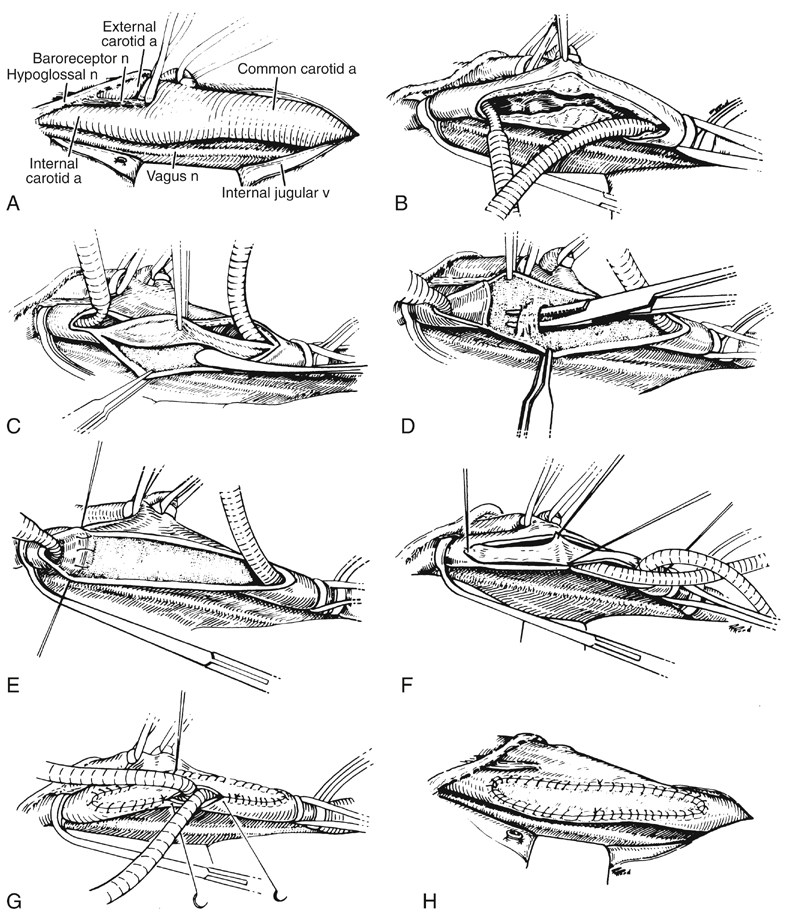
The author has previously reported a personal series of 2262 CEAs, nearly all being done under general anesthesia with routine carotid shunting and, during the last 20 years, patch angioplasty preferentially using the saphenous vein. The principal technical steps of the procedure became standardized (Figure 1). After the patient is positioned on a shoulder roll, the neck, the upper chest, and the groin from which the greater saphenous vein is to be harvested are prepared and draped in a standard fashion. The cervical incision is made parallel and slightly anterior to the course of the sternocleidomastoid muscle, its length being determined by the level of the carotid bifurcation on preoperative imaging studies. If an especially high incision is necessary, it is angled posterior to the earlobe to avoid the parotid gland. The platysma layer is divided with the cutting mode of the electrocautery unit, and complete hemostasis is maintained throughout the operation, which generally is conducted within avascular planes. The internal jugular vein is reflected laterally with minimal exposure, ligating the common facial vein with a 5–0 suture before it is divided. The carotid sheath is opened longitudinally over the common carotid artery (CCA), being sure to avoid the vagus nerve if it happens to take an anomalous course anterior to the artery. In fact, the identification and preservation of several cranial nerves are cardinal features to the remainder of the dissection (see Figure 1). The distal end of a flexible loop shunt is then inserted into the ICA, retaining it with a small ring clamp. After all air is vented from the shunt, and the cul-de-sac of the CCA is filled with blood, the proximal end of the shunt is placed well into the CCA, temporarily preventing flow in the shunt by digital compression. After a proximal ring clamp has been positioned, the Hydrogrip clamp is removed by an assistant, and any potential debris is briefly flushed through the CCA around the shunt before the surgeon tightens the ring clamp and releases digital compression of the shunt. Another elastic vessel loop should be placed on slight traction around the CCA above the proximal ring clamp to prevent dislodgment of the shunt during the remainder of the procedure (see Figure 1). Any annoying backbleeding from the external carotid artery (ECA) usually can be controlled by applying a small hemostatic clip to an ascending pharyngeal branch hidden within the soft tissue of the carotid sinus. The endarterectomy is begun using a Cannon blade or a Freer elevator and entering the alabaster subadventitial plane to excise all circular fibers of the media (Figures 1 and 2). The CCA endarterectomy is terminated about 1 cm above the proximal end of the arteriotomy. After the specimen is divided at this level, it can be elevated under full vision while the endarterectomy is continued upward into the carotid bulb. A plaque extending only a short distance into the ICA may be teased medially toward the origin of the ECA to achieve an adequate endpoint. More often, it is simpler to divide the plaque in the bulb so that the ICA and ECA endarterectomies can be done independently. Once the plaque has been divided and the elastic vessel loop has been loosened around the ECA, the ECA endarterectomy is performed with slight traction on the plaque to evert the artery until an appropriate endpoint has been attained. The ECA then is gently explored with the tips of a small curved (mosquito) hemostat to remove any loose intimal fragments. If the carotid bifurcation is located unusually low in the neck and the main branchless stem of the ECA is correspondingly long, a separate arteriotomy in the ECA may also be required to complete its endarterectomy.
Technical Aspects of Conventional Carotid Endarterectomy for Atherosclerotic Disease
Surgical Technique
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Thoracic Key
Fastest Thoracic Insight Engine

