Syncope
David G. Benditt
Overview
Syncope is a syndrome characterized by the sudden loss of consciousness (including by definition loss of postural tone) of relatively limited duration with subsequent spontaneous recovery (1). The sine qua non of “true syncope” is its specific pathophysiology, namely, transient inadequacy of cerebral nutrient flow (1). This pathophysiology distinguishes syncope from other conditions that cause temporary loss of consciousness (e.g., concussion from trauma, seizures caused by electrical disturbances in the brain).
Nomenclature: What Is and What Is “Not” True Syncope
The term syncope should not be used when there is insufficient evidence that transient global cerebral hypoperfusion caused an apparent transient loss of consciousness (TLOC) episode. In such instances, it is better to use the broader descriptor TLOC. This latter designation is akin to that of syncope, but with the cerebral hypoperfusion removed. The distinctions raised here are important clinically, because TLOC keeps the physician’s “radar screen” open more widely, whereas “syncope” focuses on a narrower set of causes. Unfortunately, even the modern literature is replete with examples that fail to respect these important nomenclature issues.
Frequency
Syncope is a common medical problem, accounting for about 1% of emergency department visits and up to 6% of hospital admissions (1,2,3,4,5,6,7,8,9,10). In the clinic, however, patients do not usually use the term “syncope” but speak of “blacking or passing out,” “collapse,” or “faint.”
It has been estimated that approximately one third of individuals will experience a syncopal episode during their lifetime (9), with susceptibility to syncope increasing in association with both advancing age and increasing infirmity (9,10). Furthermore, approximately 35% of patients with syncope experience recurrences by 3 years of follow-up (9,10,11). A history of recurrent syncope at the time of initial presentation (especially if the recurrences have been spread over a relatively long period) is a strong predictor of future recurrences. In one report, more than five lifetime syncope recurrences were associated with a 50% chance of recurrence in the following year (11).
Pathophysiology
As noted earlier, syncope is defined as “a transient, self-limited loss of consciousness, usually leading to falling. The onset of syncope is relatively rapid, and the subsequent recovery is spontaneous, complete, and usually prompt. The underlying mechanism is a transient global cerebral hypoperfusion” (1).
Most true syncope events are caused by self-limited periods of arterial hypotension. Cerebral perfusion is critically dependent on systemic arterial pressure. Thus, factors that diminish systemic arterial pressure (i.e., decreased cardiac output or peripheral vascular resistance) may impair cerebral perfusion. In patients with syncope, decreased venous filling is often a major factor in triggering reduced cardiac output. Excessive pooling of blood in dependent parts of the body or diminished blood volume predisposes to systemic hypotension and syncope. Impaired cardiac output caused by other factors may also contribute to triggering faints. Thus, bradyarrhythmias or tachyarrhythmias, especially in the setting of left ventricular dysfunction, valvular heart disease, obstructive cardiomyopathies, volume depletion, or abnormal vascular reactivity (i.e., inadequate vasoconstriction or inappropriate vasodilatation), are all considerations when one is confronted with the need to establish a basis for syncope.
Inappropriate vasodilatation with inadequate venous return is the main cause of fainting in the reflex syncopal syndromes. Vasodilatation resulting in diminished cerebral perfusion also can contribute to lightheadedness and syncope in association
with thermal stress (e.g., hot environments, excessive exercise). Impaired capacity to increase vascular resistance adequately during upright posture is critical in orthostatic hypotension, whereas a similar problem may provoke syncope during or immediately after exercise or as a consequence of exposure to certain vasodilator drugs (e.g., nitrates) (12,13,14,15,16,17,18). On only rare occasions is cerebral hypoperfusion attributable to an abnormally high cerebral vascular resistance (e.g., vascular spasm such as may occur in the setting of low carbon dioxide tension).
with thermal stress (e.g., hot environments, excessive exercise). Impaired capacity to increase vascular resistance adequately during upright posture is critical in orthostatic hypotension, whereas a similar problem may provoke syncope during or immediately after exercise or as a consequence of exposure to certain vasodilator drugs (e.g., nitrates) (12,13,14,15,16,17,18). On only rare occasions is cerebral hypoperfusion attributable to an abnormally high cerebral vascular resistance (e.g., vascular spasm such as may occur in the setting of low carbon dioxide tension).
TABLE 71.1 Syncope: Diagnostic Classification | |
|---|---|
|
TABLE 71.2 Neurally Mediated Syncopal Syndromes | |
|---|---|
|
Causes of True Syncope
Causes are listed in Table 71.1.
Neurally Mediated Reflex Syncope Syndromes
The neurally mediated syncopal syndromes (Table 71.2) comprise a variety of pathophysiologically related conditions. For the most part, clinical distinctions are based on the source of the trigger for the episodes (e.g., pain, carotid sinus stimulation, cough, micturition). In this regard, the presumed triggering neural signals may arise within the central nervous system (CNS) itself (e.g., syncope associated with fear or anxiety), or from any of a number of peripheral receptors that respond to stimuli of various types (e.g., mechanical, chemical, pain). Thus, by way of example, in carotid sinus syndrome, the afferent aspect of the reflex loop is typically believed to arise from stimulation of autonomic receptors in the cervical region. However, it now seems likely that carotid sinus stimulation may need to interact with failure of parallel CNS inputs from the ipsilateral neck muscles to trigger the syndrome (19). In typical vasovagal syncope (Fig. 71.1), the location and nature of the trigger sites are usually less certain (20,21,22,23,24,25,26).
Vasovagal syncope may be triggered by any of a variety of situational factors. Some of the latter include unpleasant sights
(e.g., sight of blood), pain, and extreme emotion. Common venues for fainting are churches, hospitals, queues, and restaurants. In many but not all cases, this type of faint is easy to diagnose because a clear history of preceding dizziness together with other typical phenomena is obtained (1). The patient may reports feelings of lack of air, a change in breathing pattern, sweating, loss of hearing, and nausea before partial or total loss of consciousness. Pallor is a common physical finding in association with these faints, and witnesses to the event should be queried directly regard recollection of this finding. During the recovery phase there is rapid return of orientation. However, fatigue, weakness, nausea, and headache may last from minutes to hours. Often, in older individuals, warning symptoms may be of very brief duration or nonexistent, thereby complicating establishment of the diagnosis.
(e.g., sight of blood), pain, and extreme emotion. Common venues for fainting are churches, hospitals, queues, and restaurants. In many but not all cases, this type of faint is easy to diagnose because a clear history of preceding dizziness together with other typical phenomena is obtained (1). The patient may reports feelings of lack of air, a change in breathing pattern, sweating, loss of hearing, and nausea before partial or total loss of consciousness. Pallor is a common physical finding in association with these faints, and witnesses to the event should be queried directly regard recollection of this finding. During the recovery phase there is rapid return of orientation. However, fatigue, weakness, nausea, and headache may last from minutes to hours. Often, in older individuals, warning symptoms may be of very brief duration or nonexistent, thereby complicating establishment of the diagnosis.
When vasovagal syncope is suspected by clinical history but uncertainty remains, tilt-table testing diagnostic techniques have been of value (1,23,24,25,26,27,28,29,30,31,32,33,34,35,36). Tilt-table testing has a specificity of approximately 90% and an approximate reproducibility in the short term of 80% to 90% and in the longer term (over more than 1 year) around 60% (35). Tilt-table testing is the only investigation that provides the opportunity to precipitate a typical attack under the eyes of the investigator and allows the victim to confirm the associated symptoms.
Carotid sinus syndrome is the second most common form of the neurally mediated syncopal syndromes (1,37,38,39,40). In this setting, syncope often presents without warning (i.e., absence of premonitory symptoms). Although rare, a history suggesting that head movements trigger dizziness or syncope supports this diagnosis. As a rule, the condition almost exclusively afflicts older people, especially men.
In clinical practice, carotid sinus syndrome is often overlooked. The reasons for this include failure to perform carotid sinus massage routinely in patients with syncope and/or failure to record both blood pressure and heart rate responses when carotid massage is undertaken. Carotid massage resulting in dizziness or syncope owing to hypotension with or without bradycardia is the key diagnostic finding in patients suspected of having carotid sinus syndrome. Testing is best conducted with the patient upright on a tilt table, with continuous digital plethysmography or intraarterial pressure measurements used to record beat-to-beat arterial pressure changes (39). Firm carotid sinus massage for 5 to 10 seconds is recommended. A cardioinhibitory response is presumed to predominate when carotid sinus massage is associated with symptom reproduction in conjunction with asystole or paroxysmal atrioventricular (AV) block (37,38,39,40). However, the vasodepressor component must be assessed separately during the maneuver by beat-to-beat arterial pressure monitoring while preventing bradycardia using a temporary dual-chamber pacing system. The magnitude of this latter part of the reflex can also be estimated by examining the rate of blood pressure recovery after resumption of the native heart rate. In the absence of symptom reproduction, the demonstration of a pause of 5 seconds or longer, and/or a systolic blood pressure fall of at least 50 mmHg, is probably relevant and can be considered to support a presumptive diagnosis (1).
Among the other forms of neurally mediated reflex syncope, postmicturition syncope, swallow syncope, and cough syncope are probably the next most frequent. The medical history associated with these situational faints provides the diagnosis. The remaining conditions (Table 71.2) are only rarely encountered.
Orthostatic Syncope
Orthostatic syncope is the result of postural hypotension or orthostatic hypotension (Table 71.3). The term orthostatic intolerance has also come to be widely used as a descriptor of patients susceptible to recurring orthostatic syncope. Presyncopal or syncopal symptoms associated with abrupt assumption of upright posture are common occurrences (Table 71.3). Elderly persons, less physically fit individuals, or patients who are for whatever reason dehydrated or volume depleted are at greatest risk. Iatrogenic factors such as excessive diuresis or overly aggressive use of certain antihypertensive agents are important contributors. Environmental factors (e.g., excessive heat) and complications associated with certain medical conditions (e.g., hemorrhage) or diseases (e.g., diabetes insipidus, adrenal insufficiency) may also play a role in specific cases. Volume depletion (often iatrogenic) (27,28,41,42,43,44), exposure to vasodilator drugs, and neurologic disturbances of vascular control resulting from concomitant disease are the most frequent causes of orthostatic syncope. In certain cases, however, patients may be manifesting a form of primary autonomic failure with inadequate reflex adaptations to upright posture. The most important of the primary autonomic disturbances encountered in practice are pure autonomic failure, multisystem atrophy, and Parkinson disease with autonomic failure.
TABLE 71.3 Syncope of Orthostatic Origin: A Classification of Causes | ||
|---|---|---|
|
Specific primary autonomic nervous system dysfunctions leading to disturbances of vascular control are currently considered to be relatively infrequent causes of syncope in general medical practice. Nevertheless, as the broad spectrum of these disturbances and their potentially subtle manifestations become more widely appreciated by physicians, these diagnoses will be made more often (45,46,47,48,49,50,51). More commonly, neuropathies associated with chronic diseases (e.g., diabetes) or toxic agents (e.g., alcohol) are the source of the problem.
In a review of 155 patients referred to a center specialized in autonomic system evaluation for assessment of suspected orthostatic hypotension, Low and colleagues (48) found that among the most severely affected symptomatic patients (n = 90; mean age, 64 years), pure autonomic failure accounted for 33%, multisystem atrophy accounted for 26%, and autonomic/diabetic neuropathy accounted for 31%. The most frequently reported symptoms in these individuals were lightheadedness (88%), weakness or tiredness (72%), cognitive difficulties (47%), blurred vision (47%), tremulousness (38%), and vertigo (37%). Patients with postural orthostatic tachycardia syndrome (POTS), conversely, tended to be symptomatic during upright posture, but they did not typically manifest sufficient hypotension to result in syncope or marked hypotension.
Cardiac Arrhythmias
Primary cardiac arrhythmias as the cause of syncope encompass those rhythm disturbances associated with intrinsic cardiac disease (e.g., sinus node dysfunction [SND], AV conduction system disease), accessory conduction pathways, or other structural abnormalities (e.g., congenital anomalies, postoperative disturbances), as well as those resulting from proarrhythmic effects of cardioactive drugs (e.g., cardiac glycosides, positive inotropic agents, antiarrhythmic drugs).
Arrhythmias resulting from intrinsic conduction system disturbances (usually acquired but occasionally congenital) are important causes of syncope. However, it is often difficult to substantiate the relationship between syncope and a suspected arrhythmia in free-living individuals (e.g., by ambulatory electrocardiographic [ECG] monitoring) resulting from the unpredictable occurrence of symptomatic events. Thus, implantable long-term loop recorders (ILRs) and mobile cardiac outpatient telemetry (MCOT) are becoming more widely applied (see later). In some cases, invasive electrophysiologic testing may be indicated (52,53,54,55,56).
Sinus Node Dysfunction
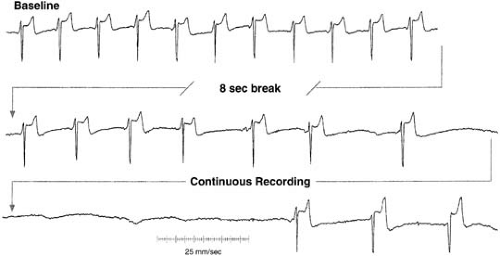
SND (also known as sick sinus syndrome, sinus node disease, and sinoatrial disease) encompasses an array of sinus node and/or atrial arrhythmias that result in persistent or intermittent periods of inappropriate slow or fast heart beating (57,58,59,60,61,62). The ECG manifestations of SND include sinus bradycardia (Fig. 71.2), sinus pauses, sinoatrial exit block, inexcitable atrium, chronotropic incompetence, and various atrial tachyarrhythmias (principally atrial fibrillation or atrial flutter). For the most part, SND is closely associated with underlying fibrosis or chamber enlargement). However, extrinsic factors (e.g., autonomic nervous system influences, cardioactive drugs) are also frequent contributors. Of these, drug-induced disturbances are the most important clinically.
In the patient with SND and syncope, the cause may be a transient severe bradyarrhythmia or tachyarrhythmia, or both. Most often, however, it is believed that the arrhythmias associated with syncope in patients with SND are those producing relatively long periods (≥10 to 15 seconds) of severe bradycardia (i.e., sinus pauses and sinoatrial block) with consequent inadequate cerebral blood flow (59,60,63,64,65).
Atrioventricular Conduction Disturbances
Although the acquired disturbances of AV conduction are most often associated with syncopal symptoms, there has been increasing concern regarding the adverse prognostic implication of syncope in congenital AV block patients (66,67,68). Drug effects also deserve special consideration because they are a particularly common, and a potentially reversible, cause of AV conduction disturbances. Antiarrhythmic drugs, cardiac glycosides, β-blockers, and calcium channel blockers are perhaps the most widely recognized in this regard. Patients with preexisting infranodal conduction system disease are at highest risk.
In general, the risk for syncope or dizziness is greatest at onset of AV block, prior to warmup of a subsidiary rhythm. Thereafter, the ventricular rhythm often stabilizes, and may average 35 to 40 beats per minute in acquired third-degree AV block. In fixed complete AV block, syncope may occur as a result of the unreliability of subsidiary pacemakers or because of the inability of the heart rate–limited circulation to provide sufficient cerebral blood flow during periods of exercise or stress.
The site of block in patients with congenital AV block is typically at the level of the AV node. Generally, the QRS complexes are narrow, and the block usually is associated with a reasonable subsidiary rhythm, which tends to increase in rate with exercise. Recently, however, concern has been raised regarding the supposedly benign natural history of congenital AV block (66,67,68), and further evaluation of this issue is needed. In the meantime, syncope and dizziness (along with exertional intolerance) are accepted indications for pacing in these patients.
Bifascicular conduction system disease is a relatively common ECG finding. However, in most cases, progression to more severe forms of AV block is slow. Susceptibility to higher-grade block (i.e., those that may be long enough to cause syncope) increases the longer the HV interval (particularly for HV intervals ≥100 milliseconds) (64,69,70,71,72) (Fig. 71.3). However, syncope in patients with evident conduction system disease may not be solely the result of bradyarrhythmias. Ventricular tachycardia (VT) is a concern in these cases owing to the usual presence of significant underlying heart disease.
Supraventricular and Ventricular Tachyarrhythmias
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree