outside these parameters (or other indicators of
RA pressure can be used).
One further indicator of
RAP is
RA size, which is usually normal when
RAP is ≤10 mmHg, but becomes dilated at pressures above this (and, in general, the higher the
RAP, the greater the dilatation). Similarly, the hepatic veins become increasingly dilated as
RAP rises above 15 mmHg.
Eustachian valve and Chiari network
Where the
IVC enters the
RA there is often an embryological remnant, the
Eustachian valve, which in fetal life directs oxygenated blood away from the tricuspid valve and towards the foramen ovale. The Eustachian valve can remain prominent in adult life and is a normal finding, but can be mistaken for a mass, thrombus or vegetation.
Similarly, a
Chiari network is a fetal remnant and appears as a web-like structure extending into the
RA with an attachment near the RA-IVC junction. It is present in around 2 per cent of the population as a normal variant but can be mistaken for a more sinister lesion.
Usually neither a prominent Eustachian valve nor a Chiari network is of any clinical significance, although there is some evidence that either remnant in combination with a patent foramen ovale may increase the risk of paradoxical (right-to-left) embolism.