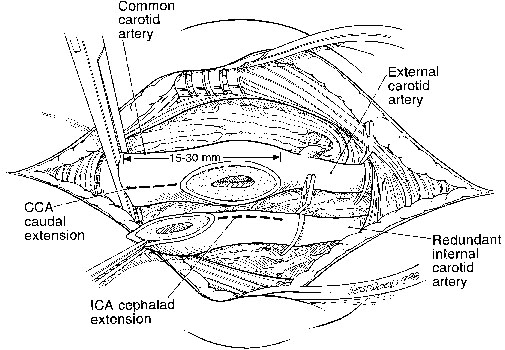
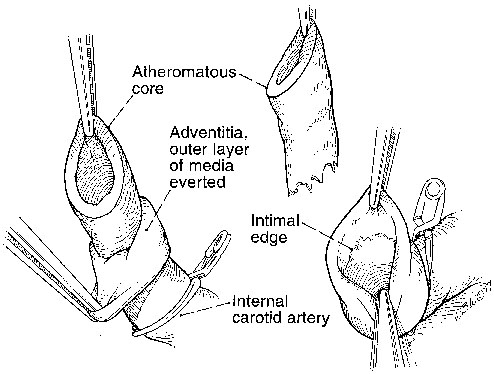
Dhiraj M. Shah, R. Clement Darling, III, Benjamin B. Chang, Paul B. Kreienberg, Philip S.K. Paty, Kathleen J. Ozsvath, Sean P. Roddy and Manish Mehta At this time, the ICA is transected obliquely, with the line of division running from the crotch of the carotid to a point more proximal on the lateral (internal) side of the CCA. The specific angle of division is not critical, but a 10- to 15-mm opening should be left in the CCA. Doing so aids visualization of disease in the bulb and facilitates reanastomosis of the arteries. After division, the ICA almost always is redundant. Because of this, it may be spatulated, further increasing the diameter of the eventual suture line. If this is done, the common carotid arteriotomy is extended caudad a similar amount (Figure 1). Endarterectomy of the ICA is begun by circumferentially elevating the plaque from the arterial wall. It is important to remove both the intima and media, and if done, the adventitia may be grasped with two fine forceps while the assistant holds the plaque. The adventitia is then pulled or rolled like a sock until the end of the plaque is reached (Figure 2). If the endarterectomy plane is too shallow and appreciable media remains, the artery will be too stiff to easily evert. At this time, the specimen usually spontaneously divides at the endpoint. If not, the plaque is sharply divided at its termination. This process usually requires less than 30 seconds.
Technical Aspects of Eversion Carotid Endarterectomy for Atherosclerotic Disease
Methods
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree