The Athlete and the Heart
Antonio B. Fernandez, MD
Paul D. Thompson, MD
 ESSENTIALS OF DIAGNOSIS
ESSENTIALS OF DIAGNOSIS
![]() The patient has an extensive history of exercise training
The patient has an extensive history of exercise training
![]() There may be profound sinus bradycardia, sinus arrhythmias, or atrioventricular conduction delays at rest that disappear with exertion.
There may be profound sinus bradycardia, sinus arrhythmias, or atrioventricular conduction delays at rest that disappear with exertion.
![]() The athlete’s heart may demonstrate four-chamber enlargement and mild left ventricular hypertrophy, but normal diastolic function and B-natriuretic peptide levels. The diastolic wall-to-volume ratio should be < 0.15 mm/m2/mL by magnetic resonance imaging.
The athlete’s heart may demonstrate four-chamber enlargement and mild left ventricular hypertrophy, but normal diastolic function and B-natriuretic peptide levels. The diastolic wall-to-volume ratio should be < 0.15 mm/m2/mL by magnetic resonance imaging.
![]() Morphologic changes reverse with detraining.
Morphologic changes reverse with detraining.
 General Considerations
General Considerations
The salutary physiologic effects of exercise training on the cardiovascular system have been studied extensively, but intense exercise training can produce cardiac adaptations that mimic pathological conditions. Consequently, clinicians should be aware of the normal cardiac structural and functional responses to exercise training in order to distinguish these changes from clinical disease that could also affect athletes.
A. Physiology of Exercise Training
The “athlete’s heart” refers to the normal structural and physiologic cardiac adaptations to exercise training. Clinical characteristics of the athlete’s heart include resting sinus bradycardia (occasionally profound), sinus arrhythmia, atrioventricular (AV) conduction delays, systolic flow murmurs, four-chamber enlargement, and an increase in cardiac mass, but usually normal or augmented ventricular systolic function.
The magnitude of these cardiac changes depends on a variety of factors including the duration and intensity of the exercise training, the body size of the athlete, the sport, and the physiologic demands of the exercise used to train for that sport. Sports can be roughly classified according to the type and intensity of the exercise performed and the degree of static and dynamic exercise required, but such classifications are innately flawed because they do not consider exercises used in training. Dynamic (isotonic) exercise and sports primarily involve changes in muscle length and joint movement with rhythmic contractions and small intramuscular force. Static (isometric) exercise and sports mainly involve large intramuscular force with little or no change in muscle length or joint movement. Most sports require elements of both.
The acute cardiovascular response to dynamic (aerobic) exercise includes a decrease in peripheral vascular resistance and increases in heart rate, stroke volume, cardiac output, systolic blood pressure, the arteriovenous oxygen difference, and oxygen consumption. Endurance exercise training increases maximal exercise capacity as measured by maximal oxygen uptake. This increase in exercise capacity is produced by increases in the arteriovenous oxygen difference and cardiac output due to increased stroke volume.
Endurance (aerobic) sports, such as long-distance running, and their required training produce the greatest reductions in heart rate and the largest increases in maximum oxygen consumption, cardiac output, stroke volume, and cardiac chamber dimensions. Endurance exercise predominantly produces a volume load on the left and right ventricles. Static or strength sports, such as weight lifting, in contrast, produce only small increases in oxygen consumption and minimal changes in cavity size, but may be associated with mild to modest increases in wall thickness, some of which may be due to increased body mass in such athletes. These changes in wall thickness with little change in chamber dimensions mimic the changes produced by pressure load.
B. Chamber Morphologic Adaptations to Endurance Training
The morphologic adaptations to endurance training have been characterized by echocardiography and magnetic resonance imaging. Cardiac remodeling occurs in approximately one-half of trained athletes. It consists of increases in left and right ventricular and left atrial cavity dimensions and volumes almost always associated with normal systolic and diastolic function (Figure 36–1). Few studies have examined right atrial size, but this may also be increased.
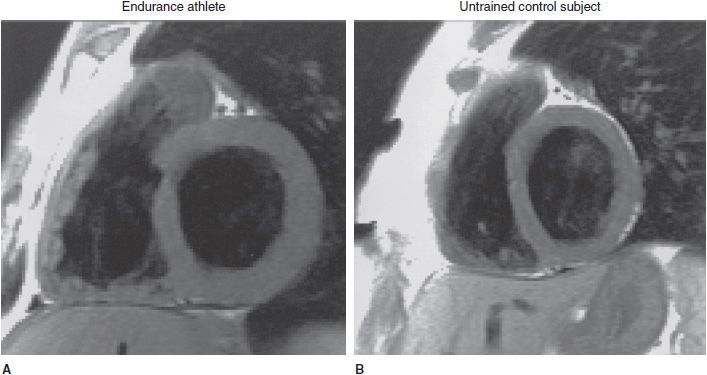
![]() Figure 36–1. End-diastolic, T1-weighted, short axis slice from an endurance athlete (A) and an untrained control subject (B). Compared with the heart of the control subject, the endurance athlete’s heart is characterized by an enlarged volume and a greater myocardial mass of both ventricles, while the proportions of the left and right heart are the same as in the untrained control subject. (Reproduced with permission from Jürgen Scharhag et al. J Am Coll Cardiol 2002;40:1856).
Figure 36–1. End-diastolic, T1-weighted, short axis slice from an endurance athlete (A) and an untrained control subject (B). Compared with the heart of the control subject, the endurance athlete’s heart is characterized by an enlarged volume and a greater myocardial mass of both ventricles, while the proportions of the left and right heart are the same as in the untrained control subject. (Reproduced with permission from Jürgen Scharhag et al. J Am Coll Cardiol 2002;40:1856).
There can be overlap between the athlete’s heart and mild forms of cardiac disease such as hypertrophic cardiomyopathy (Figure 36–2). The morphologic features of the athlete’s heart are reversible with cessation of training so that cessation of exercise can help distinguish these two conditions. Many athletes resist the idea of detraining, however, so other approaches are often required.
![]() Figure 36–2. Clinical criteria used to distinguish nonobstructive hypertrophic cardiomyopathy (HCM) from athlete’s heart when maximal left ventricular (LV) wall thickness is within shaded gray area of overlap, consistent with both diagnoses. ECG, electrocardiogram; LA, left atrium; LVH, left ventricular hypertrophy. (Adapted with permission from Maron BJ, et al. Circulation. 2006;114:1633.)
Figure 36–2. Clinical criteria used to distinguish nonobstructive hypertrophic cardiomyopathy (HCM) from athlete’s heart when maximal left ventricular (LV) wall thickness is within shaded gray area of overlap, consistent with both diagnoses. ECG, electrocardiogram; LA, left atrium; LVH, left ventricular hypertrophy. (Adapted with permission from Maron BJ, et al. Circulation. 2006;114:1633.)
C. Sudden Cardiac Death in Athletes
Clinicians require knowledge of the athlete’s heart primarily because vigorous exertion increases the risk of sudden cardiac death during exercise in individuals with known or occult heart disease. Consequently, clinicians need to know what cardiac findings in athletes are normal and how to advise individuals with diagnosed cardiac disease concerning exercise.
The frequency of sudden cardiac death (SCD) in young athletes is not clearly defined, although the largest registry of such events estimates a rate in the United States of only 66 deaths per year. Other estimates have ranged from 1 in 23,000 to 1 in 300, 000 deaths in athletes per year. This variance is likely attributable to collection bias, incomplete identification of cases, and an imprecise denominator. A study of SCD in a defined population of American collegiate athletes suggested an incidence of SCD as high as 1 in 43,000 athletes.
The most common cause of SCD in athletes younger than 35 years of age in the United States is hypertrophic cardiomyopathy (HCM), accounting for up to one-third of sport-related deaths. Other frequent causes include congenital coronary artery anomalies, myocarditis, and aortic rupture, and less commonly, arrhythmogenic right ventricular cardiomyopathy, coronary artery disease, and conduction system abnormalities. In contrast, the most common cause of exertion-related SCD in the Veneto region of Italy is arrhythmogenic right ventricular cardiomyopathy, either because mandatory Italian screening has detected and eliminated athletes with HCM or because of population differences in the prevalence of disease. In contrast to young athletes, SCD in athletes over the age of 35 years is most frequently due to occult coronary artery disease (CAD), and multiple studies have documented an increase in acute myocardial infarction (MI) and SCD among older adults during vigorous exertion.
 Clinical Findings
Clinical Findings
A. Medical History & Physical Examination
As with all of medicine, the most important element of evaluating athletes and their clinical findings is the medical history, and in the medical history, the most important element is what prompted the athlete to obtain medical evaluation. Abnormalities found on screening examinations in an asymptomatic athlete have far less import than abnormalities found during the evaluation of a symptomatic individual. In our clinical experience, most clinical abnormalities found during screening ultimately turn out to be normal variants of the athlete’s heart syndrome. Consequently, dividing athletes into those with and without symptoms is an important initial approach to their evaluation.
The other key elements of the history are the athlete’s exercise training history and his or her exercise performance. Marked changes in cardiac dimensions require considerable amounts of exercise training so that cardiac findings in an athlete with a short or low-level training history are of more concern than similar findings in an athlete with high volumes of training. It is also extremely useful to be able to assess the athlete’s level of performance. Excellent endurance exercise performance requires a large cardiac stoke volume, so that excellent exercise capacity is reassuring but does not absolutely exclude important disease. Family history of cardiac disease or unexpected or unexplained sudden death (including drowning, unexplained car accidents, or sudden infant death syndrome) is also useful in evaluating young athletes since most conditions causing SCD during exercise in this group are congenital or inherited.
The evaluation of both symptomatic and asymptomatic athletes should include a thorough physical examination. Vital signs are usually notable for training bradycardia with a resting heart rate as low as 30 bpm in highly trained aerobic athletes. Asymptomatic adolescent athletes with heart rates in this range can participate without further evaluation. Athletes may also have an S3 and S4 gallop. Athletes frequently have classical flow murmurs related to their slower heart rates and concomitant increased stroke volume. These functional murmurs typically are systolic and less than IV/VI in intensity. They are typically present supine because of enhanced venous return in this position and absent with the athlete upright; they have no diastolic component and are associated with a normal physiologic split of the second heart sound. Because HCM is the most frequent cause of SCD in young athletes, auscultation during the Valsalva maneuver or after arising from the squatting position, either of which should decrease cardiac dimensions and increase the murmur of HCM, is useful.
Syncope is a common problem among athletes and a frequent reason for referral to a cardiologist. Syncopal events are significant if judged to be not neurocardiogenic (vasovagal) and if they occur during exercise. Postexertional syncope is a common phenomenon in athletes. It is usually benign and does not require further workup. Under normal circumstances, exercise increases cardiac output and decreases peripheral vascular resistance due to vasodilation. Syncope after exercise can occur because the increases in cardiac output and heart rate decrease more rapidly than does the peripheral vasodilation. The net effect when the individual stops exercising is an increase in vasodilation without the compensatory increase in heart rate and cardiac output, thus explaining postexertional syncope. In contrast, syncope during exercise usually suggests a cardiac origin, such as anomalous coronary artery anatomy or cardiac arrhythmias.
The American Heart Association (AHA) position on screening athletes before competition recommends a 12-point evaluation (Table 36–1). The historical elements are important, but young athletes often respond positively to many of these queries, again highlighting the importance of separating the evaluation of athletes with abnormalities found on screening from those presenting with symptoms.
Table 36–1. The 12-Element American Heart Association Recommendations for Preparticipation Cardiovascular Screening of Competitive Athletes
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


