The Aorta
ECHO APPEARANCES OF THE NORMAL AORTA
The aorta extends all the way from the aortic valve to the point where it bifurcates into the left and right common iliac arteries. Different parts of the aorta are visible in many of the standard transthoracic echo (TTE) views (see Chapter 6):
left parasternal window
parasternal long axis view
parasternal short axis view
right parasternal window
apical window
apical 5-chamber view
apical 3-chamber (long axis) view
subcostal window
suprasternal window
aorta view.
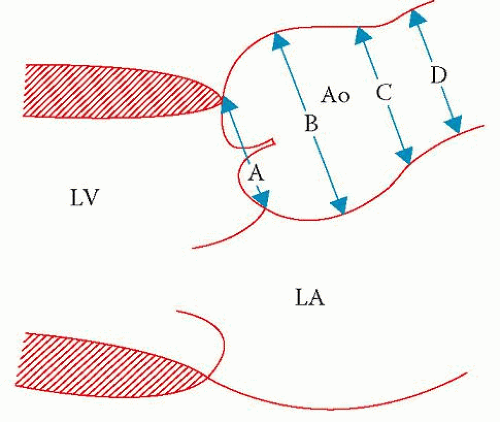
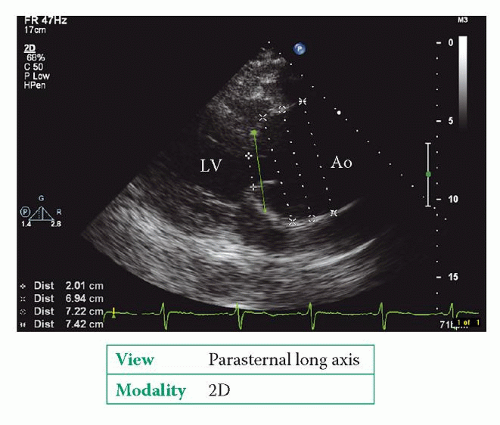
The parasternal long axis view is the preferred view for measuring aortic root dimensions, which are taken at four different levels (Fig. 26.1):
aortic annulus
sinuses of Valsalva
sinotubular junction
tubular ascending aorta.
Always measure aortic dimensions perpendicular to the axis of blood flow, at the widest diameter, from inner edge to inner edge. It is preferable to use 2D echo to make measurements rather than M-mode.
Normal ranges for the aortic diameter at each of these levels are:
2.0-3.1 cm at the level of the aortic annulus
2.4-4.0 cm at the level of the sinuses of Valsalva
2.2-3.6 cm at the level of the sinotubular junction
2.2-3.6 cm at the level of the tubular ascending aorta.
In addition, there are published normal ranges for aortic diameter, indexed for body surface area, in the form of nomograms (e.g. British Society of Echocardiography: Guidelines for valve quantification, p. 304; or see Roman MJ, et al. Two-dimensional echocardiographic aortic root dimensions in normal adults, American Journal of Cardiology 1989; 64: 507-12).
In addition, you can assess the:
aortic arch in the suprasternal window
descending thoracic aorta (located behind the left atrium) in the parasternal long axis view
proximal abdominal aorta in the subcostal view.
Commonly quoted indexed normal ranges at these levels include:
<1.9 cm/m2 at the level of the aortic arch
<1.6 cm/m2 at the level of the descending thoracic aorta
<1.6 cm/m2 at the level of the abdominal aorta (at or above the superior mesenteric artery).
For a full echo assessment of the aorta, inspect each part of the aorta and:
describe its appearance (normal or abnormal)
comment on any dilatation (stating location and dimensions)
identify any atheroma or thrombus (stating location, appearance, severity and if it is mobile)
identify any dissection (stating the entry and exit point and whether there is any thrombus in the false lumen)
identify any intramural haematoma (stating the location)
identify any transection (stating the location)
identify and characterize any aortic coarctation (see p. 287).
AORTIC DILATATION
Dilatation of the aorta can result from:
atherosclerosis
hypertension
trauma
post-stenotic (dilatation of the ascending aorta above a stenotic aortic valve).
Aortic dilatation (and dissection) is also more likely in patients with bicuspid aortic valve (p. 286) and correlates with the degree of aortic regurgitation that may be present. Patients with bicuspid aortic valve are 10 times more likely to experience an aortic dissection than those with a normal valve.
A number of connective tissue and inflammatory diseases can cause aortic dilatation:
Marfan syndrome
systemic lupus erythematosus
rheumatoid arthritis
Reiter syndrome
syphilitic aortitis.
In aortic dilatation due to Marfan syndrome, the relative proportions of the aortic root (broader at the sinuses of Valsalva, becoming narrower again at the sinotubular junction) are lost and the boundary between the sinuses of Valsalva and the ascending aorta becomes less clear – this is referred to as effacement of the sinotubular junction. Marfan syndrome is discussed on page 296. Localized dilatation of one or more sinuses of Valsalva is called sinus of Valsalva aneurysm (p. 265).
Echo assessment of aortic dilatation
Aortic dilatation can occur in more than one site, so for an aortic assessment it is important to measure the aortic dimensions in as many sites as possible (Fig. 26.2):
aortic annulus
sinuses of Valsalva
sinotubular junction
ascending aorta
aortic arch
descending thoracic aorta
proximal abdominal aorta.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree