Chapter 87
Technique
Open Surgical
Anton N. Sidawy, Richard F. Neville
Based on a chapter in the seventh edition by Jamal J. Hoballah
The management of vascular disease has undergone a major evolution. A decade ago, whenever vascular intervention was deemed necessary, open vascular surgery was the norm. However, with advances in catheter-based technology, endovascular therapy is now the first option in most clinical situations. Endovascular intervention is less invasive, and patient recovery is rapid. The limitations of endovascular therapy are related to specific anatomic considerations and questions of durability.
Open vascular surgery traditionally offered the “gold standard” with respect to durability and efficacy. However, it was associated with the typical morbidity and mortality of all open surgical procedures. These drawbacks included complications of general anesthesia (when used), the physiologic changes of clamping and unclamping major vessels, the significant intraoperative blood loss and fluid shifts in vascular procedures, and the impact of various types of skin, abdominal, and thoracic incisions.
With the goal of decreasing the morbidity of vascular interventions, the shift toward endovascular procedures is well justified. When an endovascular intervention is anatomically challenging, hybrid procedures that combine open vascular surgery and endovascular techniques can be used to modify the anatomy so that endovascular intervention is possible. For example, a bypass to the common iliac artery or aorta may be constructed to allow the safe passage of a large stent-graft for endovascular thoracic aortic aneurysm repair in a patient with a small or occluded iliac artery. Similarly, debranching procedures, such as iliorenal and iliomesenteric bypasses, in patients with suprarenal aortic aneurysms or carotid-subclavian and carotid-carotid bypasses in patients with thoracic aortic aneurysms can provide a landing zone during the endovascular treatment of a thoracoabdominal or thoracic aortic aneurysm.
Despite advances in endovascular technology and the increase in the number of endovascular interventions, open vascular reconstructions will continue to play a significant role in the management of patients with vascular disease for the foreseeable future.
Basic Principles
The key elements of a successful open vascular reconstruction are choosing the right procedure and vascular exposure and then executing the selected procedure correctly. Appropriate choices for the source of inflow, the target for outflow, and the proper conduit, if needed, are critical for success of any revascularization. This success also requires the appropriate instruments, graft, and suture materials. In addition, open vascular procedures should be performed under excellent lighting aided by magnifying loupes in select cases. For the operating surgeon, maintaining good ergonomic position during the reconstruction is essential to prevent significant work-related discomfort in the neck, shoulders, or back.
Vascular Instruments and Retractors
A vascular instrument tray typically includes vascular clamps, needle holders, forceps, scissors, and various retractors. Depending on the size of the vessel and the location of the surgical reconstruction, the instruments used will vary.
Clamps
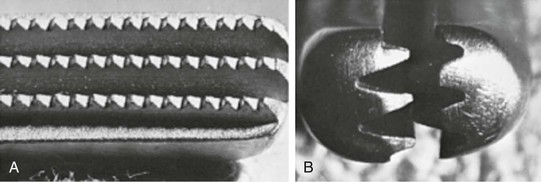
Vascular clamps typically have jaws with rows of fine interdigitating serrations that allow clamping of the vessel without slippage or significant crush injury. Although vascular clamps are considered atraumatic, a vascular clamp applied inappropriately can cause significant intimal damage or may tear the artery if placed over a plaque in an inappropriate manner. Even in a soft, minimally diseased artery, a clamp applied with excessive force can damage the arterial wall and intima.
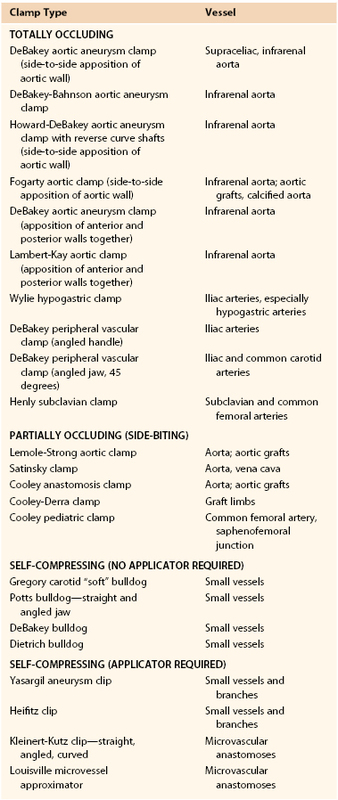
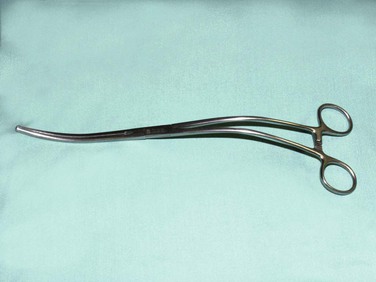
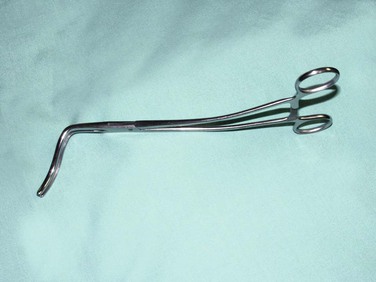
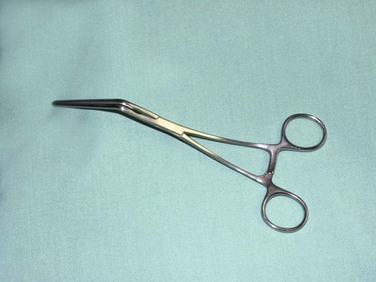
In general, clamps can be divided into those used for large, medium, or small vessels. They vary in shape and angulation to fit into specific anatomic locations, and they can be used as fully or partially occluding clamps. Clamps with special soft plastic inserts (e.g., Fogarty soft jaw) are also available to allow the clamping of prosthetic grafts without damaging the graft material. Types of vascular clamps and their suggested uses are outlined in Table 87-1. For smaller vessels and branches, various sizes of bulldog clamps or intracranial aneurysm clips, such as the Yasargil or Heifitz clips, are available (see e-Figures 87-1 to 87-12![]() ).
).
Needle Holders, Forceps, and Scissors
Needle holders of various lengths and shapes are available. The choice of needle holder is often dictated by the size of the needle used. A Mayo-Hegar needle holder is typically used with large needles, and Castroviejo needle holders are typically used with small, fine vascular needles (see e-Figure 87-13![]() ).
).
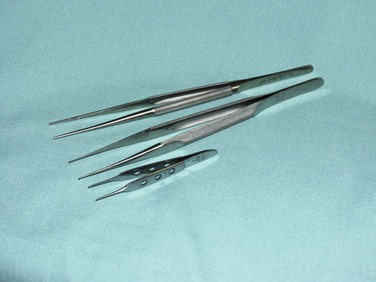
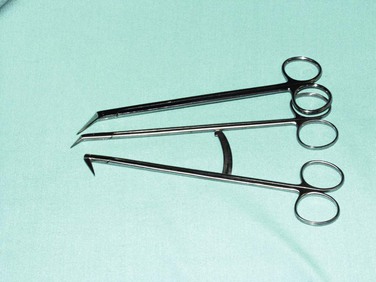
The forceps used during vascular procedures typically have very fine, noncrushing jaws, exemplified by the DeBakey forceps. However, similar to vascular clamps, vascular forceps can crush a vessel wall if they are not used appropriately and delicately. Fine-tip ring forceps or Jarrell forceps are very useful during the construction of vein bypasses to infrapopliteal vessels. Metzenbaum and Church scissors are used for the dissection of blood vessels. Stevens tenotomy scissors with sharp tips are used for dissecting tibial vessels. Special Potts scissors with various angulations are used to enlarge and shape arteriotomies and venotomies. Right-angle clamps with various tip sizes are used to encircle blood vessels and branches (see e-Figures 87-14 to 87-19![]() ).
).
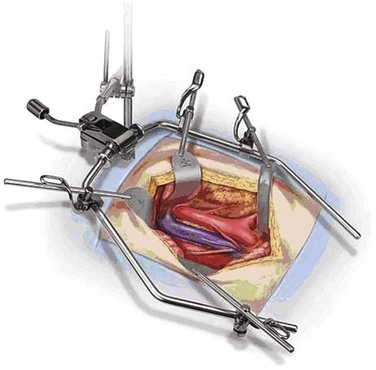
Retractor Systems
Retractors can be self-retaining or handheld. Self-retaining retractors should be used whenever possible. The Omni-Flex vascular retractor (Omni-Tract Surgical, St. Paul, Minn) is frequently used for open aortic surgery, whether transabdominal or retroperitoneal (see e-Figure 87-20![]() ). This retractor system consists of a wishbone that attaches to a post mounted on the operating room table rail, and it typically offers a selection of blades with different depths, widths, and shapes that can be clamped to the wishbone. Shallow, wide blades are typically used to retract the abdominal walls, whereas deeper splanchnic blades may be used to retract the splenic flexure and other parts of the colon. A wide, fence-shaped blade is typically used to retract the small bowel during aortic dissection, and a narrow, deep blade may be used to retract the left renal vein cephalad. This retractor system is useful during thoracoabdominal aortic aneurysm repair. Modifications of this retractor have also been designed for inguinal, carotid, and spine exposures.
). This retractor system consists of a wishbone that attaches to a post mounted on the operating room table rail, and it typically offers a selection of blades with different depths, widths, and shapes that can be clamped to the wishbone. Shallow, wide blades are typically used to retract the abdominal walls, whereas deeper splanchnic blades may be used to retract the splenic flexure and other parts of the colon. A wide, fence-shaped blade is typically used to retract the small bowel during aortic dissection, and a narrow, deep blade may be used to retract the left renal vein cephalad. This retractor system is useful during thoracoabdominal aortic aneurysm repair. Modifications of this retractor have also been designed for inguinal, carotid, and spine exposures.
Another self-retaining abdominal retractor is the Bookwalter retractor (Codman Johnson & Johnson, Raynham, Massachusetts (see e-Figure 87-21![]() ). This retractor is often used when conducting abdominal aortic replacement through mini-laparotomy incisions. The retracting blades in the Bookwalter retractor attach to an oval metal ring placed around the abdominal incision instead of a wishbone.
). This retractor is often used when conducting abdominal aortic replacement through mini-laparotomy incisions. The retracting blades in the Bookwalter retractor attach to an oval metal ring placed around the abdominal incision instead of a wishbone.
Several single-instrument self-retaining retractors are available for neck and extremity procedures (see e-Figures 87-22 to 87-24![]() ). The Weitlaner retractor is commonly used for inguinal and popliteal incisions. The Adson cerebellar retractor is angled such that it can also be very useful in groin and below knee exposure. In obese patients with significant inguinal pannus, a Miskimon retractor can be especially useful because of its deeper and wider blades, which provide a larger retracting area. Spring retractors are extremely useful when conducting infrageniculate vessel exposure because they tend to occupy little space. The Gelpi retractor is typically helpful when conducting a first rib resection through a transaxillary approach for thoracic outlet obstruction.
). The Weitlaner retractor is commonly used for inguinal and popliteal incisions. The Adson cerebellar retractor is angled such that it can also be very useful in groin and below knee exposure. In obese patients with significant inguinal pannus, a Miskimon retractor can be especially useful because of its deeper and wider blades, which provide a larger retracting area. Spring retractors are extremely useful when conducting infrageniculate vessel exposure because they tend to occupy little space. The Gelpi retractor is typically helpful when conducting a first rib resection through a transaxillary approach for thoracic outlet obstruction.
Vascular Sutures and Grafts
Sutures
Nonabsorbable sutures are used for vascular anastomoses and repairs. These sutures typically provide the tensile strength necessary to juxtapose and secure the vessels together until healing is completed. When prosthetic conduits are used in vascular reconstruction, the tensile strength provided by the sutures is needed indefinitely to maintain vascular integrity. Currently, monofilament sutures are most commonly used for vascular reconstructions, although some surgeons still prefer braided polyester multifilament sutures. Vascular sutures are usually double-armed with a needle on each end to allow continuous suturing in both directions from the initial knot.
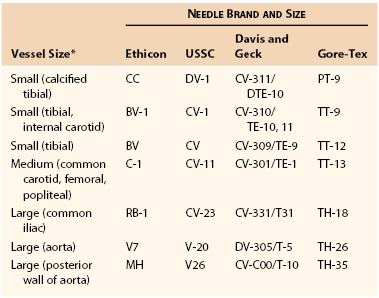
Commonly used monofilament sutures include polypropylene, polybutester, and polytetrafluoroethylene (PTFE). Polypropylene sutures (Prolene, Ethicon Inc., Somerville, NJ; Surgipro and Surgilene, Covidien, Mansfield, Mass) are made of a monofilament strand of synthetic linear polyolefin. These sutures tend to maintain their tensile strength over time. They have little friction and excellent handling characteristics. They are widely popular and are probably the most commonly used suture material in vascular reconstructions. Polybutester is another type of monofilament suture made of a copolymer of polyglycol terephthalate and polytrimethylene terephthalate coated with polytribolate to reduce drag and improve tissue passage. PTFE sutures were developed to minimize the needle hole bleeding that is often seen when polypropylene sutures are used with PTFE grafts or patches. They are designed so that there is minimal difference in the diameters of the needle and the suture. They have excellent handling characteristics, with a low tissue friction and low drag coefficient. The needle and suture sizes vary, depending on the vessel. Suggestions are provided in Table 87-2.
