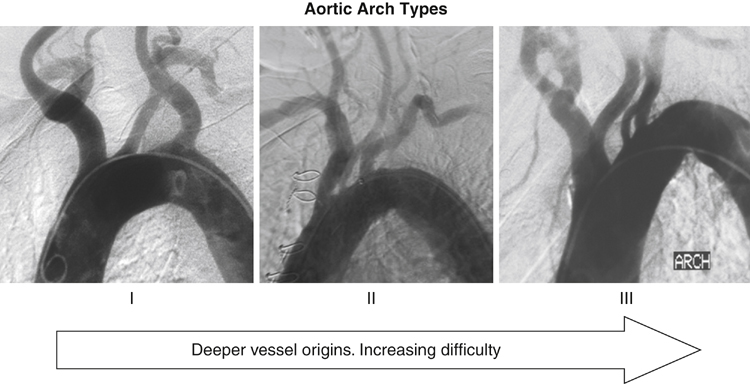
Arch manipulations with guidewires, catheters, and sheaths carry a risk of neurologic events and should be carefully performed. A 260-cm guidewire is placed in the ascending aorta, followed by a pigtail catheter. An initial arch angiogram is performed with the image intensifier in a left anterior oblique (LAO) position. The image intensifier is rotated until the upside-down U shape formed by the guidewire is as wide as possible, usually at least 30 degrees to 45 degrees, to better expose the origins of the arch vessels. The tortuosity of the arch may be assessed by drawing a horizontal line across the apex of the inner curvature of the arch. Vessels that originate below the horizontal line at the apex of the aortic arch often are more difficult to selectively cannulate (Figure 1). Alternatively, the arch may be assessed by less invasive means using CTA or MRA. Selective cannulation of the arch vessels is a critical portion of carotid angioplasty and stenting procedures. Catheterization can usually be accomplished using one of two preshaped catheters: a simple-curve catheter such as a vertebral catheter or a complex-curve catheter such as the reversed-angle Vitek catheter or Simmons catheter (Table 1). The image intensifier is maintained in its fixed position (LAO), and the bony landmarks or road mapping may be used to guide cannulation of the vessel. The catheter of first choice in most cases is a simple-curve catheter, such as a vertebral catheter. The angle formed by the vertebral catheter along with the tip angle on an angled guidewire (Glidewire) is adequate to cannulate the common carotid artery in most patients. Once the guidewire has accessed the common carotid artery, the vertebral catheter is advanced over the guidewire for selective angiograms of the common carotid artery. Be aware that as the cerebral catheter rounds the turn from the aortic arch into the common carotid artery, it tends to straighten out, and the guidewire can jump forward. TABLE 1 Equipment Used in Carotid Angioplasty and Stenting
Technical Aspects of Percutaneous Carotid Angioplasty and Stenting for Arteriosclerotic Disease
Carotid Imaging and Sheath Access
Aortic Arch Angiogram
Selective Common Carotid Catheterization
Step
First-Line Equipment
Alternative Equipment
Arterial access
Micropuncture kit
6- or 7-Fr sheath
Single-wall entry needle
Imaging
260-cm soft guidewire
70-cm or 100-cm pigtail catheter
Selective cannulation
Vertebral catheter
100-cm angled glide catheter
Vitek catheter
Simmons catheter
H1 catheter
Carotid sheath access
260-cm stiff guidewire
90-cm sheath
Guiding catheter
Cerebral protection
Free-wire filter
Fixed-wire filter
0.14 buddy wire
Flow reversal
Angioplasty
Predilatation: 3 × 40 mm monorail balloon
Postdilatation: 5.0 or 5.5 × 2 mm monorail balloon
Stenting
Tapered self-expanding stent
Straight self-expanding stent
Pharmacotherapy
Atropine
Nitroglycerin
Heparin
Bivalirudin
Filter management
Filter aspiration catheter
Filter retrieval catheter
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Technical Aspects of Percutaneous Carotid Angioplasty and Stenting for Arteriosclerotic Disease
