4 The Laboratory
Equipment
 Design of the Facilities and Equipment
Design of the Facilities and Equipment
Standards for cardiac catheterization laboratories have been published. The catheterization laboratory must be in close proximity to a cardiac care unit or an intensive medical unit and have sufficient space (≥ 30 m2). The following equipment should be present in the catheterization laboratory:
 Defibrillator with battery operation
Defibrillator with battery operation
 Temporary pacemaker
Temporary pacemaker
 Emergency medications in sufficient amounts
Emergency medications in sufficient amounts
 Capabilities for artificial ventilation as well as oxygen and compressed air supply
Capabilities for artificial ventilation as well as oxygen and compressed air supply
 Blood gas analyzer
Blood gas analyzer
 Pulse oximetry
Pulse oximetry
 Suction
Suction
 Operating lights
Operating lights
 Emergency power generator for the cardiac catheterization room, control room, and recovery room
Emergency power generator for the cardiac catheterization room, control room, and recovery room
For some specific techniques such as high-frequency rotablation, sufficient access to pressurized air (140 L/min, at least 650 kPa [6.5 bar]) is required. For complex interventions, in cooperation with anesthesia and cardiac surgery, wall connectors for oxygen and pressurized air to run the anesthesia apparatus should be available.
 Angiography System
Angiography System
Although the basic layout of a catheterization system has changed little over time (layout of a modern biplane catheterization laboratory; Fig. 4.1), there have been substantial technical improvements in recent years, especially with regard to the following:
 Significantly improved X-ray utilization through improvements in tube technology
Significantly improved X-ray utilization through improvements in tube technology
 More efficient use of photons by the image intensifier, with improved contrast resolution
More efficient use of photons by the image intensifier, with improved contrast resolution
 Transition to digital technology in both imaging and recording of hemodynamic data
Transition to digital technology in both imaging and recording of hemodynamic data
 A comfortable, easily movable patient table, which has to be accessible from all sides (especially in the case of resuscitation)
A comfortable, easily movable patient table, which has to be accessible from all sides (especially in the case of resuscitation)
 Stand with image intensifier/flat panel detector and Xray tube
Stand with image intensifier/flat panel detector and Xray tube
 X-ray generator with tube
X-ray generator with tube
 Image intensifier for image recording (if possible three input formats; zoom) or alternatively a flat panel detector for image recording
Image intensifier for image recording (if possible three input formats; zoom) or alternatively a flat panel detector for image recording
To be able to evaluate the heart from different projections, the X-ray tube and image intensifier have to be movable (rotation range ± 90°; angulation range ± 40°). Particularly for interventions, a biplane system has the advantage that it allows simultaneously different projections for fluoroscopy and image documentation and thus saves both contrast media and time. Alternatively, modern single-plane systems with the possibility for rotational angiography can be used.
Image transmission occurs via an image intensifier–television combination or flat panel technology. At least one monitor per plane is required in the catheterization room and the control room (diagonal diameter of the monitors in the catheterization room should be at least 44 cm). In the catheterization laboratory there is an additional monitor per plane to save and display a reference image. Additional monitors are required to show the hemodynamic data. Ideally, another monitor should be available for imaging external data (echocardiography or three-dimensional mapping system for electrophysiological interventions).
For interventional cardiology additional specific requirements were made for the catheterization system (Table 4.1).
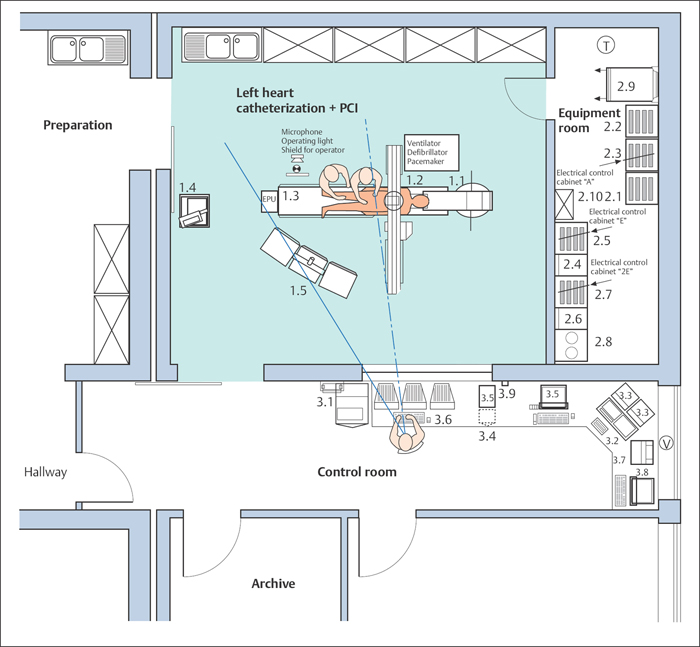
Fig. 4.1 Layout of a modern biplane cardiac catheterization laboratory.
(Cardiac catheterization system)
1 | Procedure room |
1.1 | Stand frontal plane |
1.2 | Stand lateral plane |
1.3 | Patient table |
1.4 | Contrast medium power injector |
1.5 | Monitors/ceiling-mounted monitor support |
2 | Equipment room |
2.1 | Control cabinet geometry |
2.2 | Control cabinet image intensifier/TV |
2.3 | Control cabinet system |
2.4 | High-voltage generator 1 |
2.5 | Control cabinet generator 1 |
2.6 | High-voltage generator 2 |
2.7 | Control cabinet generator 2 |
2.8 | Control cabinet |
2.9 | Computer cabinet |
2.10 | Cabinet for service documentation |
3 | Control room |
3.1 | Control console |
3.2 | Analysis console |
3.3 | Control monitor |
3.4 | View station for external media |
3.5 | Video recorder |
3.6 | Hemodynamic recording system |
3.7 | Video printer |
3.8 | Computerized hospital information system |
3.9 | ISDN/DSL network connection |
Table 4.1 Specific requirements for the catheterization system for interventional applications
– Extended protection against radiation at the patient table – Automatic angle adjustment or automatic angle display – Generator power ≥ 100 kW, continuous power > 2 kW – Source image distance (SID) tracking (automatic dose regulation with subsequent reduction of the tube current with reduction of the focal spot–image intensifier distance) – Last image hold (“freeze frame”) or last image run (storage image), two monitors per plane – Roadmapping: device-based orientation aid for catheter direction during interventions – Pulsed fluoroscopy, pulse width (1–10 ms, selectable), frame rates (3–25/s, selectable) – Additional filters for fluoroscopy of at least 0.1 to 0.5 mm Cu equivalent, special grid (mm ≤ 1.8) – Aperture system (iris diaphragm, for overframing rectangular and semitransparent diaphragm) – Image intensifier with at least three input formats (e.g., 13, 17, and 23 cm) |
Image Recording
Digitized recording of coronary angiography and hemodynamic data is now standard. Digital image quality is determined by matrix size and depth. For example, a 512 × 512 matrix consists of 512 rows and 512 columns and thus 262,144 pixels (minimum requirement for coronary angiography.) The image depth is expressed in bits. Eight bits allow visualization of 28 = 256 gray scale divisions, whereas 10 bits allow 1,024 gray scale divisions.
Hence, for a 512 × 512 matrix with an image depth of 8 bits (where 8 bits = 1 byte) the data amount per image is 512 × 512 × 1 byte = 262,144 bytes, which is 256 kilobytes (where 1 kilobyte = 1,024 bytes). The major advantages of digital imaging and digital storage are as follows:
 Immediate availability of images
Immediate availability of images
 Higher image quality, e.g., significantly increased image contrast
Higher image quality, e.g., significantly increased image contrast
 The possibility of image processing (automatic/manual) → higher image quality, diagnostically more conclusive
The possibility of image processing (automatic/manual) → higher image quality, diagnostically more conclusive
 Image recording in real-time, no data loss
Image recording in real-time, no data loss
 The availability of digital analysis possible (electronic measurements, automatic contour recognition of the ventricles, etc.)
The availability of digital analysis possible (electronic measurements, automatic contour recognition of the ventricles, etc.)
 Cost-saving and space-saving digital storage of the images (1 CD/patient → an unlimited number of patients depending on the server configuration when using a picture archiving and communication system)
Cost-saving and space-saving digital storage of the images (1 CD/patient → an unlimited number of patients depending on the server configuration when using a picture archiving and communication system)
 The ability to transit images via digital data networks
The ability to transit images via digital data networks
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