Grafts
Selection of a graft type is an integral part of any vascular reconstruction. Polyester grafts of different shapes and structures are available to replace the thoracic aorta. Polyester and PTFE grafts are available as conduits for the abdominal aorta and infrainguinal vessels. Autogenous vein grafts are favored in many small arterial reconstructions. These grafts are discussed in detail in Chapter 92, 93, and Chapter 94.
Basic Vascular Techniques
Open vascular surgery is conducted using the general principles of blood vessel exposure with proximal and distal control, along with the basic techniques of vascular reconstruction. These basic vascular techniques include thromboembolectomy, endarterectomy, creation and closure of an arteriotomy, and construction of bypasses or in-line graft replacement using end-to-side or end-to-end anastomoses.
Vascular Exposure and Dissection
An exhaustive discussion of specific vascular exposures is beyond the scope of this chapter; these are addressed in greater detail in procedure-specific chapters. Several excellent resources are also available that describe the vascular anatomy and the variety of exposures available to the vascular surgeon.1–4
Initial Vessel Exposure
The basic concept of vascular exposure and dissection is to approach and expose the vessels by the most direct and shortest route possible. Selection of the surgical approach and incision should take into consideration the possibility that the operation may become more complex than originally anticipated and that surgical control and reconstruction may occur at a more proximal or distal location. Anatomic landmarks, location of the pulse, or a combination of the two is typically used to guide placement of the initial skin incision. In most cases, the vascular structures can be exposed by dissection between existing muscle bellies. If dissection requires extensive muscle transection, the approach to the vascular structures should be reconsidered.
Following incision, proper handling of the skin and soft tissue overlying the vessels is essential to prevent significant wound complications. Lymphatics are typically ligated and divided to avoid lymphorrhea and lymphocoele. Use of electrocautery through lymph nodes should be avoided to prevent significant lymph leak or the need to excise lymph nodes, leaving dead space in the wound.
Once the vascular sheath is identified and incised, the adventitia is held and retracted in one direction, and dissection is carried out in the tissue adjacent to the edge of the blood vessel wall. By staying close to the adventitia, the dissection can be maintained in the correct areolar anatomic plane, and the vessel can be circumferentially dissected and encircled with a Silastic loop or umbilical tape (Dow Corning Corporation, Midland, Mich). The basic surgical technique of traction with countertraction is essential in vascular exposure. Traction on a vessel loop is often used to retract a vessel during dissection or mobilization. Gentle tension on the vessel loop is recommended to prevent injury to the intima.
“Redo” Vessel Exposure
“Redo” vascular exposure poses a unique challenge, given the fibrous obliteration of the normal anatomic vascular planes. When the surgeon is faced with a “redo” operation, sharp dissection with a No. 15 knife blade may allow better management of the scar tissue than scissor dissection, and it may allow the surgeon to stay in the appropriate dissection plane. An inadvertent arteriotomy caused by a small blade may be easier to repair than arterial disruption caused by dissecting scissors. The most common vessel that requires “redo” exposure is the common femoral artery, and the approach to this vessel is illustrative of “redo” vessel exposure in general.
The principle of dissecting from known to unknown can be useful in preventing branch vessel injury during re-exposure and to obtain proximal control outside of the scarred area to aid in vascular control should an inadvertent injury occur. A significant concern with a “redo” femoral artery exposure is injuring the profunda femoris artery. Consequently, the superficial femoral artery is exposed in the most distal part of the incision, where minimal scarring exists. The dissection is then carried along the medial aspect of the superficial femoral artery and progresses proximally. Typically, the common femoral vein is identified during the process, revealing a safe dissection plane. Once the inguinal ligament is reached, the common femoral artery is encircled with a loop. The direction of the dissection is then reversed and continued back distally toward the superficial femoral artery. The area of size transition between the common and superficial femoral arteries exposes the location of the profunda femoris artery. At that level, dissection from the medial and posterior aspect of the common femoral artery identifies a plane that has not been violated and allows dissection of the profunda femoris artery from underneath the common femoral artery. The profunda femoris artery is controlled at its origin by passing a vessel loop underneath the superficial femoral artery and then retrieving it just proximal to the common femoral bifurcation. In cases of extensive scarring, the profunda femoral branch can be controlled with a balloon occlusion catheter after common femoral arteriotomy, to avoid potential injury during profunda dissection.
Anticoagulation
Before interrupting blood flow, the patient must be adequately anticoagulated. Unfractionated heparin at 75 to 100 U/kg is typically administered intravenously approximately 5 minutes before blood flow interruption. We recommend that the anticoagulation be monitored by measuring the activated clotting time (ACT), aiming for a value of more than 250 seconds.
Distal limb ischemia following aortic reconstruction or other types of vascular procedures is a dreaded complication and is often attributed to distal embolization. However, an important factor in this complication is unrecognized suboptimal anticoagulation. Hence, it is important to maintain adequate anticoagulation throughout the period of blood flow interruption by re-dosing with heparin when necessary, using the ACT for guidance. In patients with known heparin-induced thrombocytopenia, anticoagulation may be achieved with intravenous thrombin inhibitors such as argatroban (see Chapter 35).
Blood Vessel Control
Blood vessel control can be achieved using vascular clamping, balloon occlusion, vessel loops, pneumatic tourniquet, Rumel tourniquet, or internal occluders.
Vascular Clamping
Ideally, vascular clamps should be applied to a disease-free segment of the artery. Palpating the artery against a right-angle clamp can help determine the presence and extent of atherosclerotic plaque, which is often in a posterior location and not appreciated by only palpating the anterior aspect of the artery. In the presence of significant plaque, the artery should be dissected more proximally to identify a less diseased site for clamping. This situation is often encountered when clamping the common femoral artery, where plaque often extends to the level of the inguinal ligament. Further dissection proximal to the external iliac circumflex and inferior epigastric branches, however, usually reveals an external iliac artery that is soft and free of disease. If clamping is necessary across an area of diseased artery, the clamp should be applied in a manner that opposes the soft part of the artery against the plaque without causing plaque fracture or vessel tear.
Occasionally, the plaque burden and calcification are so extensive that the only option is to identify a more proximal location for safe clamp placement. One example is supraceliac aortic control through the lesser sac, when clamping in the infrarenal or suprarenal location is not possible because of extensive calcification or scarring from previous surgery or an inflammatory process.
Balloon Occlusion
If the plaque is circumferential or occupies more than 50% of the circumference, vascular clamps can fracture the plaque or tear the wall, and may not provide vascular control. This can be managed by occluding the artery from within using a compliant balloon occlusion catheter, such as the Fogarty catheter normally used to perform embolectomy, or a noncompliant balloon catheter used for angioplasty. There are also several compliant occlusion balloons that can be used to occlude the aorta during ruptured aneurysm repair, including Reliant (Medtronic, Minneapolis, Minn), Coda (Cook, Bloomington, Ind), and Equalizer (Boston Scientific, Natick, Mass). Balloon occlusion can be used to control the external iliac artery in the presence of extensive calcification that extends beyond the most proximal part of the exposure. It is also useful for controlling the right common iliac artery during a left retroperitoneal abdominal aortic aneurysm repair, the profunda femoris artery during repair of a pseudoaneurysm of a femoral anastomosis, or the renal or visceral vessels during a thoracoabdominal aortic aneurysm repair.
Vessel Loops
Vessel loops are ideal for controlling small- to medium-sized vessels, such as the profunda femoris or popliteal arteries and arterial branches. Silastic vessel loops can be traumatic, however, if excessive tension is applied to them. A double loop, or Potts technique, can be helpful in the use of vessel loops by minimizing the tension required to obtain vascular control of small- or medium-sized arteries. Further, excessive tension on Silastic vessel loops for simultaneous proximal and distal control of a vessel may make an anastomosis or repair more difficult to construct. One way to avoid excessive tension on the artery in two opposing directions is to apply a vessel loop on the proximal side of the artery and a small Yasargil aneurysm clamp or bulldog clamp on the distal end of the artery (Fig. 87-25).
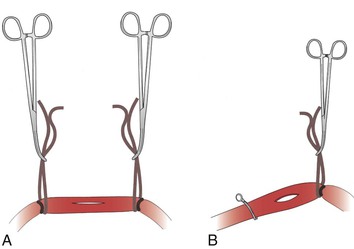
Figure 87-25 A vessel loop on the proximal side of the artery and a small Yasargil aneurysm clamp or bulldog clamp on the distal side of the artery can minimize tension on the anastomosis. A, Pulling on both loops can result in tension on the arteriotomy. B, Tension on the anastomosis is minimized when one loop is pulled and the other replaced with a bulldog clamp.
Pneumatic Tourniquet
A pneumatic tourniquet can be used for vascular control in the extremities and is ideal for infrapopliteal reconstructions. It allows for minimal exposure, dissection, and handling of the arteries, and may decrease the risk of spasm or injury caused by clamping of the tibial vessels. The tourniquet can be placed around the thigh or below the knee; usually a soft roll is applied first, followed by the tourniquet. The leg is elevated, and an Esmarch compression wrap is used to wrap the leg from the foot in a cephalad direction expelling the venous blood from the leg. The tourniquet is then inflated to a pressure of about 250 or 100 mm Hg above systolic pressure. It is essential to make sure the graft is well aligned and to mark the graft orientation before inflating the tourniquet. Bleeding occasionally occurs despite the tourniquet, and this can sometimes be controlled by increasing the pressure in the tourniquet. An additional clamp on the profunda femoris artery can also help control persistent bleeding. Sometimes calcified and incompressible arteries at the tourniquet site prevent this technique from completely controlling bleeding at the distal arteriotomy.
Other Techniques
Rumel tourniquets can be used for vascular control, but they can cause arterial wall damage in the presence of significant plaque. The Rumel tourniquet may be most useful during an endovascular aortic aneurysm procedure when there is a large sheath in an artery and persistent bleeding from the arteriotomy around the sheath. Cinching the sheath with a Rumel tourniquet at that level can control the bleeding. Pediatric Rumel tourniquets are useful to atraumatically secure carotid intraluminal shunts to control blood leak around the shunt keeping blood flow to the brain while carotid endarterectomy is being performed.
When dealing with tibial vessels, direct clamping of the arteries should be avoided to prevent intimal injury or spasm. The use of internal coronary artery occluders in this setting can be useful to achieve vessel control. Florester internal vessel plastic tip occluders (Biovascular, St. Paul, Minn) are available in various sizes. However, the surgeon must be comfortable using such occluders, and oversizing should be avoided to prevent intimal damage during insertion.
Thrombectomy and Thromboembolectomy
Basic Considerations
Thrombectomy and thromboembolectomy must be mastered by every vascular surgeon because the need to perform these procedures is inevitable. Even the most successfully performed open or endovascular procedure can be complicated by a distal embolic or a thrombotic event. Although numerous techniques are available to achieve pharmacologic or mechanical thrombectomy, the need for balloon thrombectomy cannot be completely avoided. Balloon thrombectomy allows the removal, inspection, and pathologic examination of the occlusive clot and restores blood flow expeditiously.
A vessel may become acutely occluded because of a thrombotic or embolic process. Thrombosis frequently occurs proximally and distally to the embolus because of the stagnant flow; hence, the term thromboembolectomy. Balloon embolectomy is often paired with thrombectomy to remove the thrombus. Several issues need to be addressed during the performance of a thromboembolectomy procedure, including the location and shape of the arteriotomy used to extract the thrombus, selection of the thrombectomy catheter, and performance of the procedure with minimal blood loss and injury to the arterial system. In addition, steering the catheter into the appropriate location and extracting all the offending thrombi are essential to the success of the procedure.
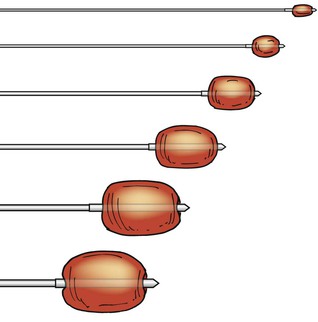
Thromboembolectomy Catheters
A wide variety of thromboembolectomy catheters are available (see e-Figures 87-26 and 87-27![]() ). The standard ones are balloon catheters that vary in size, length, and maximal balloon inflation. These catheters are typically available in sizes from 2 to 7F. Saline solution is used to inflate the balloon, except for the 2F balloon, which requires air insufflation for easy deflation. The diameter of the fully inflated balloon is 4 mm for the 2F catheter, 5 mm for the 3F, 9 mm for the 4F, 11 mm for the 5F, 13 mm for the 6F, and 14 mm for the 7F.
). The standard ones are balloon catheters that vary in size, length, and maximal balloon inflation. These catheters are typically available in sizes from 2 to 7F. Saline solution is used to inflate the balloon, except for the 2F balloon, which requires air insufflation for easy deflation. The diameter of the fully inflated balloon is 4 mm for the 2F catheter, 5 mm for the 3F, 9 mm for the 4F, 11 mm for the 5F, 13 mm for the 6F, and 14 mm for the 7F.
Size 2F catheters are typically used for very small pedal or hand vessels. The most commonly used catheters are 3 to 5F catheters. A 3F Fogarty catheter is typically used for tibial vessels. A 4F Fogarty catheter is used for vessels the size of the superficial femoral and popliteal arteries; it can also be used for external iliac arteries. A 5F Fogarty catheter is typically used for external iliac or common iliac arteries. Size 6F and size 7F catheters can be used for thrombectomy of an aortic femoral graft or a saddle aortic embolus. A venous thrombectomy catheter with a large, lower pressure balloon is also available.
Standard balloons are made of latex; however, latex-free embolectomy catheters are available for patients with latex allergy. In addition, balloon catheters that can be introduced over guide wires for fluoroscopically assisted thromboembolectomy are also available in sizes 3, 4, 5.5, 6, and 7F.
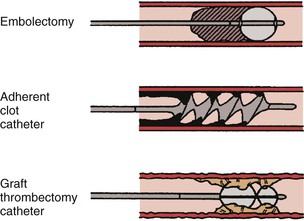
Special catheters have been devised for adherent clots. The Fogarty adherent clot catheter (Edwards Life Sciences, Irvine, Calif) features a spiral-shaped, latex-covered stainless steel cable that assumes a corkscrew shape when retracted, thus expanding the surface area to entrap fibrous material. It is marketed for adherent clots resistant to removal by standard elastomeric balloons in both native arteries and synthetic grafts. The Fogarty graft thrombectomy catheter (Edwards Life Sciences) is designed to remove tough thrombus from synthetic grafts; it has a flexible wire coil at the distal end and expands when retracted to form a double-helix ring that acts as stripper, forming a plane between the graft and the adherent material. This catheter is not intended for native vessels and is marketed for use in PTFE dialysis grafts and aortobifemoral grafts (see e-Figure 87-28![]() ).
).
Technique
Arteriotomy Location and Shape
The balloon embolectomy catheter is designed to extract thrombi from a site remote from the clot’s location. The arteriotomy for clot extraction can be performed in a location proximal or distal to the embolic or thrombotic process. Site selection depends on the ease of exposure, anticipated location of the thrombus, and ease of arteriotomy closure. In patients with acute lower extremity ischemia, the common femoral artery is an ideal site for clot extraction. A patient with an aortic saddle embolus or a popliteal embolus can be managed by thromboembolectomy through the common femoral artery. The common femoral artery and its bifurcation are easy to expose, and closure of the arteriotomy is easily accomplished in this relatively large artery. Further, the procedure can be performed under local anesthesia. If thromboembolectomy proves to be inadequate, a site closer to the location of the thrombus may be required. Before performing the thrombectomy, it is important to ensure that the patient is adequately anticoagulated.
The selection of a transverse versus longitudinal arteriotomy for catheter access is influenced by the size of the vessel, the cause of the embolus or thrombus, and the presence of plaque in the vessel. A transverse arteriotomy is usually simpler to close and may be preferred when dealing with an embolic process. When the occlusive pathology is due to an atherosclerotic and thrombotic process, or when significant arterial plaque is present, a longitudinal arteriotomy should be used. In such a situation, it is not uncommon for an emergency bypass to become necessary, and the longitudinal arteriotomy can be incorporated into one of the anastomoses. If a bypass is deemed unnecessary, a patch is usually needed to close the longitudinal arteriotomy to avoid significant narrowing of the vessel lumen. Transverse arteriotomy can be easily closed with interrupted sutures to avoid purse-stringing and narrowing of the lumen of the artery at the site.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree